4782
Views & Citations3782
Likes & Shares
Study design: Cross sectional observational analytical study. All pregnant women in second and third trimester with singleton pregnancy, attending the Antenatal Clinic of Sparsh hospital without any other complain, included in this study.
Machine: GE Voluson P8 Usg machine was used for scanning of patients. volume probe was used.
Measurement done in 2D, during rest, contraction and Valsalva manoeuvre are
- Distance between bladder neck and imaginary line between posterior inferior surface of pubis symphysis and Ano rectal angle.
- Measurement done in 3D during rest, contraction and Valsalva manoeuvre
- Distance between urethra and lateral midpoint of levator ani muscle, right and left side.
- Distance between urethra and post fourchette.
- Thickness of levator ani muscle.
- Hiatus area.
Result: This study shows that changes in pelvic floor started during pregnancy as the gestational age increases, changes enhanced, due to the weight of gravid uterus which causes stretching of pelvic floor musculature and neurovascular structures. hormones of pregnancy also relax the ligaments of pelvis. As the parity increases bladder neck mobility increases .in second gravida patients changes in levator ani thickness and hiatal area is not statistically significant.
Conclusion: Trans labial USG is a non-invasive easily available inexpensive and well accepted by pregnant women .it dynamically evaluate the pelvic floor anatomy and changes during contraction and Valsalva manoeuvre. Quantitative analysis can be easily done during scanning. changes can be shown to the patient during scanning, so that patient and her health care adviser can take proper care of pelvic floor after delivery with in time.
Keywords: USG, Trans labial USG, Pelvic floor defects, Bladder neck mobility
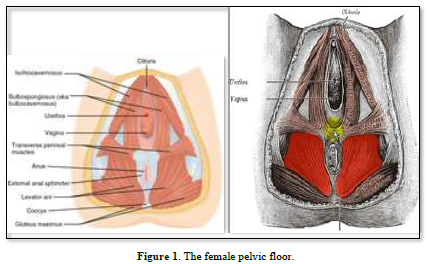
Function of pelvic floor is support to pelvic organs. damage to pelvic floor led to pelvic floor disorders. Pregnancy and child birth are transformative experiences for a woman’s body. damage to pelvic floor during pregnancy and child birth can lead to urinary incontinence, fecal incontinence and pelvic organ prolapse. trauma to the neurovascular element of pelvic floor led to pain with or without sexual function.
Weight of women increase during pregnancy, increase weight of pregnant uterus stretches pelvic floor muscles more and neuro vascular supply of pelvic floor is also affected by this pressure. Relaxin hormone secreted from placenta, increases the flexibility of ligaments in pelvis and soften the pelvis. connection between bones and tissue loosen resulting in increased flexibility and instability.
Labor and delivery are the most important risk factor for pelvic floor disorders. vaginal delivery especially first vaginal delivery causes maximum damage to pelvic floor. maximum stress is offered to pelvic floor muscles during second stage of labor when there is active pushing. this damage is increased with operative vaginal deliveries using vacuum or forceps.
Pelvic floor disorders are not easily recognizable, as symptoms can mimic other condition. pain may be confused for endometriosis.
Changes during pregnancy in pelvic floor can easily be assessed by Ultrasonography. this is inexpensive. easily available and reproducible technique. Trans labial 2Dand 3D USG is very effective method to demonstrate the changes in the pelvic floor during pregnancy to women and sensitize them regarding the problem to be faced due to these changes in future and trained them and their health workers for precaution to be taken during delivery to minimize the damage and post-delivery care of pelvic floor. Changes in hiatal area during pregnancy can help to decide which patient can have smooth normal vaginal delivery and which patient can have difficulty during labor so appropriate decision can be taken before hand.
MATERIAL AND METHOD
Objective: To study the changes in pelvic floor during pregnancy by trans labial USG.
