1823
Views & Citations823
Likes & Shares
Result: The training interventions provided among healthcare workers on tuberculosis infection control is statistically significant.
Conclusion: effective training on (TBIC) is the most effective intervention to limiting hospital transmission of TB in healthcare professionals providing tuberculosis care services. In recommendation: Training and retraining of healthcare professionals on (TBIC) strategy using WHO guidelines should be make priority of all government and partners in the tuberculosis program.
Keywords: Intervention, Occupational, Tuberculosis and healthcare workers
Abbreviation: TBIC: Tuberculosis Infection Control; HCWs: Healthcare Workers
METHODOLOGY
Design: Educational training using seminar method was use to provide educational training on infection prevention and control using WHO training manual on (TBIC) as an intervention to limit nosocomial transmission of tuberculosis among healthcare professionals in the study area.
Study Area: The study area is located at the northern part of Nigeria with 46,053 square kilometers coverage. 8,397,541 is the projected population of Kaduna State across the 23 LGA in 2017 with an increased to 3.0% of 6,113,503 of 2006 National projection (NBS, 2017). The entire populations are mostly farmers.
Settings: The training was carried out in General Hospital Rigasa for Zone A, General Hospital Gambo Sawaba for Zone B and Primary Healthcare Center Kauru for Zone C respectively.
Participants: The study include all healthcare professionals providing TB care services through DOTs such as public health, radiologist, medical doctors, nurses, community health workers, health record officer, environmental health etc.
Variable: the pre-test was used to assess the participant’s knowledge on TBIC using WHO training manual, while the post-test assessed the participants level of knowledge on TBIC using WHO training manual on tuberculosis infection prevention and control after the training intervention.
Data Source: Data was collected using a pre- and post-test on the general knowledge of TBIC using WHO training manual on tuberculosis infection prevention and control.
Study Size: total of 252 healthcare workers invited for the educational training on TBIC using WHO training manual as interventions to limit nosocomial transmission of tuberculosis among healthcare professionals in the area.
Sampling Procedure: A multistage sampling procedure was adopted for the conduct of this study. Stage 1, selected all local Government Area (LGAs) involved in providing TB care services through directly observed treatment short course (DOTs). Stage 2, stratified the local government according to the three sub political zones. Stage 3 selected 2 LGAs from each of the sub political zones considering urban and rural characteristics.
Statistical Methods: Data collected ware validated through data triangulations method and analyzed using SPSS version 23.0. All information was presented in tables.
Ethical Issues: Ethical approval ware secured from the Kaduna State Ministry of Health Research Ethics Committee and Health Research, Lead City University research ethical committee and Ethics Committee of the National Tuberculosis and Leprosy Training Center (HREC, NTBLTC). Data collected was strictly used for the purpose of this study.
Test of Hypotheses
Hypothesis 1
H01: There is no significant difference between the pre and post test
RESULT
Characteristics of the Respondents
The sum of 252 participants were trained out of which (52.6%) are males, (53.8%) are in between the ages of 25-34 with mean age of 31.51±8.24. Among these health workers (67.7%) ware married, (48.6%) had OND/NCE, (41.1%) obtained higher degree certificate and only (9.5%) obtained secondary school certificate and below. More than 50% of the participants were either laboratory personnel (28.7%) or community healthcare workers (26.8%) The result also shows that majority of the respondents (26.8%) while only (6.5%) were doctors respectively. About 36.6% of the respondents were from the general outpatient’s department, while (14.2%) where from the DOTS center.
