Review Article
Novel Formulation of Aloe vera and Quercetin in the Management of Dermal Disease: Eczema
6572
Views & Citations5572
Likes & Shares
Eczema, also known as atopic dermatitis, is a state that compels your skin inflamed or irritated. Scientific investigations claim that aloe vera, an admired natural plant product may aid to manage the eczema. There is not much research evaluating the use of aloe vera for eczema. But it is well known to have anti-bacterial and anti-fungal properties, along with anti-inflammatory properties, could be particularly applicable to manage the eczema. Quercetin efficaciously inhibits the secretion of histamine and pro-inflammatory markers along with evident to decrease eczema. Thus, amalgamated effect of aloe vera and quercetin may synergize the therapeutic efficacy in the management of eczema. Topical treatment is often the first‐line remedy for mild to moderate eczema. Dermal formulations (Cream, ointment, gel etc.) are still the main therapeutic approach for the treatment of skin disorders. Present studies emphasize the types, etiology, symptoms, prevention and herbal therapeutic options for the management of eczema.
Keywords: Skin disorders, Eczema, Aloe vera, Topical formulation, Quercetin
INTRODUCTION
Eczema is a dermal disorder wherein blemish of skin begin dry, broken, and rough. Some types can also cause blebs. Eczema is usually, chronic, non-contagious skin disorder. The main indication of this inflammatory disease is a very itchy rash. There is generally no cure for eczema, but it can be managed with consistent medical care and a systematic treatment plan. Some types of eczema can be prevented by avoiding stress, infliction, and belongings that cause allergic response [1]. Eczema may produce potential for complications, such as a secondary bacterial or fungal infection of the eczema rash.
Aloe vera (A. vera) evolve wild in tropical, semi-tropical, and arid climates worldwide. It is cultivated for agricultural and medicinal applications. A. vera is one of the most paramount plants used in traditional medicine. A. vera contains enzymes, minerals, vitamins, acids, amino acids, lipids, lectin, lactates, salicylates, phenolics, polysaccharides, urea. A. vera is conventionally applied to relieve itching and inflammation, wound healing as well as antimicrobial properties [2,3]. Aloenin is an important compound of A. vera used in skin allergies, burns and insect bites. Aloenin is efficacious in healing damaged dermal situation [4].
Quercetin is able to reduce wheal, flare and itching of damaged skin. It may also help to restore skin barrier function and integrity. Quercetin is a natural flavonoid. It is obtained from several plants and foods, such as onions, apples, green tea, Ginkgo biloba, berries, St. John's wort, American elder, and others. It functions as antioxidants and plays an important role to combat free radical damage, which is related to various diseases [5,6].
Dermal formulation is the most common and popular approach to manage skin diseases [7]. A. vera herbal formulations available in the form of cream, gel, facial solution, moisturizer etc. Quercetin is formulated in different dermatological preparations as gel, emulgel and microemulsion gel. Combination, sequential and rotational ways are often more promising and better over single-agent remedies in the management of ailments [8]. There are a variety of novel remedies or topical formulations such as nano emulsions, microemulsion, multiple emulsion, liposomes, aerosol foams, hydrogel, organogel, nanogel etc. available that are frequently applied in order to target concurrent multiple pathogenic factors [9]. Therefore, A. vera and quercetin combination in novel topical formulation are proposed as viable remedies for effective eczema management.
