4128
Views & Citations3128
Likes & Shares
RECOMMENDATION AND FUTURE PLAN
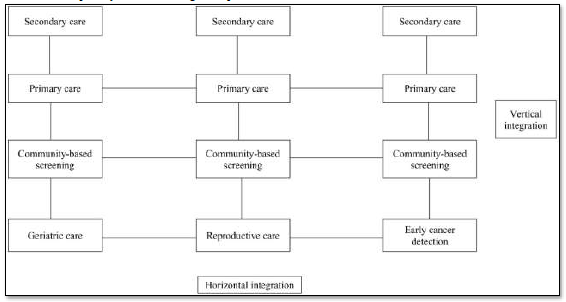
This program has proven to be acceptable, appropriate, and feasible for a community-based geriatric care program in a developing country like Sri Lanka. The above approach has cultivated community engagement which in turn helps for future scalability and sustainability. Implementing digital data systems could enhance effective data management and analysis in dropout cases. Horizontal integration of other community-based healthcare programs will support effective resource management. Such integration will enhance patient care by implementing a more unified healthcare system. Furthermore, it is recommended to do home-based care out of hours, which has demonstrated greater effectiveness in providing accessible and cost-effective care. The adoption of these strategies is likely to yield improved patient outcomes and more efficient utilization of healthcare resources. This delivery model could demonstrate an improvement in the quality of life, especially in resource-limited settings. Our plan is focused on implementing a vertical and horizontal integration model, aimed at enhancing sustainability and cost-effectiveness in healthcare delivery. This process allows us to identify patients who are then referred to the Family Health Centre in Kondavil from community centers for further assessment and care. Depending on their medical needs, patients may receive additional referrals, those with general medical issues will consult with a General Physician, while the VOG addresses reproductive health concerns for those who are detected from early-stage cancer detection, patients are referred to Consultant oncological surgeon [5-8]. Our future strategy encompasses horizontal integration, where community health workers shall be utilized for additional roles especially cancer screening and reproductive health management for better resource management. Rather than assigning distinct staff for each project, we plan to deploy the same set of workers for diverse responsibilities, including community-based screening and duties at institutional-based clinics. This method not only centralizes our efforts but also optimizes the utilization of our human resources [9]. An integral part of this plan is staffing efficiency and compensation. By employing an integrated model, we aim to reduce the overall headcount, thereby ensuring competitive salaries for the staff. Moreover, we plan to offer out-of-hours home-based care, with our staff receiving overtime payments. For example, suppose two out of three community health workers provide home care from 4 PM to 7 PM. In that case, they will be compensated at an overtime. This approach, which combines overtime with regular salaries, is designed to ensure a fair and satisfactory income for our staff, as opposed to the less favorable financial conditions under a system with a separate staff for each service category.
ACKNOWLEDGEMENT
This community-based program was funded by old boys’ association of St Johns college Jaffna Sri Lanka.
- The National Policy and Strategic framework for Prevention and Control of Chronic Non-Communicable Diseases in Sri Lanka (2023-2033) Ministry of Health Sri Lanka. Available online at: www.documents.gov.lk
- Ssensamba JT, Nakafeero M, Musana H, Amollo M, Ssennyonjo A, et al. (2022) Primary care provider notions on instituting community-based geriatric support in Uganda. BMC Geriatr 22(1): 1-8.
- Primary Care-Frailty Science (2024) Available online at: https://frailtyscience.org/clinical-topics/primary-care/
- Connor E, Mullan F (1983) Community Oriented Primary Care: Meaning and Scope. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK234632/
- WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention. Available online at: https://www.who.int/publications/i/item/9789240030824
- Cancer Screening Guidelines (2024). Available online at: https://www.cancer.org/cancer/screening/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html
- Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, et al. (2020) Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin 70(5): 321-346.
- Smith RA, Andrews KS, Brooks D, Fedewa SA, Saslow D, et al. (2019) Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 69(3): 184-210.
- Integrated care for older people: Guidelines on community-level interventions to manage declines in intrinsic capacity. Available online at: https://www.who.int/publications/i/item/9789241550109
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Pathology and Toxicology Research
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)