Study design: Cross sectional observational analytical study
Inclusion criteria
- All pregnant women in second and third trimester with singleton pregnancy, attending the Antenatal Clinic of Sparsh hospital without any other complain, included in this study. Duration of study was from December 2022 to July 2023
- Study was approved by Sparsh Hospital’s ethical committee
- 112 patients recruited for study, after explaining everything regarding study and written consent taken by every patient before USG examination of pelvic floor
- Age of patients 21-to-35-year, average age of patients 32.5 years
- BMI average 28
Exclusion criteria
- Patient with history of pelvic floor surgery
- History of neuromuscular disorder
- History of smoking
- Any pelvic organ tumor
- Hormonal intake
- Chronic constipation, chronic cough or any other medical disorder
- History of SUI
Control Group
- Nulliparous patients who attended gynae OPD for any other gynecological problem
- Age between 21 to 30 years
- No h/o any hormonal intake
- No complain of POP and SUI
- No history of chronic cough or constipation
- Average age of patient - 28 yrs.
- Average BMI 25
25 primi patients included in second trimester group, 25 primi patients in third trimester group, 25 second gravida patients in second trimester group, 25 second gravida patients in third trimester group and 12 patients in nulliparous group. Total 112 patients.
Machine
Machine used for scanning of patients was GE VOLUSON P8 2 D and 4 D (volume probe) probe was used.
Scanning of patient done by a clinician with experience of more than 20 years after voiding urine patient lie down with knee flexed and heel close to the buttock only 30 to 50 ml urine in bladder was allowed during examination first patient was explained about the procedure then measurements was taken during rest, contraction and Valsalva manoeuvre patient was asked to hold breath for 10 to 15 sec for effective Valsalva manoeuvre.in this manoeuvre all the pelvic organs moves towards the imaginary line between the posterior surface of pubis symphysis to anorectal line area of hiatus is increased during contraction all the organs moves away from imaginary line towards the pubic symphysis for effective contraction patient asked to contract the anus and vagina.
During examination probe is covered by disposable transparent probe cover. new cover is used for each patient.
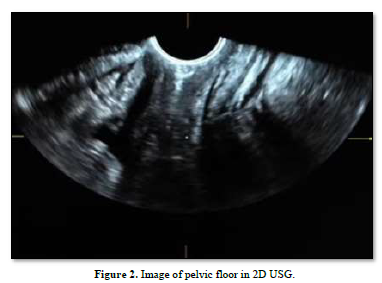
Measurement done in 2D, during rest, contraction and Valsalva manoeuvre are (Figure 2):
- Distance between posteroinferior surface of pubis symphysis and anorectal angle
- Distance between bladder neck and imaginary line between posterior inferior surface of pubis symphysis and Ano rectal angle.
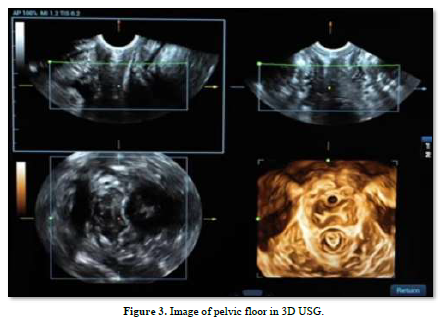
Measurement done in 3D during rest, contraction and Valsalva manoeuvre (Figure 3):
- Distance between urethra and lateral midpoint of levator ani muscle, right and left side
- Distance between urethra and post fourchette
- Thickness of levator ani muscle
- Hiatus area
RESULT
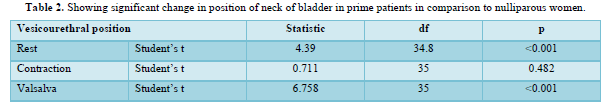
Table 1 showing descriptive analysis of vesicourethral distance from imaginary line between post surface of pubis symphysis and anorectal angle.