ECZEMA AND ITS MANAGEMENT
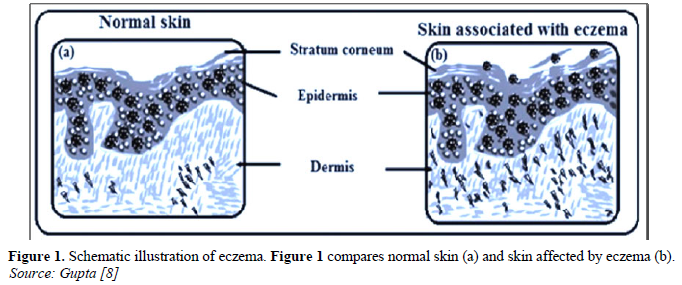
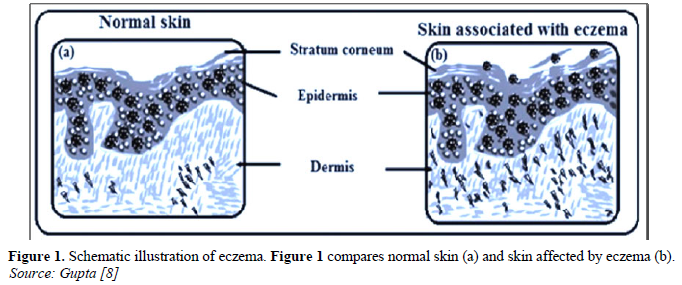
Eczema is a common incendiary skin amitosis that is increasing in acclaim. The inception of eczema (also known as atopic dermatitis or atopic eczema/dermatitis syndrome) commonly takes place in the first few months of life and generally within the first year of life. The exact rationale of eczema is unknown, but factors that may trigger or aggravate the condition include food and environmental allergens or annoyance, heat or cold, stress, and genetic susceptibility. Severe eczema can give rise to notable morbidity and have crucial social, emotional and financial influences on children and their families [10]. Histologically, three features of eczema are observed (Figure 1). Expansion of the stratum corneum is due to disruption to the cornification process, abnormal accumulation of fluid occurs due to destruction of the proteins involved in tight junctions, thereby leading to uncontrolled gesture of fluids in the paracellular space, infiltration of the dermis by immune cells is an indication of the primary immune reaction itself or in response to the ingress of allergens through a cracked dermal barrier [11].
Eczema has been an engrossing challenge for it is proficient of remissions and worsening. Evidently, it is tough to circumvent the allergens entangled for the condition, more so in the underprivileged candidate of the disease. Nonetheless, it is valuable to dwell on the therapies available thus far to relieve the symptoms and signs. Although dermal corticosteroids are often used to manage the predominant symptoms of the ailment, the persistency of the situation increases the risk of everlasting unwanted effects. Herbal medicine is as old as civilization. Utilization of traditional herbal medicine is extensive in different province of the world. Herbal remedies are generally distinguished as effective and have fewer side effects. Many herbs are used to treat various dermal diseases including eczema. Among them is A. vera which has demonstrated great results in dermal diseases [12].
GLIMPSE ON ALOE VERA
The scientific name of A. vera is Aloe barbadensis miller. It is a member of Asphodelaceae (Liliaceae) family, and is a shrubby or dendriform, perennial, xerophytic, fleshy with serrated edges, green color plant. A. vera leaf is comprise of three strata: 1) An inner clear gel; 2) The middle layer of latex, 3) The outer thick layer of 15-20 cells. A.vera has antioxidant, anti-inflammatory, antimicrobial, antineoplastic, hypoglycemic and immune enhancing properties. It is applied traditionally to manage many ailments. It is applied topically for wound healing, soothing inflamed skin and various dermal lesions. Many investigations revealed that A. vera decreases the manifestations of eczema such as skin dehydration, scaling and refined the skin quality. In addition, its antimicrobial properties prevent further infection [13,14].
MEDICINAL PROPERTIES OF ALOE VERA
The medicinal properties of A. vera are based on mostly by incidental data. Though most of these applications are interesting, systematic trials are essential to measure its effectiveness in all the following diseases.
Properties based on scientific corroboration
These properties have been tested in humans or animals. Safety and efficacy have not always been proven. Medicinal properties based on scientific evidence was observed in the conditions like psoriasis, seborrheic dermatitis, vulgaris, skin burns, genital herpes, Type 2 diabetes, HIV infection, neoplastic lesions, ulcerative colitis, wound healing, mucositis, radiation dermatitis, acne vulgaris, lichen planus, frostbite, constipation, and aphthous stomatitis [15].
Properties based on historical convention or theory
These medicinal properties often have not been thoroughly investigated in humans. Safety and effectiveness have not always been proven in traditional and scientific theories for the conditions like alopecia, bacterial and fungal dermal infections, chronic leg wounds, systemic lupus erythematosus, arthritis and parasitic infections [2].
