1745
Views & Citations745
Likes & Shares
The study aimed to assess the risk factors and prevalence of low birth weight among births attended at Kibogora Level 2 Teaching Hospital in Nyamasheke. Low birth weight remains a significant contributor to child morbidity and mortality, with long-term implications for adult health. Adopting a prospective study with a quantitative approach, primary data were collected from 45 women. The study revealed a prevalence of 15.6% of low birth weight among births attended at Kibogora Level 2 Teaching Hospital. Data analysis was conducted using the Statistical Package for Social Sciences (SPSS) software, version 16. These findings underscore the importance of continued efforts to address risk factors and improve outcomes for newborns, highlighting the need for targeted interventions to mitigate the impact of low birth weight on public health.
The issue of low birth weight (LBW) is a significant public health challenge in low- and middle-income countries [1,2].
Globally, over 20 million newborns, estimated at 15%-20%, are born with low birth weight, with 13% of these cases occurring in sub-Saharan Africa [3,4]. The World Health Organization estimates the incidence of low birth weight (LBW) to be 15.5%. Approximately 25 million babies with low birth weight are born annually, with nearly 95% of them in developing countries [5]. Infants are at a heightened risk of mortality during their initial month, and those who survive often encounter enduring consequences. These may encompass increased susceptibility to stunted growth, diminished intelligence quotient (IQ), and the development of chronic conditions in adulthood, such as obesity, hypertension, and diabetes mellitus [6,7]. Low birth weight is defined as a weight below 2500g at birth, regardless of gestational age. A weight between 1000g and 1499g is categorized as very low birth weight, while a weight of 999g and below is classified as extremely low birth weight [3,6]. LBW births continue to be prevalent, especially in low- and middle-income countries (LMICs), where an estimated 10%-20% of newborns meet the LBW criteria [8,9].
Despite numerous interventions aimed at controlling LBW births, their prevalence is on the rise and remains a significant challenge. According to a 2013 report from the United Nations Children’s Fund, an estimated 22 million infants were born weighing less than 2500 grams, with a global incidence of around 16%. Sadly, most of these infants did not survive beyond the neonatal period. Worldwide, 20 million neonates with LBW are born annually, with 92% originating from developing countries, predominantly in Asia (70%) and Africa (22%). A study conducted in Kenya and neighboring East African countries revealed a LBW prevalence of 12.3% [10]. In northern Tanzania, the prevalence of LBW was reported to be 10.6% [11]. According to the most recent national antenatal care guidelines from 2020, the incidence of LBW is noted as 7%, showing a gradual increase from 6% reported in the Demographic and Health Survey (DHS) of 2014-2015 [10]. Worldwide, LBW is linked with a range of maternal and obstetric factors, including malnutrition and inadequate weight gain, infections such as malaria and HIV, prepartum hemorrhage, chronic hypertension and hypertensive disorders of pregnancy, diabetes, abnormal placentation, multiple pregnancy, and preterm birth [12]. Certain factors, like those you've mentioned, can be altered through early and thorough prenatal care. In Rwanda, however, only 47% of individuals managed to complete the four recommended antenatal care visits as per the Rwanda Demographic Health Survey (RDH) from 2015 to 2020. Additionally, socioeconomic factors, including education, income, inequality, and access to prenatal care, play crucial roles in determining pregnancy outcomes and birth weight [12]. In Rwanda, children born in rural areas tend to have lower birth weights compared to those born in urban areas. Additionally, mothers who attended secondary or high school education or belong to the highest wealth quintile are less likely to deliver LBW babies. The rate of LBW varies from 4% to 8% in regions such as Kigali and the South Province of Rwanda [10].