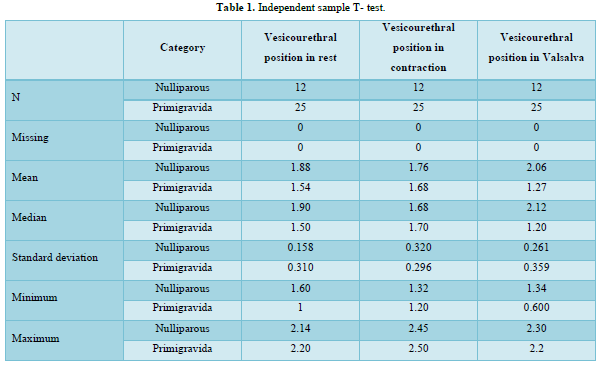
This result shows that there is significant change in position of neck of bladder in prime patients in comparison to nulliparous women. This change in position is statistically significant in rest and Valsalva, p value is (Table 2).
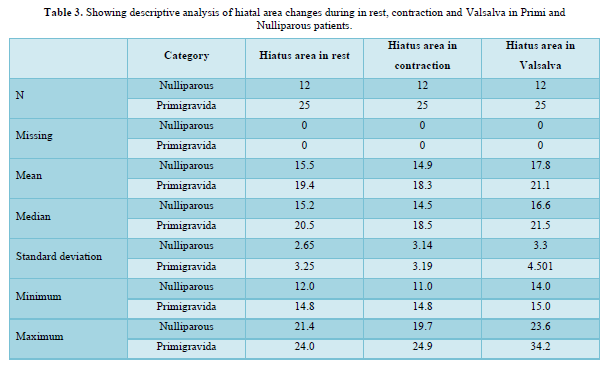
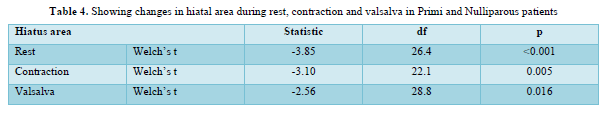
Analysis of Tables 3 & 4 is showing that in primi patient during pregnancy area of hiatus is changed during rest, contraction and Valsalva procedure. these changes are statistically significant. these changes are due to pressure exerted by gravid uterus on levator ani muscle, which causes excessive starching and hypertrophy of muscle. These changes are more prominent during late third trimester.
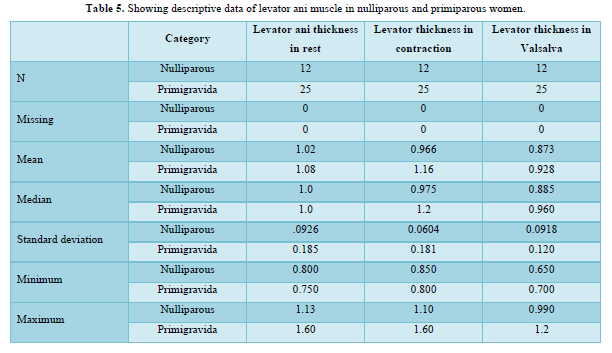
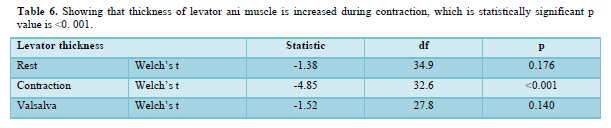
These result shows that thickness of levator ani muscle is increased during contraction, which is statistically significant p value is (Tables 5 & 6).
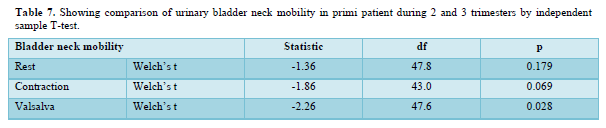
Bladder neck mobility is changed in rest, in contraction and Valsalva in third trimester in primi patients but statistically significant change in Valsalva manoeuvre, p value is 0.028. this shows as the gestational age increases, changes in Para vesical and para urethral tissues are more due to stretching and hormonal effect (Table 7).