Aloe vera in Dermal Protection and Disease
- vera maintains the skin moist and thus it is conventionally used as a moisturizer to cure the dehydrated skin. For example, A. vera gel gloves can build up dermal integrity and reduces the appearance of fine lines and erythema [16] and can be used for the treatment of pimples. Among different A. vera extracts, aloe mucopolysaccharides aid to combine water with the skin [17], thus providing moisturizing results. The leaf gel materials of A. vera was investigated which reveals that it boosts skin entropy, uniformity and energy at 30 and 90 min post application and thus have a greater hydrating effect [18]. A. vera also shields the skin from aging and it is thus having lots of scope in cosmeceuticals [17]. In clinical studies of radiation-induced dermatitis, A. vera extract can lower the influence of ultraviolet light on the skin, as some of the antioxidants and vitamins found in A. vera leaf can counteract the impact of ultraviolet (UV) radiation [19] A. vera gel can alter the release of dermal keratinocytes derived from immunosuppressive cytokines like interleukin-10 (IL-10), thereby minimizing UV-induced delayed hypersensitivity responses [20]. Observations have shown that A. vera gel accommodates small molecule immunomodulators, such as G1C2F1, which minimizes epidermal Langerhans cells from UV-induced dermal immune responses [21]. These investigations presumed scientific proof holding up the traditional use of A. vera as a topical protective agent. A. vera gel has conventionally been considered to be a skin healing flora [22]. A. vera gel also exhibited beneficial consequence on the epidermal keratinocytes during the wound healing activity. A. vera gel plays a crucial