21
Views & Citations10
Likes & Shares
CASE REPORT
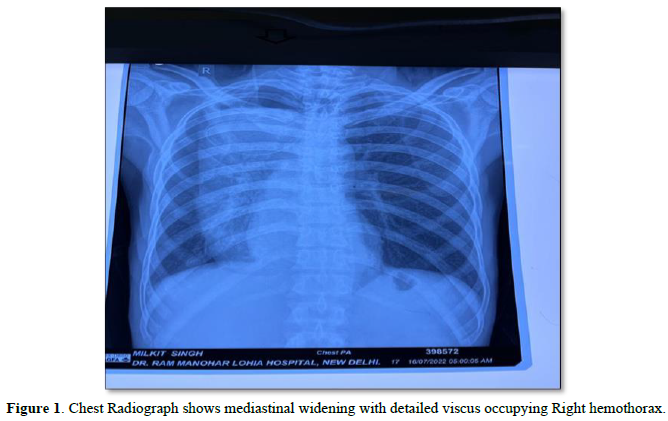
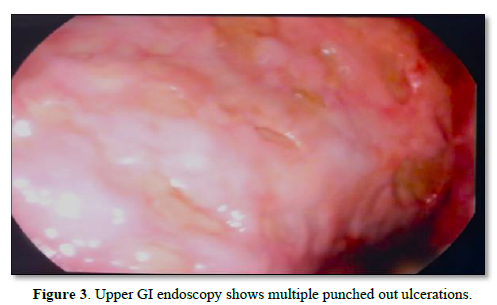
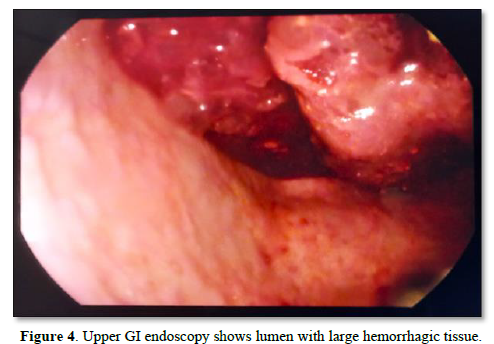
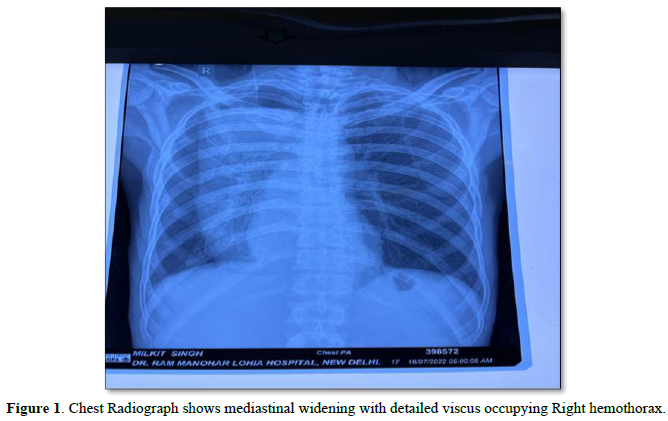
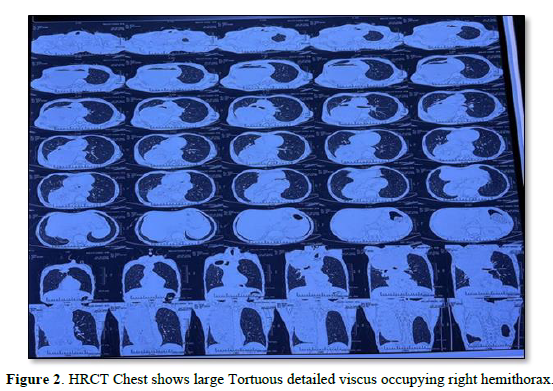
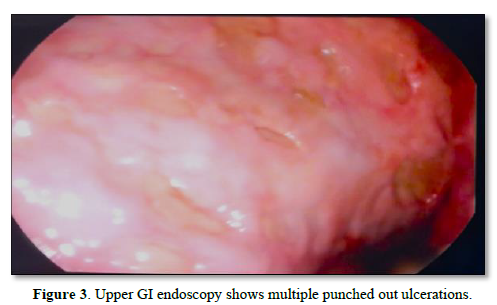
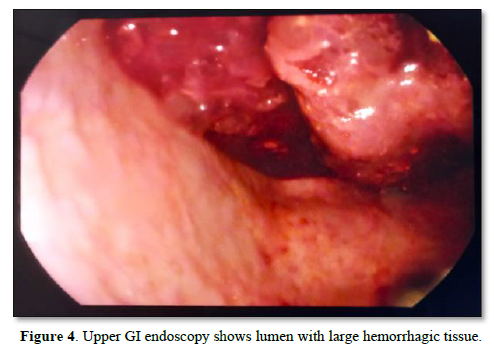
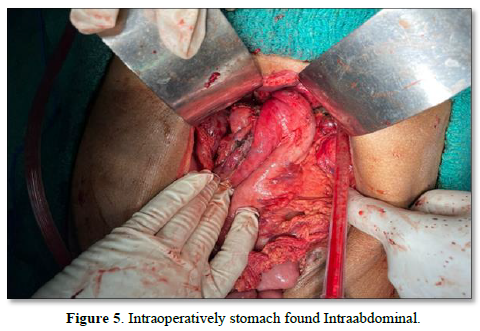
A 57-year-old male presented with complains of hematemesis with regurgitated food and water. His symptoms accompanied by sweating, fatigue. Patient had no history of regular use of NSAIDs, aspirin, immunosuppressant, any weight loss, Malena and hoarseness of voice. On physical examination patient had pale conjunctiva with decrease capillary refill time. Routine blood test showed Hemoglobin- 9.6 gm/dl, normocytic normochromic anemia which was significantly lower than baseline, white blood cell counts of 10 k/ml, platelet count 140 k/ml and potassium level 2.7 mmol/L. Chest radiograph reported as mediastinal widening with dilated viscus occupying most of right hemithorax (Figure 1). HRCT chest reported large tortuous dilated viscus occupying right hemithorax compressing right lung parenchyma suggesting of large rolling hiatus hernia (Figure 2). An upper GI endoscopy showed a dilated tortuous lumen, possibly of the esophagus. The entire scope was accommodated within this tortuous viscus. There were multiple punched-out ulcerations present till the maximum visibility of the scope (Figure 3). The lumen was further filled with frank blood with large hemorrhagic tissue adhered to the walls (Figure 4). The provisional diagnosis was a large, complicated rolling-type of hiatus hernia through the esophageal hiatus.The patient was planned for exploratory laparotomy. Intra-operatively, to our surprise, the stomach found normal intraabdominal (Figure 