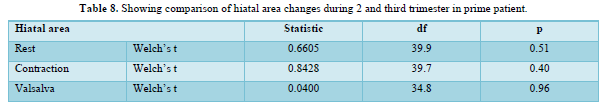
Changes in hiatal area during rest, contraction and Valsalva are not significant between 2 and third trimester in primi patient (Table 8).
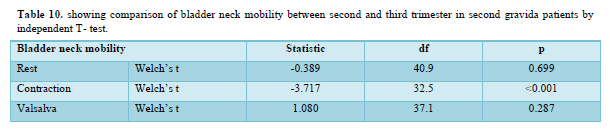
Bladder neck mobility is more in 3rd trimester as compared to 2 trimesters in second gravida. these changes are statistically significant during contraction (Table 10).
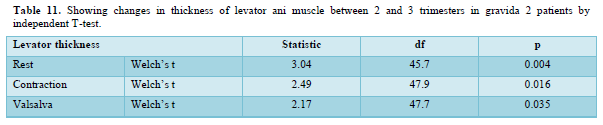
Thickness of levator muscle is decreased in third trimester as compared to 2 trimesters in rest, contraction and Valsalva, which is statistically significant. p value is given in Table 11.
Hiatal area is slightly increased in 3 trimesters as compared to 2 trimesters in gravida 2 patients but this is not statically significant.
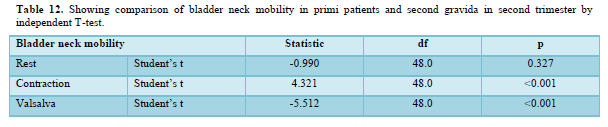
Bladder neck mobility is more in second gravida patients as compared to primi patients. This is statistically significant in contraction and Valsalva. this may be due to incomplete damage repair of previous pregnancy. Damaged caused by vaginal delivery is not healed completely with time (Table 12).
Changes in hiatal area and thickness of levator ani muscle in rest, contraction and Valsalva are not statistically significant in second trimester between prime and second gravida patients.
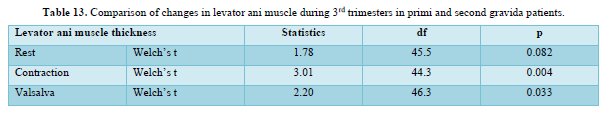
Changes in levator ani muscle is statistically significant during contraction and Valsalva in third trimester between primi and second gravida patients.
There are no statistically significant changes in bladder neck mobility and hiatal area in 3rd trimester between primi and second gravida patients.
DISCUSSION
In this study we compare the ultrasound measurement of pelvic floor in 3 different group, nulliparous, primi patient with singleton pregnancy and women with second singleton pregnancy .in this study we tried to find out effect of first singleton pregnancy on pelvic floor anatomy and effect on Para vesical and para urethral supporting tissues. we compare the changes in pelvic floor due to pregnancy in first singleton pregnancy and second singleton pregnancy. we found that there is increased bladder neck mobility in second gravida patients in contraction and Valsalva, which is statistically significant. Changes in hiatal area and thickness of levator muscle is not significant.
There are no statistically significant changes in hiatal area and bladder neck mobility in third trimester in first and second gravida patients. levator ani changes are statistically significant in 3rd trimester in both these group, during contraction and Valsalva. Hans Peter Dietz, study found no significant differences between women with one, two or three and more caesarean births in any clinical or sonographic parameters of pelvic organ support and pelvic floor muscle function [4]. Dan Luo’s study showed that multiparous women experienced more obvious symptoms and pelvic floor structure changes during pregnancy as compared to nulliparous patients [5]. This is also shown in our study that multiparous women shows much more changes in pelvic floor anatomy during their pregnancy as compared to nulliparous women .urinary complains are more in second gravida patients as compared to first gravida and nulliparous women due to increased bladder neck mobility in these patients during their pregnancy period in second as well as in third trimester .this indicate that increase no of pregnancy causes more changes in pelvic organ support and pelvic floor muscle function. This aspect needs more research to support.