part in the management of superficial and partial thickness burns. A. vera gel also exhibited beneficial consequence on the epidermal keratinocytes during the wound healing activity. A. vera gel plays a crucial part in the management of superficial and partial thickness burns.
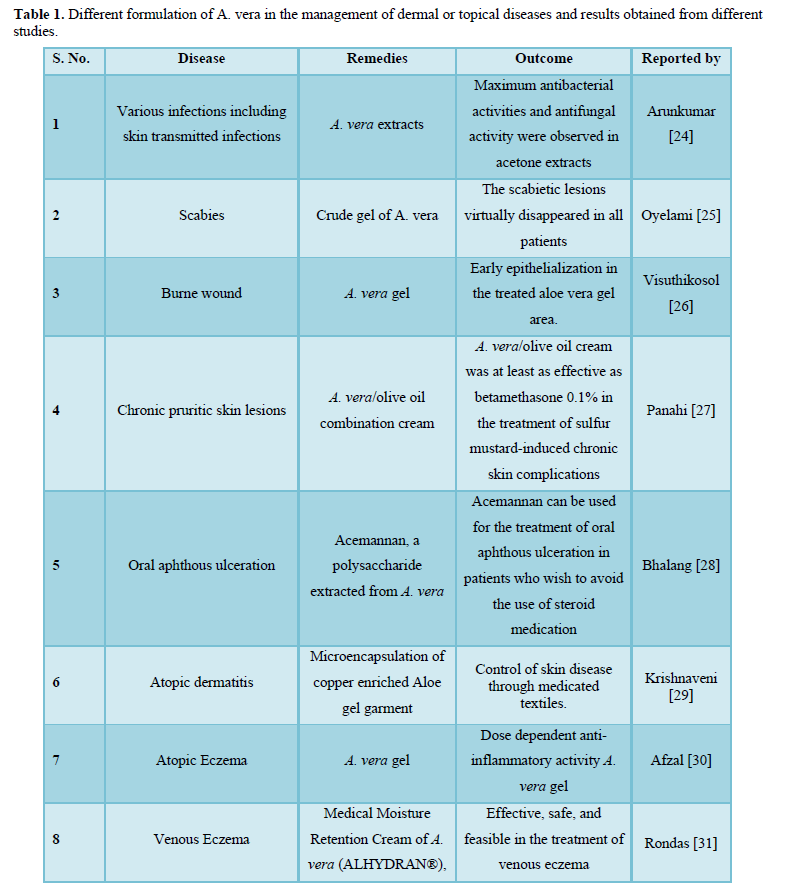
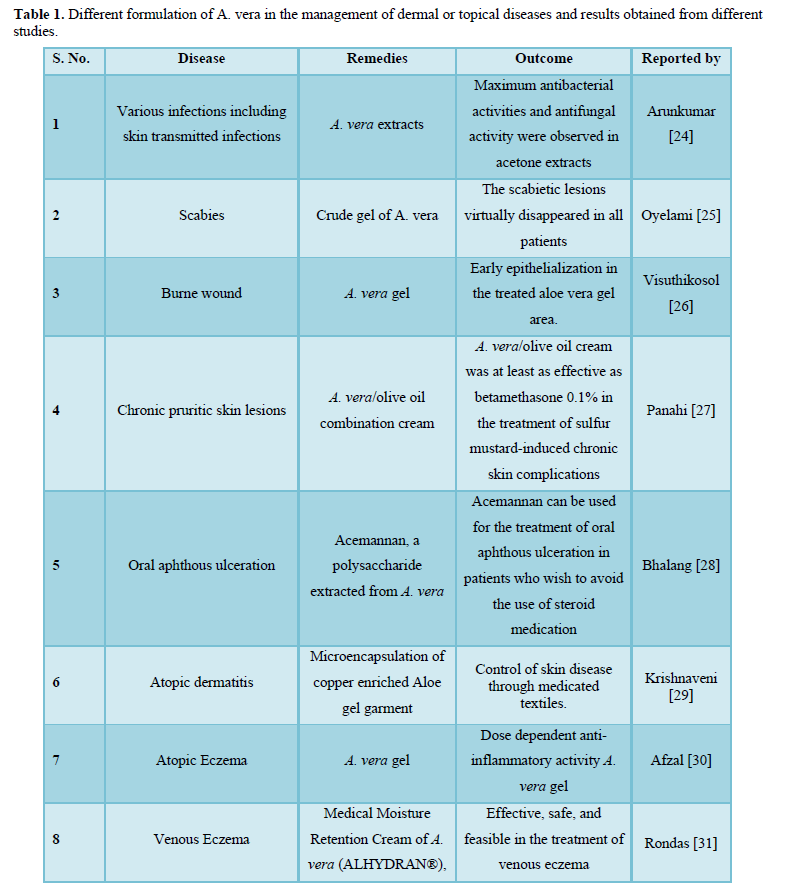
Several relevant investigations have showed that Aloe and its active components have potent therapeutic effects on several chronic dermal diseases like psoriasis and acne [23], as well as various kinds of dermal inflammations (Table 1). Moreover, it has been reported that A. vera lotion has a prophylactic action by reducing the impact of radiation-induced dermatitis [19]. Several earlier investigations have revealed that A. vera and its active compounds have encouraging potential for the effective management of dermal diseases with lower adverse effects.
QUERCETIN AT A GLANCE
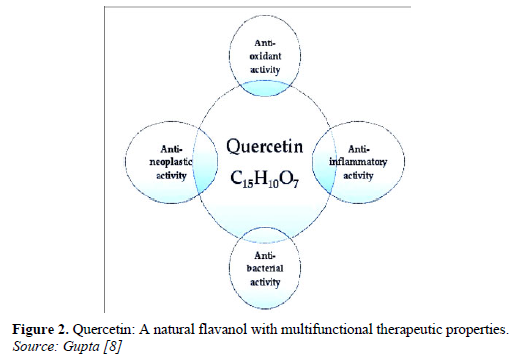
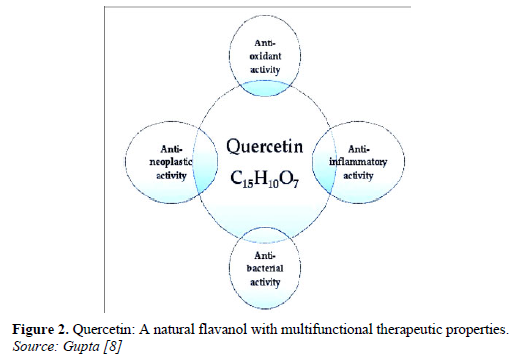
Quercetin is classified as plant derived component, flavanol. It is reported that, quercetin has shown an excellent in vitro antioxidant. Within the flavonoid family, quercetin is the most potent scavenger of Reactive oxygen species. Earlier in vitro studies have shown that quercetin also possesses anti-microbial, anti-inflammatory, anti-proliferative activities, immuno-suppressive, anti-fibrotic, anti-coagulative, anti-atherogenic and antihypertensive. Quercetin also confines great prospective for dermal application, as it shows strong protective influence against UV-induced lipid peroxidation [32] and proved to be efficacious on human skin with anti-ageing activity and skin rejuvenation potentiality [33].
