20
Views & Citations10
Likes & Shares
There are types called incomplete forms more common in females. In these forms the hypoplasia of the abdominal wall is partial or unilateral, associated or not with renal, testicular and osteoarticular malformations, which are generally on the same side. These partial forms are known as Pseudo-Prune Belly Syndrome (PPBS) [3,5].
The clinical forms can be very variable, ranging from stillbirth due to major renal and respiratory dysplasia to practically normal children. 95% of carriers of this syndrome are male, however it is generally more serious in girls due to a higher incidence of urethral atresia. This explains the diversity of opinion on the attitude to adopt in the face of this syndrome [4].
We report a case followed at the Kihumba Hospital Center for respiratory complications.
OBSERVATION
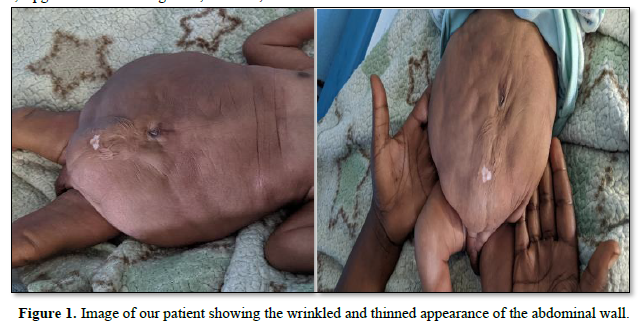
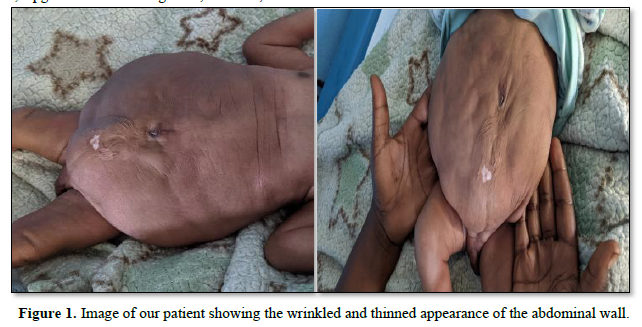
This is a male newborn, resulting from an unmonitored pregnancy carried to term, vaginal delivery, cephalic presentation, Apgar 7/8/8. Mother aged 25, G4P4E3, with no particular history. The clinical examination found a newborn acrocyanotic, hypotonic, with a sucking reflex present, a weight of 4300g, a height of 47cm and a head circumference of 34cm. The Finnistron at 38.5 SA. The respiratory examination notes a Silvermann score of 8/10. Abdominal examination reveals a thinned and wrinkled abdominal wall with palpation of the abdominal organs (Figure 1).
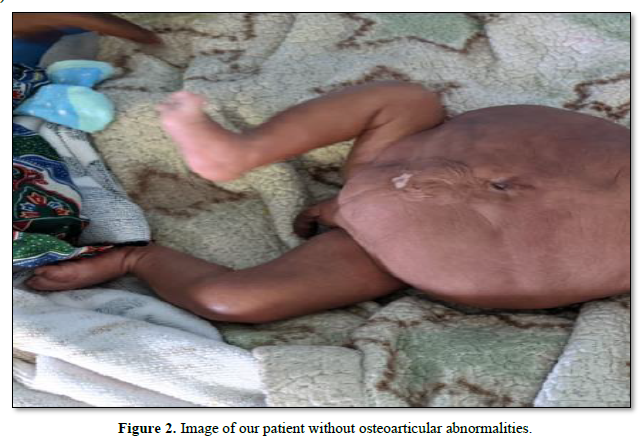
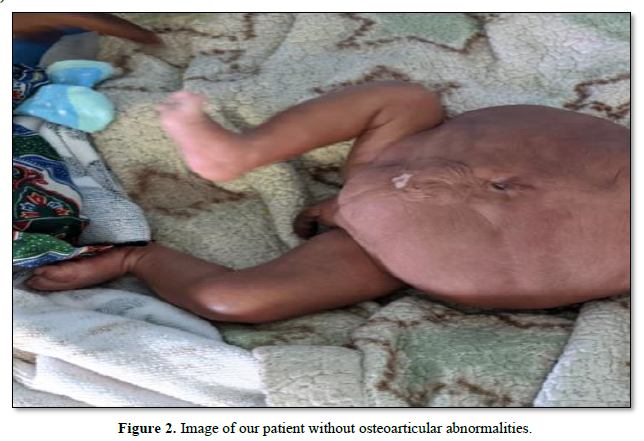
The osteoarticular examination found no malformation (Figure 2).
The cardiovascular examination was unremarkable. We have a scroctum not containing testicles.