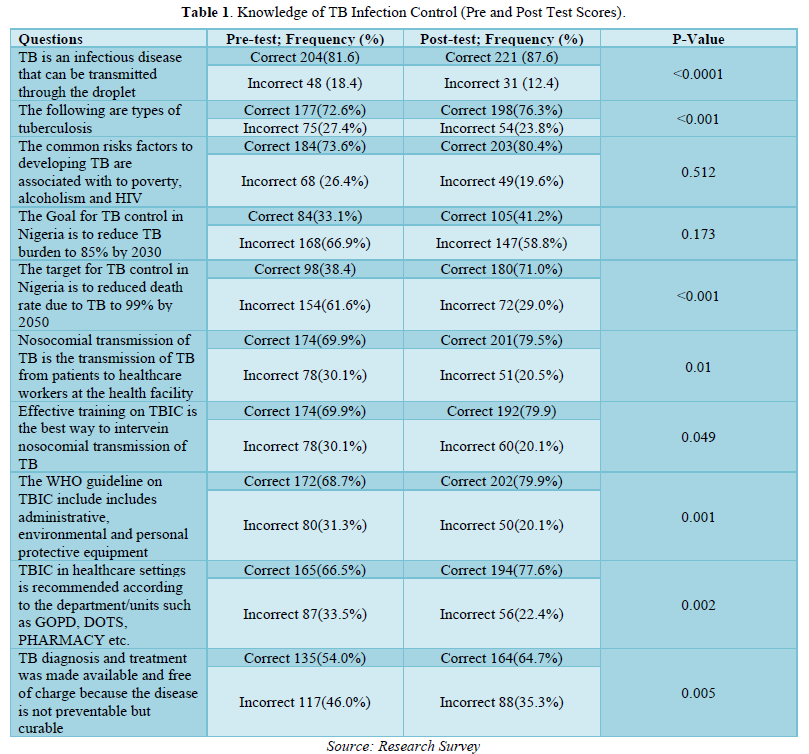
Educational Intervention to Limit Nosocomial Transmission of Tuberculosis among Healthcare Workers Providing TB Care Services (Pre-test and Post-test)
Of 252 total respondents 204(81.6%) answered rightly at the pre-test that TB is an infectious disease that can be transmitted through the droplet while 48(18.4%) answer incorrectly, On the same question 221(87.6%) of the respondents answered rightly at the post-test that TB is an infectious disease that can be transmitted through the droplet while 31(12.4%) answer incorrectly, this implies that the proportions of the respondents 221(87.6%) that answered rightly at the post-test is higher than the proportion of the respondents 204(81.6%) that answered correctly at the pre-test, this means that the training has increased the level of knowledge among the respondents that TB can be transmit via the droplet. It’s also observed that 177(72.6%) of the respondents answered rightly at the pre-test on the types of tuberculosis while 75(27.4%) answered incorrectly, on the same questions 198(76.3%) of the respondents answered rightly at the post-test on the types of TB while 54(23.8%) answered incorrectly, this implies that the proportions of the respondents198(76.3%) that answered rightly at the post-test is higher than the proportion of the respondents177(72.6%) that answered rightly at the pre-test, this means that the training has increased the level of knowledge among the participants on the types of tuberculosis infection. It’s also observed that 84(73.6%) of the participant answered correctly at the pre-test that the common risks factors to developing TB are associated with poverty, alcoholism and HIV while 68(26.4%) answered incorrectly, on the same questions 203(80.4%) answered correctly at post-test that the common risks factors to developing TB are associated with to poverty, alcoholism and HIV while 49(19.6%) answered incorrectly, this implies that the proportions of the respondents that answered rightly at the post-test 203(80.4%) is higher than the proportion of the respondents that answered rightly at the pre-test 84(73.6%), this means that the training has added value to the respondents. It’s also showed from the analysis of this result that 84(33.1%) of the respondents answered rightly at the pre-test that the Goal for TB control in Nigeria is to reduce TB burden to 85% by 2030 while 168(66.9%) answered incorrectly, on the same questions 105(41.2%) of the participant answered rightly at the post-test that the Goal for TB control in Nigeria is to reduce TB burden to 85% by 2030 while 147(58.8%) answered incorrectly, this implies that the proportion of the participants that answered rightly at the post-test 105(41.2%) is higher than the proportion of the participants that answered rightly at the pre-test 84(33.1%), this means that the training has increased the participants knowledge on the Goals of tuberculosis control in Nigeria. It’s also observed that 98(38.4) of the participants answered rightly at the pre-test that the target for TB control in Nigeria is to reduced death rate due to TB to 99% by 2050 while 154(61.6%) answered incorrectly, on the same questions 180(71.0%) of the participants answered correctly at the post-test that that the target for TB control in Nigeria is to reduced death rate due to TB to 99% by 2050 while 72(29.0%) answered incorrectly, this implies that the proportions of the of the participants that answered rightly at the post-test 180(71.0%) is higher than the proportions of the participants that answered rightly at the pre-test 98(38.4), this is means that the training has increased the level of knowledge of the participants on the targets of TB control in Nigeria. It’s also observed that 174(69.9%) of the participants answered rightly at the pre-test that Nosocomial transmission of TB is the transmission of TB from patients to healthcare workers at the health facility while 78(30.1%) answered incorrectly, on the same questions, 201(79.5%) of the respondents answered correctly at the post-test that Nosocomial transmission of TB is the transmission of TB from patients to healthcare