PROBLEM STATEMENT
Despite efforts within the health sector to manage LBW newborns, their care remains complex, leading to higher mortality rates compared to newborns with normal weight [6]. LBW is widely regarded as the single most significant predictor of infant mortality, particularly deaths occurring within the first months of life [5]. Additionally, LBW serves as a significant determinant of infant and childhood morbidity, particularly influencing neurodevelopmental impairments such as mental retardation and learning disabilities. Half of all perinatal and one-third of all infant deaths are directly or indirectly linked to LBW. Mortality rates among LBW babies are 40 times higher than those among normal-weight babies. Moreover, infants born with very low weight are over 100 times more likely to succumb within the first year of life compared to infants of normal birth weight [13]. The recent prevalence of LBW in Rwanda has shown a slight increase to 7%, up by 1% according to the latest Rwanda Demographic and Health Survey. Despite efforts, the under-5 mortality rate has continued to decline from 50 deaths per 1,000 live births in the 2014-15 RDHS to 45 deaths per 1,000 live births in the present survey. However, the decline in childhood mortality rates has slowed down and eventually stagnated among newborns and infants. After dropping from 50 deaths per 1,000 live births to 32 deaths per 1,000 live births, the overall infant mortality rate has remained practically unchanged in the most recent 5-year period. This is mainly due to neonatal mortality and post-neonatal mortality staying at almost the same level, with 20 deaths per 1,000 live births between 2019-2020, compared to 19 deaths per 1,000 live births previously. Despite efforts to improve maternal and newborn health, the infant mortality rate in Rwanda remains stubbornly high at 33 deaths per 1,000 births, up from 32 deaths per 1,000 live births [14].
The Rwandan four-yearly Summary Report of Maternal and Newborn Deaths highlighted that 61% of neonatal mortality cases involved LBW newborns. This underscores the significance of LBW as a concern for the Rwandan health sector, particularly for healthcare professionals who specialize in working with children [15].
The management of LBW poses significant challenges in any country, but it becomes even more daunting in developing nations like Rwanda. Various complex factors contribute to and complicate the care of LBW newborns, including chronic family poverty leading to food insecurity, a shortage of qualified healthcare providers, inadequate equipment at health facilities, and a lack of prospects for pregnant women, which may result in feelings of hopelessness [5]. The Western province, in particular, faces a high unmet need for family planning compared to other parts of the country, exacerbating the issue of pregnant women's lack of prosperity. Additionally, Nyamasheke, continues to experience chronic poverty more than any other part of the country, which may increase the association with maternal biomedical, demographic, and socioeconomic factors related to LBW. The purpose of this study was to determine the prevalence of low birth weight and associated risk factors among births attended in Kibogora level 2 teaching Hospital.
METHODOLOGY
The research methodology for this study, conducted at Kibogora Level Teaching Hospital, involved gathering data from women who gave birth at the hospital between June 13th and 17th, 2022, and provided consent. A sample of 45 neonates was recruited over a 5-day period using the Yamane formula, selected from the entire population of neonates born during the study period. A data collection form, developed based on relevant literature, was utilized to collect information on study variables. Prior to data collection, the form underwent validation and reliability testing to ensure its accuracy and consistency. Ethical considerations were prioritized, with informed consent obtained from participants, and measures implemented to uphold confidentiality. Data analysis employed appropriate statistical methods to ascertain the prevalence of low birth weight and associated risk factors. In summary, the methodology aimed to acquire reliable data while adhering to ethical guidelines and maintaining participant confidentiality. This chapter presents the data collected, the results of the statistical analysis conducted, and the interpretation of findings. A total of 45 newborns/postnatal women were recruited into the study to assess the prevalence of low birth weight and their associated risk factors among births attended at Kibogora Hospital. A questionnaire was utilized to gather information from individuals who willingly agreed to participate. Data entry was performed using a computer, and the Statistical Package for Social Sciences (SPSS) software, version 16, was employed for analysis. The results were presented using descriptive statistics in the form of tables.
PRESENTATION OF FINDINGS AND DISCUSSIONS
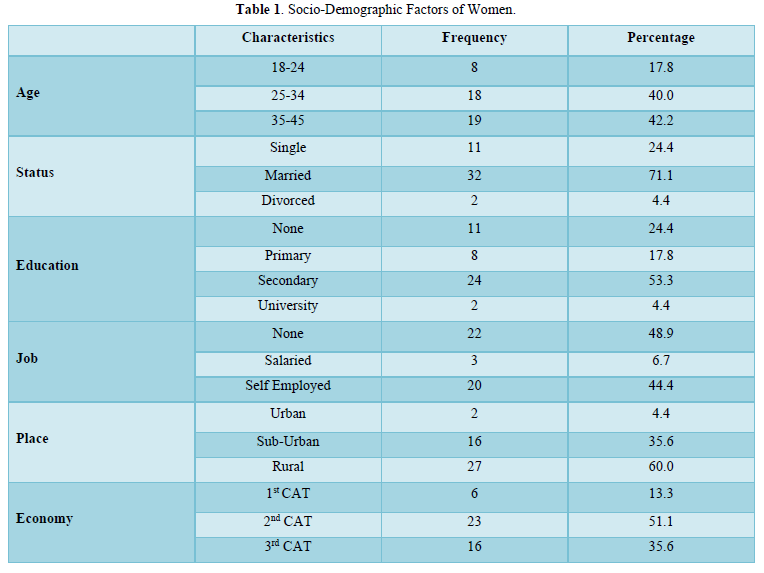
Socio-Demograhic Characteristics of Womens
Table 1 shows the social demographic characteristics of the respondents (postnatal women). Based on the age the most respondents were in range of 35 to 45 19(42.2) followed by 25 to 34 18(40.0), followed by 18-24 8(17.8). Based on marital status the most respondents were married 32 (71.1) followed by single 11(24.4) and the last 2(4.4) were divorced. Based on education the most respondents reached in secondary school 24(53.3), followed by 11(24.4) that didn’t study, followed by 8(17.8) who did primary education and lastly 2(4.4) did university. Based on job, the most respondents had no job 22(48.9) followed by self-employed 20(44.4) and lastly 3(6.7) who were salaried. Based on place the most respondents were living in rural area 27(60.0) followed by 16(35.6) that lives in sub-urban and lastly 2(4.4) that lived in urban. Based on the economy most of the respondents were in second category 23(51.1) followed by third category 16(35.6) and lastly 6(13.3) that were in first category of UBUDEHE.