5). There was slight dilatation of the esophageal hiatus and of the abdominal part of the esophagus, however, no obvious herniation was identified. On passing a nasogastric tube from the head end, there was copious drainage of dark hemorrhagic contents. The tube was not palpated in the stomach or the abdominal esophagus. A diagnosis of achalasia and megaesophagus was then considered, bearing in mind that the nasogastric tube of small caliber was rolled-up inside the megaesophagus. A wide-bore (36 Fr) gastric calibration tube (GCT) used in bariatric procedures was then passed. Failure of the GCT to pass across the lower esophageal junction (LES) was considered to be confirmatory for the diagnosis of achalasia. A Heller’s cardiomyotomy was performed over the LES (total of 8 cm) and gastric fundus, which enabled the GCT to pass into the stomach. An anterior fundoplication (270°) was used to strengthen the defect and the nasogastric tube was passed till the pylorus.
The patient recovered over 2 weeks postoperatively with enteral and parenteral nutrition. He was discharged on oral feeding on POD 17, and is being considered for elective transthoracic esophagectomy after optimization.
DISCUSSION
Achalasia is an esophageal motility disorder due to neurogenic degeneration which result in hypertension of lower esophageal sphincter (LES), with consequent failure of LES relaxation. Achalasia is categorized based on etiology - primary or idiopathic, and, secondary if caused by parasitic infections like Trypanosoma’s Cruzi seen in chagas disease or, if associated with metabolic disease or tumors [4,5]. Presenting symptoms of achalasia consists of dysphagia, regurgitation and weight loss. The gold-standard test for diagnosis is esophageal manometry which demonstrates esophageal aperistalsis and increase LES pressure.