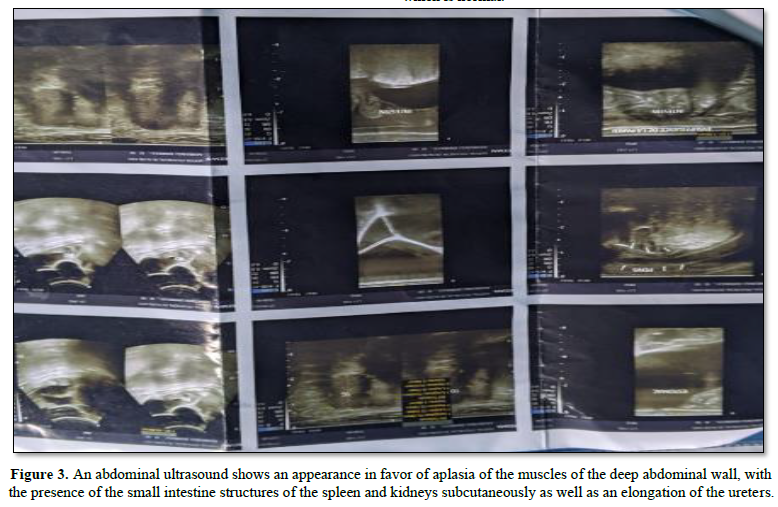
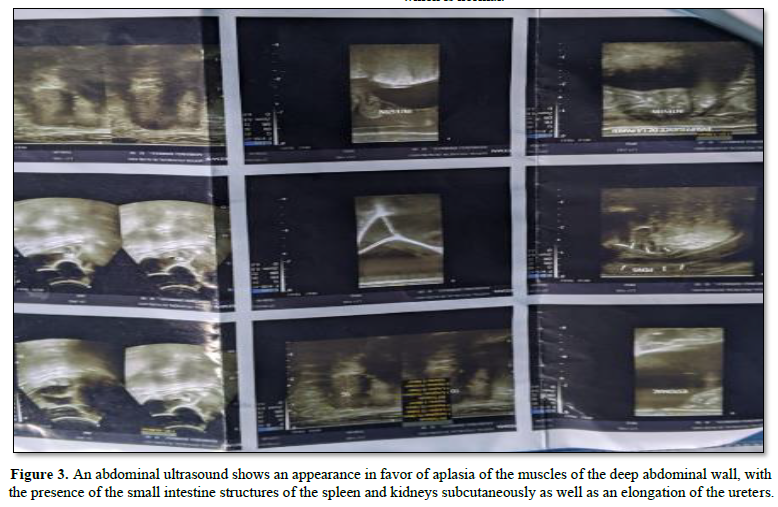
Paraclinical examinations include: An abdominal ultrasound shows an appearance in favor of aplasia of the muscles of the deep abdominal wall, with the presence of the small intestine structures of the spleen and kidneys subcutaneously as well as an elongation of the ureters (Figure 3). The biological tests are unremarkable, notably renal function which is normal.
We treated (respiratory distress which we linked to the insufficiency of the diaphragm to achieve its respiratory function) the newborn with oxygen, a double antibiotic therapy made of ampicillin and gentamycin for 5 days. After a month we suggested doing an orchidopexy, and transferring the patient to continue with the rest of the treatment in well-equipped hospitals. The family refused the intervention.
Note that the hypoplasia of the abdominal wall muscles and the elongation of the ureters was confirmed by an abdominopelvic ultrasound.
The family consulted us four months later for respiratory difficulty, we are already counted in their ascendants and we see an orchidopexy carried out at the Heal Africa hospital in Goma. As a presumptive diagnosis, we suspected bronchopulmonary dysplasia and/or bronchiolitis in infants and we treated him with nebulization of salbutamol, dexamethasone, adrenaline with physiological serum with clinical improvement and discharge in 7 days was granted.
DISCUSSION
This pathology called Prune Belly syndrome was first described around 1839 by Fröhlich. Later in 1895, Parker made the first description involving urinary tract abnormalities. And it was only in 1950 that Osler named it "Prune Belly" because of the appearance of the abdominal wall [1,2]. It remains a rare disease and most studies specify that its incidence remains at one case in 40,000 births [2]. This condition is marked by a clear male predominance with 95% of patients are male [4,6,7] and this correlates with our patient who is also male. The exact etiology of PBS is unknown. There are several theories of which three predominate: the one which proposes a prenatal obstruction of urine, the one which is based on embryology and which proposes the failure of primary mesodermal differentiation between the 6th and 10th week of gestational age which leads to defective muscle building of the abdominal wall and the urinary tract. And finally, that of the bladder bags, which suggests dysgenesis of the velum sac and the allantois [2].
Clinically, this syndrome presents itself with urinary malformations, namely a megabladder, dilated urethras and ureters which can also be stenotic, polycystic kidney disease, hydronephrosis, and sometimes a diverticulum near the vesicoureteral and urethral junction [1,2,7]. Note that up to 75% of patients with PBS associate other malformations, notably pulmonary, cardiac, skeletal, gastrointestinal and genital malformations. These malformations were reported by Routh et al with an incidence of 25% for cardiovascular, 24% for gastrointestinal, 23% for musculoskeletal, 58% for respiratory and 15% for genital [2]. Osteoarticular malformations such as club foot, hip dysplasia, vertebral malformations, and scoliosis. No skeletal malformation was found in our patient.