workers at the health facility while 51(20.5%) answered incorrectly, this implies that the proportions of the respondents 201(79.5%) that answered rightly at the post-test is higher than the proportions of the participants 174(69.9%) that answered rightly at the pre-test, this means that the training has increased the level of knowledge among the respondent that nosocomial transmission of TB is the transmission of TB from patients to health care workers in health facilities. It’s also observed that 174(69.9%) of the participants answered rightly at the pre-test that Effective training on TBIC is the best way to intervein nosocomial transmission of TB while 78(30.1%) answered incorrectly, on the same questions 192(79.9) of participants answered correctly at the post-test that Effective training on TBIC is the best way to intervein nosocomial transmission of TB while 60(20.1%) answered incorrectly, this implies that the proportions of the respondents192(79.9) that answered rightly at the post-test is higher than the proportions of the respondents 174(69.9%) that answered correctly at the pre-test, this means that the training has added value to the participants that effectives training on TBIC is the best way to intervened the transmission of TB among HCWs. Its showed from the analysis of this study that 172(68.7%) of the participants answered rightly at the pre-test that the WHO guideline on TBIC include includes administrative, environmental and personal protective equipment while 80(31.3%) answered incorrectly, on the same questions 202(79.9%) of the respondents answered correctly at the post-test that The WHO guideline on TBIC include includes administrative, environmental and personal protective equipment while 50(20.1%) answered incorrectly. This implies that the proportions of the participants 202(79.9%) that answered rightly at the post-test is higher than the proportions of the respondents172(68.7%) that answered correctly at the pre-test, this means that the training has increased the level of knowledge of the respondents that WHO TBIC includes the administrative control, environmental control and the personal protective control measures. It’s observed that 165(66.5%) of the participants answered correctly at the pre-test that TBIC in healthcare settings is recommended according to the department/units such as GOPD, DOTs, Pharmacy etc. while 87(33.5%) answered incorrectly, on the same questions 194(77.6%) of the respondents answered rightly at the post-test that TBIC in healthcare settings is recommended according to the department/units such as GOPD, DOTs, Pharmacy etc. while 56(22.4%) answered incorrectly, this implies that the proportions of the respondents 194(77.6%) that answered rightly at the post-test is higher than the proportions of the respondents 165(66.5%) that answered correctly at the pre-test, this means that the training has added value to the participants that TBIC is recommended according to the units and departments. Its showered from the analysis of this study that 135(54.0%) of the participants answered rightly at the pre-test that TB diagnosis and treatment of TB disease was made available and free of charge in Nigeria, while 117(46.0%) answered incorrectly, on the same questions 164(64.7%) of the participants answered rightly at the post-test that TB diagnosis and treatment was made available and free of charge in Nigeria, while 88(35.3%) answered incorrectly respectively, this implies that the proportions of the participants that answered correctly at the post-test164(64.7%) is higher than the proportions of the participants 117(46.0%) that answered rightly at the pre-test, this means that the training has increased the knowledge of the respondents that the diagnosis and treatment of tuberculosis was made available in Nigeria (Table 1).
Decision Rule
If the P value is greater than the critical value (0.05) we fail to accept the null hypothesis, hence otherwise. Since the majority of the p value satisfies otherwise (i.e. less than 0.005), then the decision rule is to rej null hypothesis (H0) which states that there is significant difference between the pre and post-test.