QUERCETIN IN CUTANEOUS DISORDERS
Quercetin is an encouraging potential compound for dermal diseases as it holds powerful antioxidant [34] and broad anti-inflammatory activities [35]. These activities can be executed in the management of dermal inflammatory diseases like psoriasis and in the favor of skin in response to oxidative stress persuaded by UV irradiation [36]. As the outermost protective organ of the human body, the skin is vulnerable to oxidative stress caused by environmental imbalance, which leads into various skin damage and diseases, such as aging, cancer, and inflammation (Figure 2). In the countenance of ultraviolet radiation, air pollution, and other extrinsic factors on the skin, it is of great importance to use substance that can hinder oxidative stress and inflammatory response to treat inflammatory dermal lesions and delay the skin aging. The antioxidant ability of OH on quercetin is playing a crucial role for anti-inflammatory and anti-oxidative responses. It is investigated that quercetin is applicable in treatment of furunculosis, dermatitis, atopic dermatitis, eczema, and other inflammatory dermal diseases.
NOVEL TOPICAL FORMULATIONS IN THE MANAGEMENT OF ECZEMA
Therapeutics is applied dermally to the skin especially for their local or site-specific action. Even though, the dermal delivery of the drug can also be applicable for systemic activity. Over the previous years, dermal delivery of drugs has given rise to more and more attention, of which, systemic side effects can be minimized in comparison to parenteral or oral drug delivery. Dermal delivery of the drug circumvents hepatic first-pass metabolism and extensive fluctuations of drug-plasma levels caused by repeated oral administration of rapidly eliminated drugs. Based on the characteristics of the ingredients and on the condition of the skin to be applied, a dispensing medium to provide a stable physicochemical environment that protects the active compound from chemical and enzymatic degradation should be developed, that can be a liquid or semi-solid, monophasic or multiphasic (dispersed systems). Inflammation of hypertrophic scar on the eczematous lesions forms a strong barrier for the skin permeation of medicaments through dermal route. To overcome this challenge, various novel topical formulations such as hydrogels, microemulsions, solid lipid nanoparticles, liposomes, dendrimers, and microsponges, nanogels, organogels etc. [37] have been explored for the penetration enhancement and prolonged release actions. These preparations are depicted to be applied not only as “drug carriers”, but also play a role in “drug depots” for releasing active ingredients over a sustained period of time.