Result of this study shows, significant change in bladder neck position in prime patients as compared to nulliparous patients. this change is statistically significant during rest and Valsalva. change in hiatal is also significant during rest and Valsalva. Thickness of levator ani muscle is increased in prime patient. change is statically significant during contraction.
Incidences of pelvic floor defects ranges from 10-58% [6]. Pregnancy and child birth are considered to be independent high-risk factors [7,8]. Weight of the baby increases gradually and exert pressure on surrounding structures, especially in third trimester there is excessive pressure on surrounding structure. this causes damage to adjacent neurovascular structures. Hormonal changes during pregnancy and delivery cause pelvic floor structures changes [9]. Further damage with subsequent pregnancy and delivery, pelvic floor tissue adopts to this change through a series of remodeling processes [10]. When changes caused by pregnancy and delivery not healed with time then POP and SUI will be experienced by women, affecting the social life of patient. also affect the mental and physical health of patients [11,12].
levator ani muscle is unique, differ from other skeleton muscles, it maintains a constant tone, except during voiding, defecation and the Valsalva manoeuvre [13]. LAM contract quickly with sudden increase in intra-abdominal pressure during sneezing or coughing [14-16]. This property of muscle minimizes the risk of SUI and POP [17,18]. LAM starches during delivery beyond its limits approximately 3.3 time in order to allow passage of the term infant. First vaginal delivery causes maximum damage to LAM and pelvic floor, this led to decreased pelvic floor muscle strength, enlarge vaginal hiatus and pelvic organ prolapse in future, if injures not healed properly after delivery. pregnancy and delivery cause some permanent changes in pelvic floor morphologically and function of LAM. larger vaginal hiatus indicate s a weaker pelvic floor support structure, that will be more prone to POP [19].
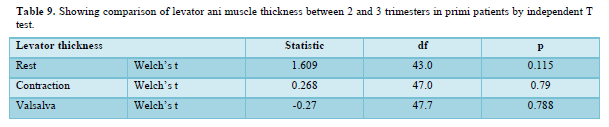
In our studies there is no statistically significant changes in pelvic floor findings between second and third trimester, in prime patients. mobility of bladder neck is more in third trimester as compared to second trimesters in prime patients. No significant change in LAM in third trimester as compared to second trimester.
Bladder neck mobility is more in third trimester as compared to second trimester in second gravida patients. this change is statistically significant during contraction. changes in lam morphology are significant in third trimester as compared to second trimester in second gravida patients.
There is no significant difference between the women with a second singleton pregnancy group and the women with the first singleton pregnancy in hiatal area, which was consistent with a previous study.
Result of our studies shoes that there is increased mobility of bladder neck in primi and second gravida patients compared to nulliparous patents, which is statistically significant. changes in hiatal area are also significant in prim patient group patients as compared to nulliparous patients.
This study provides the basic information regarding the changes in pelvic floor in first singleton and in second singleton pregnancy in Indian women. which is of clinical significance to anticipate the problems to be faced by the women after delivery, so that she can take proper care of her pelvic floor after delivery.
CONCLUSIONS
Result of this study shows that pelvic floor changes begin during pregnancy and some changes progress as the gestational age progresses. there are significant increase in mobility of bladder neck, decent in bladder neck, anorectal junction and enlargement of hiatal area. there are no significant changes in hiatal area with increase in no of pregnancy. bladder neck mobility is increased with increase in parity. professor Dietz first applied 3 D ultrasound to the observation of pelvic floor tissue. USG become the preferred imaging examination method for diagnosis of pelvic floor disorders in female strans labial USG is a non-invasive easily available inexpensive and well accepted by pregnant women .it dynamically evaluate the pelvic floor anatomy and changes during contraction and Valsalva manoeuvre. Quantitative analysis can be easily done during scanning. changes can be shown to the patient during scanning, so that patient and her health care adviser can take proper care of pelvic floor after delivery with in time.
More studies with large sample size are required to support these findings.