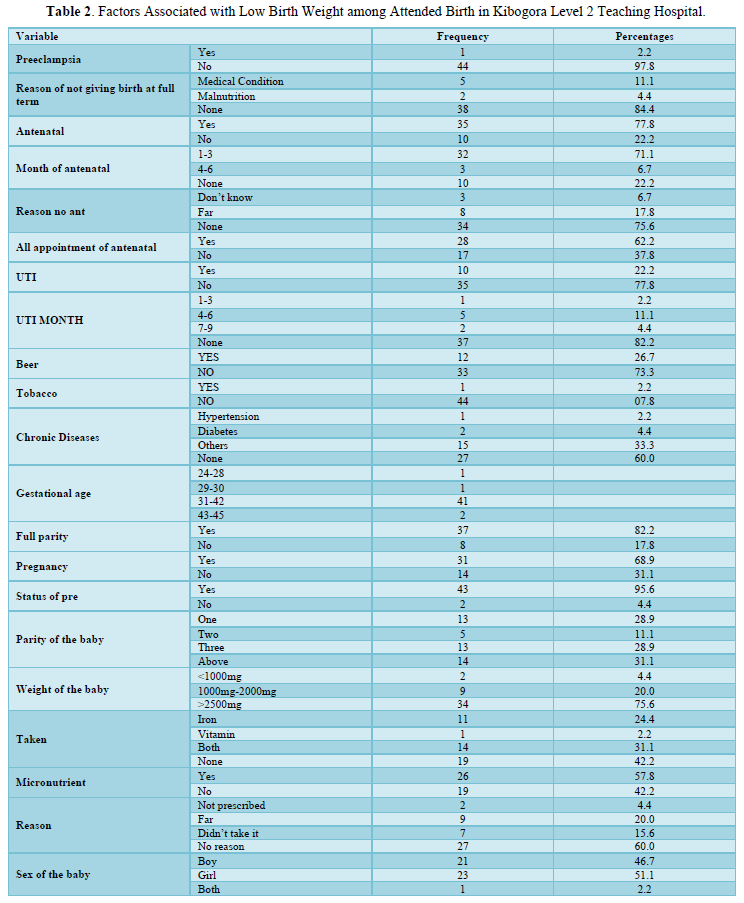
Factors Associated with Low birth Weight Among Attended Birth in Kibogora Hospital.
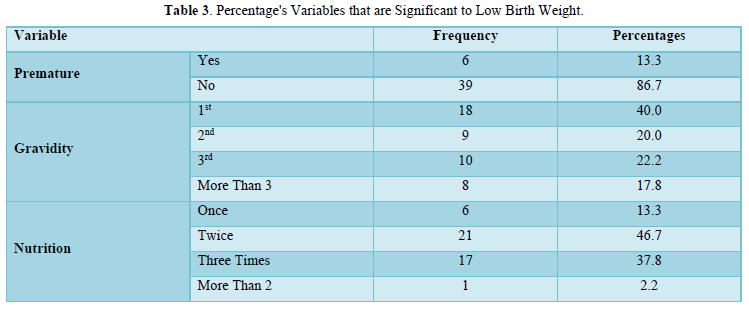
In this data analysis, Table 2 shows that Preeclampsia, ante natal care, medical conditions (chronic diseases), gestational age, full parity, pregnancy status and parity of the baby had a p value above 0.005 and that shows that it was not significantly related to LBW. SPSS was used to further investigate the variables in Table 3 and the results indicated that premature, gravity and nutrition are significantly related to LBW.