SCOPE OF PHYTO-CHEMICAL IN NOVEL TOPICAL FORMULATION
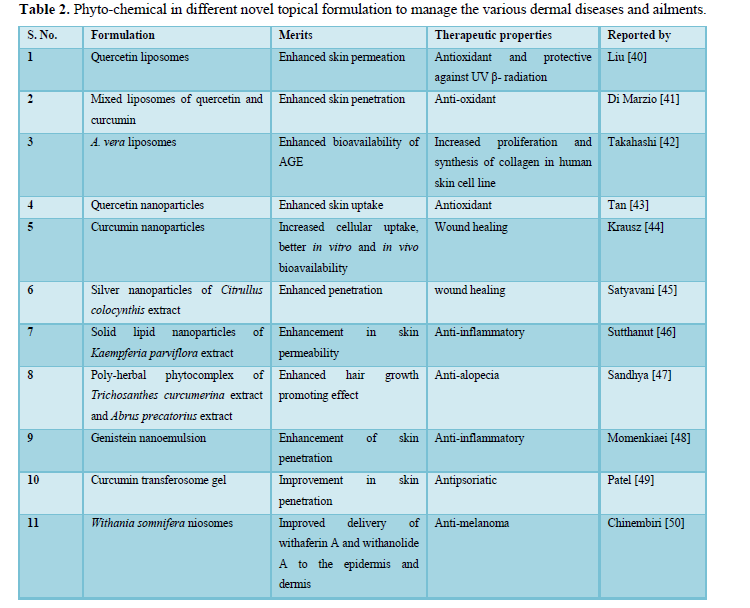
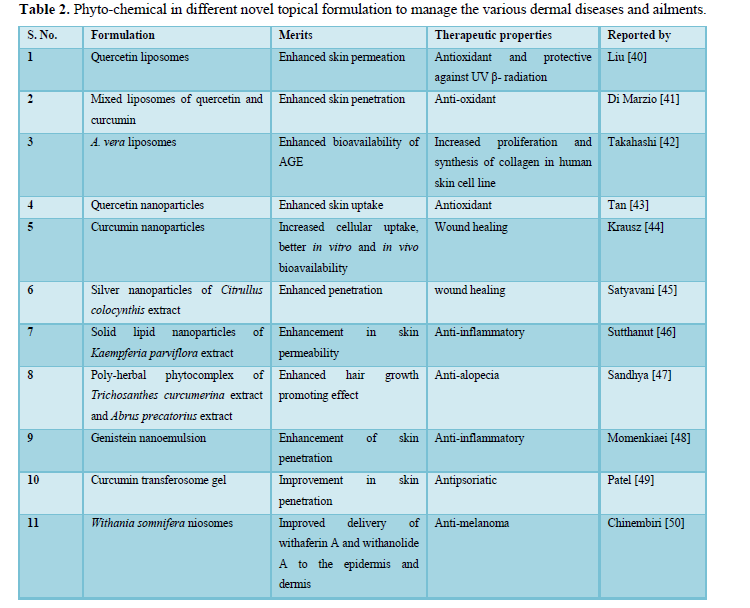
Dermal applications of drugs, herbal or others are applied with a diversity of desired effects, including the targeting of local tissues for dermal consequences, to the targeting of deeper strata, to the seeking out of a broader systemic influence. The history of the dermal application of plant-based medicines is over the prolonged period of time with documentations within traditional medicinal systems [38]. Herbal medicines are used in the management of a wide variety of conditions extending from dermatitis and psoriasis to dermal infections to dermal malignancies. However, the skin does provide an alarming barrier and novel drug delivery systems are being revolve to as a means to enhance dermal absorption. It is the incorporation of herbal medicines into such novel drug delivery systems. The key novel formulations that have been more specifically utilized for the dermatological and transdermal applications of herbal medicines are polymeric nanoparticles, liposomes, ethosomes, nano-emulsions, transferosomes, phytosomes and novel gels (Table 2). All these are reserving much interest to aggravate the therapeutic efficacy of phyto-chemicals [39].
CONCLUSIONS
Eczema is characterized by dry, rough and broken topmost layer of the skin known as stratum corneum. Several medicinal plant species applied to treat dermal ailments was investigated and documented since ancient time. Several investigated species are claimed very useful. However, these medicinal floras demanding a phytochemical screening for active moieties, biological properties and clinical studies are of universal significance. Using natural constituents in different novel topical formulations for skin care are very popular today. Moreover, one such type of natural plant; A. vera contain a lot of constituents which can be useful for dermal care. It is reported that A. vera possesses anti-aging and wrinkles reducing properties, moisturizing and cooling responses on the skin without allergic reaction, and burned wound healing effects on the skin. Their potential is still undefined and need more investigations. Indeed, more research trials and clinical evidences are needed. It was shown that using only one natural constituent is not enough for skin care. Maybe, combination of several different natural components is a right solution. Quercetin along with A. vera might be useful in the management of eczema due to its antioxidant and anti-inflammatory activity. Also, it is necessary to find out in which novel formulation the selected combination is stable and showing the best results.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
Wollenberg A, Barbarot S, Bieber T, Christen‐Zaech S, Deleuran M, et al. (2018) Consensus‐based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: Part I. J Eur Acad Dermatol Venereol 32(5): 657-682.