It is very rare for a patient of achalasia to present with upper gastrointestinal bleeding; the postulated mechanisms are esophageal ulcer or severe esophagitis due to loss of the mucosal protective barrier by the uncontrolled gastric acid reflux and by prolonged stasis [8]. Infections like Candida species, cytomegalovirus, and herpes simplex virus may be contributory in immunocompromised patients. Direct mucosal damage from the ingestion and stasis of caustic agents like tannins, nonsteroidal anti-inflammatory drugs (NSAIDs), bisphosphonates, and certain antibiotics may also complicate a pre-existing achalasia. In extreme cases, achalasia may present as near-fatal esophageal bleeding. Other long-standing complications can be megaesophagus, aspiration pneumonia, esophageal rupture, malnutrition, esophageal squamous cell carcinoma [2,9]. It is evident that patients who develop large episodic hematemesis from underlying ulcers with end-stage complications like megaesophagus, malignancy and cases refractory to medical treatment need to undergo esophagectomy [10].
Our patient presented with upper GI bleed with massive esophageal dilation mimicking hiatus hernia on UGI endoscopy and imaging. The diagnosis of achalasia was confirmed intra-operatively after failure to identify any intra-abdominal pathology. The standard surgical treatment involves pneumatic dilation or Heller’s cardio myotomy which both aim to reduce LES resting pressures. We performed Heller's cardio myotomy with anterior fundoplication as a temporizing measure in our moribund patient; we have further planned for elective transthoracic esophagectomy after optimization.
There are inherent challenges in the diagnosis and management of complicated achalasia, as evident from our case. With a large sigmoid dolichol mega esophagus undiagnosed previously, investigations like CT and endoscopy may also be limited in the emergency situation. The endoscope is often limited by the amount of blood, necrotic luminal contents and the increased tortuous length. Multiple endoscopies may be required to clearly diagnose the condition, since manometry is not a feasible option in these situations. This has also been documented in earlier reports [2]. Probably, intra-operative confirmation as we performed is the only feasible method.
CONCLUSION
This case demonstrates rare case of long-standing achalasia with megaesophagus that mimics hiatus hernia. Multiple endoscopies may be required to clearly diagnose the condition, since manometry is not a feasible option in these situations.
- de León San Juan AR, de la Serna Y Bueno JP (2017) Achalasia. New concepts. Med Clin 148(10): 453-455.
- Cho JH (2019) Massive esophageal bleeding in long-standing achalasia complicated by esophageal carcinoma and aspirin-induced stasis ulcer. Medicine 98: e16519.
- Tuason J, Inoue H (2017) Current status of achalasia management: A review on diagnosis and treatment. J Gastroenterol 52: 401-406.
- Pohl D, Tutuian R (2007) Achalasia: An overview of diagnosis and treatment. J Gastro Intestin Liver Dis 16: 297-303.
- O’Neill OM, Johnston BT, Coleman HG (2013) Achalasia: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 19: 5806-5812.
- del Pozo García AJ, Buey LG, Llorca I, Iscar T, Barxias M, et al. (2003) Relapsing upper bleeding in non-Hodgkin's esophageal lymphoma associated with achalasia. Eur J Gastroenterol Hepatol 15: 1127-1130.
- Kraft AR, Frank HA, Glotzer DJ (1973) Achalasia of the esophagus complicated by varices and massive hemorrhage. N Engl J Med 288: 405-406.
- Chiejina M, Samant H (2020) Esophageal ulcer. Stat Pearls Publishing, Treasure Island (FL). Available online at: https://pubmed.ncbi.nlm.nih.gov/29262120/
- Zhang WW, Xie XJ, Geng CX, Zhan SH (2015) Rare case of upper gastrointestinal bleeding in achalasia. World J Clin Case 3: 327-329.
- Bassi R, Saeed Y (2021) A Rare Case of a Life-Threatening Massive Upper Gastrointestinal Bleed and Airway Obstruction in a Patient with a Megaesophagus Secondary to Longstanding Achalasia. Cureus 13(2): e13204.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- International Journal of AIDS (ISSN: 2644-3023)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)