Highlights
Prevalence of low birth weight is 15.6% significant risk factors identified for low birth weight include nutrition, gravidity, prematurity, urinary tract infection (UTI) during pregnancies, and education.
The Prevalence of Low Birth Weight
The study revealed that the prevalence of low birth weight among attended birth in Kibogora level 2 teaching Hospital was 7(15.6) among the total of 45 newborns/mother (Table 4).
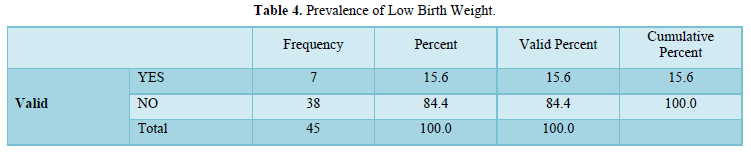
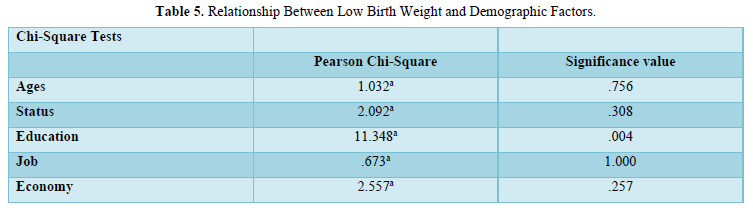
Table 5 shows the relationship between low birth weight and socio-demographic factors. Where it summarizes how socio-demographic factors relates to low birth weight. A chi square test was used to test between the two variables. The chi square test shows that there was no scientifically significant association age and low birth weight. At chi square of 1.032a and significance value of 0.756 while education is significantly proven to have an association with a chi square of 11.348a and p value that is less than 0.005 which is 0.004.
Association Between Variables
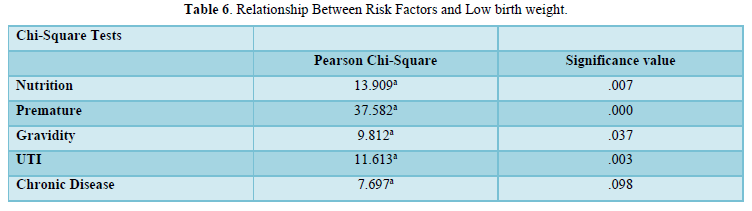
It summarizes how the below risk factors are significantly associated to low birth weight (Table 6). Chi square test was used to test the dependent and independent variables. The chi square test shows that chronic diseases is not significantly associated with low birth weight with a chi square of 7.697a and p value of .098. while nutrition is significantly associated to low birth weight. At the chi square of 13.909a and significance value of 0.007 that is less that p value of 0.005. Premature has a chi square of 37.582a and p value of .000, gravidity had a chi square of 9.812a and p value of .037 and lastly UTI has a chi square of 11.613a and p value of .003.
DISCUSSION OF FINDINGS
The study found that 15.6% of newborns had low birth weight, a figure lower than the 2020 study in Kisumu, Kenya, but higher than the 12.8% reported in Gakoma, Rwanda [10]. Socio-demographic factors were linked to low birth weight, with maternal age showing no significant impact, consistent with the Gakoma study [10]. Education emerged as a significant factor, with lower educational levels associated with higher incidences of low birth weight, mirroring findings from Dhaka, Bangladesh. Marital status, occupation, and economic status, however, did not show significant correlations. Nutrition was another critical factor, with inadequate nutritional advice during pregnancy significantly increasing the risk of low birth weight, aligning with results from Nekemte town, West Ethiopia. Medical conditions such as preterm birth, gravidity, and urinary tract infections were also significant contributors [16]. Preterm birth had a notably high correlation, and although chronic diseases were not statistically significant, they were still considered relevant. These findings underscore the importance of addressing both socio-demographic and medical factors to reduce low birth weight prevalence and enhance maternal and neonatal health outcomes. Prioritizing education, providing adequate nutritional guidance, and managing medical conditions effectively during pregnancy are essential strategies for improving birth outcomes.