-
Maan AA, Nazir A, Khan MKI, Ahmad T, Zia R, et al. (2018) The therapeutic properties and applications of Aloe vera: A review. J Herb Med 12: 1-10.
-
Kumar R, Singh AK, Gupta A, Bishayee A, Pandey AK (2019) Therapeutic potential of Aloe vera - A miracle gift of nature. Phytomedicine 60: 152996.
-
Gao Y, Kuok KI, Jin Y, Wang R (2019) Biomedical applications of Aloe vera. Crit Rev Food Sci Nutr 59(sup1): S244-S256.
-
Ulusoy HG, Sanlier N (2020) A mini review of quercetin: From its metabolism to possible mechanisms of its biological activities. Crit Rev Food Sci Nutr 60(19): 3290-3303.
-
Polerà N, Badolato M, Perri F, Carullo G, Aiello F (2019) Quercetin and its natural sources in wound healing management. Curr Med Chem 26(31): 5825-5848.
-
Pivetta TP, Silva LB, Kawakami CM, Araujo MM, Del Lama MPF, et al. (2019) Topical formulation of quercetin encapsulated in natural lipid nanocarriers: Evaluation of biological properties and phototoxic effect. J Drug Deliv Sci Technol 53: 101148.
-
Gupta V, Dhote V, Paul BN, Trivedi P (2014) Development of novel topical drug delivery system containing cisplatin and imiquimod for dual therapy in cutaneous epithelial malignancy. J Liposome Res 24(2): 150-162.
-
Manasiya M, Sawarkar S, Bajaj A (2019) Topical Vitamin A Delivery: Challenges, Overview of Novel Approaches. Indian Drugs 56: 7-19.
-
Tizek L, Schielein MC, Seifert F, Biedermann T, Böhner A, et al. (2019) Skin diseases are more common than we think: Screening results of an unreferred population at the Munich Octoberfest. J Eur Acad Dermatol Venereol 33(7): 1421-1428.
-
Bell DC, Brown SJ (2017) Atopic eczema treatment now and in the future: Targeting the skin barrier and key immune mechanisms in human skin. World J Dermatol 6(3): 42-51.
-
Zari ST, Zari TA (2015) A review of four common medicinal plants used to treat eczema. J Med Plant Res 9(24): 702-711.
-
Rahmani R, Gharanfoli M, Gholamin M, Darroudi M, Chamani J, et al. (2020) Plant-mediated synthesis of superparamagnetic iron oxide nanoparticles (SPIONs) using aloe vera and flaxseed extracts and evaluation of their cellular toxicities. Ceram Int 46(3): 3051-3058.
-
Sánchez M, González-Burgos E, Iglesias I, Gómez-Serranillos MP (2020) Pharmacological update properties of Aloe vera and its major active constituents. Molecules 25(6): 1324.
-
Surjushe A, Vasani R, Saple DG (2008) Aloe vera: A short review. Indian J Dermatol 53(4): 163-166.
-
West DP, Zhu YF (2003) Evaluation of aloe vera gel gloves in the treatment of dry skin associated with occupational exposure. Am J Infect Control 31(1): 40-42.
-
Sahu PK, Giri DD, Singh R, Pandey P, Gupta S, et al. (2013) Therapeutic and medicinal uses of Aloe vera: A review. Pharmacol Pharm 4(8): 599.
-
Fox LT, Du Plessis J, Gerber M, Van Zyl S, Boneschans B, et al. (2014) In Vivo skin hydration and anti-erythema effects of Aloe vera, Aloe ferox and Aloe marlothii gel materials after single and multiple applications. Pharmacogn Mag 10(Suppl 2): S392-S403.
-
Haddad P, Amouzgar-Hashemi F, Samsami S, Chinichian S, Oghabian MA (2013) Aloe vera for prevention of radiation-induced dermatitis: A self-controlled clinical trial. Curr Oncol 20(4): e345-e348.