DISCUSSION
This results is in line with a study that reported that educational training is the recommended intervention to improving the practice of tuberculosis infection control among nurses in Ibadan, south-west Nigeria [10]. Another study also documented that training of clinicians is the bases to reducing occupational tuberculosis [11]. Similarly, another study has reported that educational intervention is the key to limiting occupation diseases among healthcare workers [12].
LIMITATIONS
The findings cannot be generalized all over the country. However, the study provided adequate information on the intervention to limit nosocomial tuberculosis among healthcare professionals in the study area.
INTERPRETATION
The result of the training interventions provided on WHO guideline on tuberculosis infectious control shows that the interventions is statistically significant compering pre and post training overall scores.
CONCLUSION
Providing education training on TBIC is an intervention to limiting nosocomial transmission in healthcare settings.
RECOMMENDATION
Training and retraining of healthcare professionals on infection and prevention and control strategy using WHO manual should be make priority of all government and partners in the tuberculosis program.
WHAT IS KNOWN ABOUT THIS TOPIC
- The significance of educational intervention on tuberculosis infection prevention control in healthcare settings has been documented in many scientific studies.
- The effect of educational intervention on tuberculosis infection control was documented among nurses in Ibadan, Oyo State, Nigeria.
WHAT THIS STUDY ADDS
- The educational intervention on WHO guideline on tuberculosis infection control provided by this study is statistically significant.
COMPETING INTERESTS
The authors declared no competing interests.
- da Silva EH, Lima E, dos Santos TR, Padoveze MC (2022) Prevalence and incidence of tuberculosis in health workers: A systematic review of the literature. Am J Infect Control 50(7): 820-827.
- MacNeil A, Glaziou P, Sismanidis C, Date A, Maloney S, et al. (2018) Global Epidemiology of Tuberculosis and Progress Toward Meeting Global Targets-Worldwide, 2018. Morb Mortal Wkly Rep 69(11): 281-285.
- Paleckyte A, Dissanayake O, Mpagama S, Lipman MC, McHugh TD (2021) Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrob Resist Infect Control 10(1): 106.
- Okpokoro E, Lesosky M, Osa-Afiana C, Bada F, Okwor U, et al. (2023) Prevalence and Risk Factors for Mycobacterium tuberculosis Infection among Health Workers in HIV Treatment Centers in North Central, Nigeria. Am J Trop Med Hyg 1(aop).
- Baussano I, Nunn P, Williams B, Pivetta E, Bugiani M, et al. (2011) Tuberculosis among Health Care Workers. Emerg Infect Dis 17(3): 488-494.
- Islam MS, Chughtai AA, Banu S, Seale H (2021) Context matters: Examining the factors impacting the implementation of tuberculosis infection prevention and control guidelines in health settings in seven high tuberculosis burden countries. J Infect Public Health 14(5): 588-597.
- Agaya J, Nnadi CD, Odhiambo J, Obonyo C, Obiero V, et al. (2015) Tuberculosis and latent tuberculosis infection among healthcare workers in Kisumu, Kenya. Trop Med Int Health 20(12): 1797-1804.
- Zhou F, Zhang L, Gao L, Hao Y, Zhao X, et al. (2014) Latent Tuberculosis Infection and Occupational Protection among Health Care Workers in Two Types of Public Hospitals in China. PLoS ONE 9(8): e104673.
- Williams M, Ndlebe L, Ten HBW, Venter D (2020) Employees’ knowledge and practices on occupational exposure to tuberculosis at specialized tuberculosis hospitals in South Africa. Curations 43(1): 1-8.
- Akande PA (2020) The effect of an educational intervention to improve tuberculosis infection control among nurses in Ibadan, south-west Nigeria: A quasi-experimental study. BMC Nurs 19(1): 81.
- Murgia N, Gambelunghe A (2022) Occupational COPD-The most under-recognized occupational lung disease? Respirology 27(6): 399-410.
- Abdollahi T, Razi PS, Pahlevan D, Yekaninejad MS, Amaniyan S, et al. (2020) Effect of an ergonomics educational program on musculoskeletal disorders in nursing staff working in the operating room: A quasi-randomized controlled clinical trial. Int J Environ Res Public Health 17(19): 7333.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)