CONCLUSION
In conclusion, this study sheds light on the prevalence of low birth weight among births attended at Kibogora Hospital, which was found to be 15.6%. The significant risk factors identified include nutrition, gravidity, prematurity, urinary tract infection (UTI), and education. These findings underscore the importance of focusing on these factors in prevention and intervention efforts aimed at reducing the prevalence of low birth weight in the community. By addressing issues related to maternal nutrition, providing adequate prenatal care to reduce the risk of preterm birth, and promoting education among expectant mothers, healthcare professionals can play a vital role in improving maternal and neonatal health outcomes and ultimately reducing the burden of low birth weight in the community.
- Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, et al. (2013) National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health 1(1): e26-36.
- Id Lumbani T, Dzikiti L, Hajison P, Feresu S (2019) Maternal factors contributing to low birth weight deliveries in Tshwane District, South Africa. PLoS One 14(3): e0213058.
- UNICEF- WHO (2015) Low Birthweight Estimates
- Asia S (2012) Low Birth Weight Policy Brief. pp: 1-8.
- Gebregzabiherher Y, Haftu A, Weldemariam S, Gebrehiwet H (2017a) The Prevalence and Risk Factors for Low Birth Weight among Term Newborns in Adwa General Hospital, Northern Ethiopia. 2017 Article ID 2149156, pp: 1-7.
- Sema A, Tesfaye F, Belay Y, Amsalu B, Bekele D, et al. (2019) Associated Factors with Low Birth Weight in Dire Dawa City, Eastern Ethiopia: A Cross-Sectional Study. 2019:
- Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, et al. (2016) Low birth weight leads to obesity, diabetes and increased leptin levels in adults: The CoLaus study. Cardiovasc Diabetol 15: 73.
- Health LG (2013) Supplementary appendix.
- UNICEF-WHO (2004) Global Estimates.
- Nzayisenga PJ, Emmanuel N, Connie M, Michael H (2021) Prevalence and factors associated with low birth weight among neonates in Rwanda: A prospective cross-sectional study. Life Res 4(2): 16.
- Mitao M, Philemon R, Obure J, Mmbaga BT, Msuya S, et al. (2016) Risk factors and adverse perinatal outcome associated with low birth weight in Northern Tanzania: A registry-based retrospective cohort study. Asian Pac J Reprod 5(1): 75-79.
- Chibwesha CJ, Zanolini A, Smid M, Vwalika B, Kasaro P, et al. (2017) Predictors and outcomes of low birth weight in Lusaka, Zambia. Int J Gynaecol Obstet 134(3): 309-314.
- Gebregzabiherher Y, Haftu A, Weldemariam S, Gebrehiwet H (2017b) The Prevalence and Risk Factors for Low Birth Weight among Term Newborns in Adwa General Hospital, Northern Ethiopia. Obstet Gynecol Int 2017:
- RDHS 2014-2015 (2016) Rwanda Demographic and health survey report 2014-2015.
- Khurmi MS, Sayinzoga F, Berhe A (2017) Newborn Survival Case Study in Rwanda - Bottleneck Analysis and Projections in Key Maternal and Child Mortality Rates Using Lives Saved Tool (LiST) 6(2): 93-108.
- Habak PJ, Carlson K, Robert P Griggs Jr (2024) Urinary Tract Infection in Pregnancy.
- Bian Y, Zhang Z, Liu Q, Wu D, Wang S (2013) Maternal risk factors for low birth weight for term births in a developed region in China: A hospital - based study of 55,633 pregnancies. J Biomed Res 27(1): 14-22.
- The DHS Program (2011) Ethiopia Demographic and Health Survey Preliminary Report.
- Minuci EG (2009) Diferenciais intra-urbanos de peso ao nascer no município de São Paulo Birth weight intra-urban differentials in the city of São Paulo. 43(2): 256-266.
- Ruwanpathirana T, Fernando DN, Senanayake H (2013) Development of birth weight for gestational age charts in a Sri Lankan setting-methodological issues. 2: 47-51.
- Tegegne KT, Assefa AA, Zenebe A, Bagajjo WS, Rike M, et al. (2022) Effect of Anemia on Birth Weight Among Pregnant Women Attending Anc Clinic at Public Hospitals of Sidama Region, Ethiopia 2022 A Prospective Cohort Study Protocol. J Clin Cases Rep 10: 16-30.
- WHO (2011a) Sixty-Fourth World Health Assembly. pp: 16-24.
- WHO (2011b) Guidelines on Optimal feeding of low birth-weight infants in low-and middle-income countries.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)