Our patient presents genital malformations such as cryptorchidism present in almost all male patients, however. Genital malformations in women include vaginal atresia, bicornuate uterus and urogenital sinus. There has never been a case of infertility for both women and men [8,9]. In rare cases the hypoplasia of the muscles of the abdominal wall is unilateral, as are the other associated renal, testicular and bone malformations generally found on the same side as the abdominal muscular hypoplasia, thus describing the incomplete form generally more frequent in the female gender, also called Pseudo Prune Belly Syndrome (PPBS) [3,5]. Our patient, on the other hand, presents generalized abdominal muscle hypoplasia, bilateral renal and testicular malformations and has no bone malformations, which makes him a rare case.
Diagnosis is based prenatally on obstetric ultrasound and makes it possible to detect abnormalities of the urinary system associated with the typical appearance of the abdominal wall. Hosbino reported a case of PBS diagnosed at 12 weeks of pregnancy [1,2]. After childbirth it is based on the completed abdominopelvic ultrasound which should be supplemented by an abdominopelvic CT, a transthoracic ultrasound to look for cardiac malformation, a renal assessment to assess renal function, an ultrasound of the hips with a skeletal x-ray looking for skeletal malformations as well as a karyotype looking for deletion of nuclear factor 1-beta (HNF1beta) [1,10].
Treatment is essentially based on surgery: abdominoplasty, orchidopexy and reconstruction of the urinary tract [1,6,11]. This treatment is dictated on a case-by-case basis for severe cases. Regardless, whether surgical treatment is undertaken or not, patients with PBS require permanent multidisciplinary medical care and close monitoring. For our patient, we started by treating the respiratory distress and its complications, a bilateral orchidopexy was performed and will be followed in another hospital specialized for the reconstitution of the urinary tract and abdominoplasia. Pulmonary hypoplasia is the main cause of mortality in the neonatal period. Let's say that for our patient, after a month post-orchidopexy, he presented respiratory distress and we thought it was bronchopulmonary dysplasia. The severity of urinary tract abnormalities and renal function determine not only mortality, but also long-term prognosis [1,7]. Nebulization combining salbutamol, dexamethasone, adrenaline and physiological serum allowed us to stabilize the respiratory state of our patient.
CONCLUSION
Prune Belly syndrome affects males in 95% of cases. Renal failure and pulmonary hypoplasia are the main causes of mortality. In the absence of the classic triad, it will be necessary to look for other malformations given the existence of atypical forms, in order to undertake adequate and immediate treatment.
The case of our patient remains atypical given that he does not present skeletal malformations and abdominal wall dysplasia is widespread. Brochodyspalsia is the complication that risks ending the life of our patient even if we have stabilized the two episodes of distress that he presented by repeated nebulization; the prognosis for survival remains poor.
- Xu W, Wu H, Wang D-X (2015) A Case of prune belly syndrome. Pediatr Neonatl 56(3): 193-196.
- Fette A (2015) Associated rare anomalies in prune belly syndrome: A case report. J Pediatr Surg Case Rep 3: 65-71.
- Zugor V, Labanaris AP (2012) The prune belly syndrome: Urological aspects and long-term outcomes of rare disease. Pediatr Rep 4(2): e20.
- Soukaina B (2018) Prune belly syndrome: An uncommon case. Pan Afr Med J 29: 129.
- Grover H, Sethi S, Garg J, Ahluwalia AP (2017) Pseudo Prune Belly syndrome: Diagnosis revealed by imaging? A case report and brief review. Pol J Radiol 82: 252-257.
- Diao B, Diallo Y, Fall PA, Ngom G, Fall B, et al. (2008) Syndrome de Prune Belly? Aspects épidémiologiques, cliniques et thérapeutiques. Prog En Urol 18: 470-474.
- Seidel NE, Arlen AM, Smith EA, Kirsch AJ (2015) Clinical manifestations and management of Prune Belly syndrome in a large contemporary pediatric population. Urology 85(1): 211-215.
- Gallo C, Costa W, Favorito L, Sampaio F (2017) Prune belly syndrome: is penile structures similar to normal fetuses? In: State University of Rio de Janeiro, Urogenital Research Unit, Rio de Janeiro, Brazil. London, United Kingdom.
- Tibor-Denes F, Tavares A, Machado M, Giron A, Srougi M (2017) Gonadal function and reproductive system anatomy in post pubertal prune belly syndrome patients. J Urol 197(4S).
- Granberg CF, Harrison SM, Dajusta D, Zhang S, Hajarnis S, et al. (2012) Genetic basis of prune belly syndrome: Screening for HNF1? gene. J Urol 187(1): 272-278.
- Dénes FT, Park R, Lopes RI, Moscardi PRM, Srougi M (2015) Abdominoplasty in Prune Belly Syndrome. J Pediatr Urol 11(5): 291-292.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Pathology and Toxicology Research
- International Journal of Diabetes (ISSN: 2644-3031)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)