LIMITATION
Sample size is small. We have not taken patient who had first and second LSCS delivery. same patient is not followed in second and third trimester. Same patient is not taken for first and second pregnancy. All the patients were Indian so our result may not apply to other ethnic groups.
KEY POINTS
- FPFD is a common gynecological disorder.
- Trans labial USG is easily available well accepted means of the diagnosis of FPFD.
- First pregnancy causes more changes in pelvic floor anatomy and increase in hiatal area.
- With increase in parity hiatal area does not change much.
- With increase in parity bladder neck mobility changes and bladder neck descend down wards.
- Bruno B, Kavin S, Stephen WL (2023) Anatomy, Abdomen and Pelvis, Pelvic Floor, StatPearls, Treasure Island (FL).
- Fernandes ACNL, Palacios-Ceña D, Hay-Smith J, Pena CC, Sidou MF, et al. (2021) Women report sustained benefits from attending group-based education about pelvic floor muscles: A longitudinal qualitative study. J Physiother 67(3): 210-216.
- Mélanie R, Nathaly G, Marie-Pierre C, Gabriel V, Nathalie BJ, et al. (2021) The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review. Life 11(9): 900.
- Dietz HP, Scoti F, Subramaniam N, Friedman T, Shek KL (2018) Impact of subsequent pregnancies on pelvic floor functional anatomy. Int Urogynecol J 29: 1517-1522.
- Luo D, Chen L, Yu X, Ma L, Chen W, et al. (2017) Differences in urinary incontinence symptoms and pelvic floor structure changes during pregnancy between nulliparous and multiparous women. Peer J 5: e3615.
- Mallett VT, Bump RC (1994) The epidemiology of female pelvic floor dysfunction. Curr Opin Obstet Gynecol 6: 308-312.
- Boyle R, Hay-Smith EJ, Cody JD, Morkved S (2014) Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women: A short version Cochrane review. Neurourol Urodyn 33: 269-276.
- Van Geelen H, Ostergard D, Sand P (218) A review of the impact of pregnancy and childbirth on pelvic floor function as assessed by objective measurement techniques. Int Urogynecol J 29: 327-338.
- Hilton P, Dolan LM (2004) Pathophysiology of urinary incontinence and pelvic organ prolapse. BJOG 111(1): 5-9.
- Eickmeyer SM (2017) Anatomy and physiology of the pelvic floor. Phys Med Rehabil Clin N Am 28: 455-460.
- Irwin DE, Milsom I, Kopp Z, Abrams P, Cardozo L (2006) Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries. BJU Int 97: 96-100.
- Verbeek M, Hayward L (2019) Pelvic floor dysfunction and its effect on quality of sexual life. Sex Med Rev 7: 559-564.
- Barber MD, Bremer RE, Thor KB, Dolber PC, Kuehl TJ, et al. (2002) Innervation of the female levator ani muscles. Am J Obstet Gynecol 187: 64-71.
- Junginger B, Baessler K, Sapsford R, Hodges PW (2010) Effect of abdominal and pelvic floor tasks on muscle activity, abdominal pressure and bladder neck. Int Urogynecol J 21: 69-77.
- Sapsford RR, Hodges PW (2001) Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med Rehabil 82: 1081-1088.
- Ashton-Miller JA, DeLancey JO (2007) Functional anatomy of the female pelvic floor. Ann N Y Acad Sci 1101: 266-296.
- Herschorn S (2004) Female pelvic floor anatomy: The pelvic floor, supporting structures, and pelvic organs. Rev Urol 6(5): S2-S10.
- Handa VL, Roem J, Blomquist JL, Dietz HP, Muñoz A (2019) Pelvic organ prolapse as a function of levator ani avulsion, hiatus size, and strength. Am J Obstet Gynecol 221:41: e1-e7.
- Lu R, Zhang Y, Yu YP (2019) Application of ultrasound in diagnosis of uterine prolapse by measuring area of levator hiatus. Zhonghua Yi Xue Za Zhi 99: 2315-2318.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Rheumatology Research (ISSN:2641-6999)