-
Byeon SW, Pelley RP, Ullrich SE, Waller TA, Bucana CD, et al. (1998) Aloe barbadensis extracts reduce the production of interleukin-10 after exposure to ultraviolet radiation. J Invest Dermatol 110(5): 811-817.
-
Rudolph KL, Chang S, Lee HW, Blasco M, Gottlieb GJ, et al. (1999) Longevity, stress response, and cancer in aging telomerase-deficient mice. Cell 96(5): 701-712.
-
Grace OM, Simmonds MSJ, Smith GF, Van Wyk AE (2008) Therapeutic uses of Aloe L. (Asphodelaceae) in southern Africa. J Ethnopharmacol 119(3): 604-614.
-
Miroddi M, Navarra M, Calapai F, Mancari F, Giofrè SV, et al. (2015) Review of clinical pharmacology of Aloe vera L. in the treatment of psoriasis. Phytother Res 29(5): 648-655.
-
Arunkumar S, Muthuselvam M (2009) Analysis of phytochemical constituents and antimicrobial activities of Aloe vera L. against clinical pathogens. World J Agric Res 5(5): 572-576.
-
Oyelami OA, Onayemi A, Oyedeji OA, Adeyemi LA (2009) Preliminary study of effectiveness of Aloe vera in scabies treatment. Phytother Res 23(10): 1482-1484.
-
Visuthikosol V, Chowchuen B, Sukwanarat Y, Sriurairatana S, Boonpucknavig V (1995) Effect of aloe vera gel to healing of burn wound a clinical and histologic study. J Med Assoc Thai 78(8): 403-409.
-
Panahi Y, Davoudi SM, Sahebkar A, Beiraghdar F, Dadjo Y, et al. (2012) Efficacy of Aloe vera/olive oil cream versus betamethasone cream for chronic skin lesions following sulfur mustard exposure: A randomized double-blind clinical trial. Cutan Ocul Toxicol 31(2): 95-103.
-
Bhalang K, Thunyakitpisal P, Rungsirisatean N (2013) Acemannan, a polysaccharide extracted from Aloe vera, is effective in the treatment of oral aphthous ulceration. J Altern Complement Med 19(5): 429-434.
-
Krishnaveni V, Aparna B (2014) Microencapsulation of copper enriched Aloe gel curative garment for atopic dermatitis. NISCAIR-CSIR, India. Indian J Tradit Know 13(4): 795-803.
-
Afzal I, Zia S, Kausar S, Hazrat A, Jan T, et al. (2020) Dose Response Relationship of Aloe vera to Cure Atopic Dermatitis in Rats. Dermatol Ther 33(4): e13376-e13376.
-
Rondas AALM, Schols JMGA (2017) Application of Medical Moisture Retention Cream (ALHYDRAN®), A New Option in the Treatment of Venous Eczema. J Gerontol Geriatr Res 6(395): 2.
-
Saija A, Tomaino A, Trombetta D, Pellegrino ML, Tita B, et al. (2003) ‘In vitro’ antioxidant and photoprotective properties and interaction with model membranes of three new quercetin esters. Eur J Pharm Biopharm 56(2): 167-174.
-
Chondrogianni N, Kapeta S, Chinou I, Vassilatou K, Papassideri I, et al. (2010) Anti-ageing and rejuvenating effects of quercetin. Exp Gerontol 45(10): 763-771.
-
Vicentini FT, Simi TR, Del Ciampo JO, Wolga NO, Pitol DL, et al. (2008) Quercetin in w/o microemulsion: In vitro and in vivo skin penetration and efficacy against UVB-induced skin damages evaluated in vivo. Eur J Pharm Biopharm 69(3): 948-957.
-
Vicentini FTMC, He T, Shao Y, Fonseca MJ, Verri Jr WA, et al. (2011) Quercetin inhibits UV irradiation-induced inflammatory cytokine production in primary human keratinocytes by suppressing NF-κB pathway. J Dermatol Sci 61(3): 162-168.
-
Choquenet B, Couteau C, Paparis E, Coiffard LJ (2008) Quercetin and rutin as potential sunscreen agents: Determination of efficacy by an in vitro method. J Nat Prod 71(6): 1117-1118.
-
Silverberg JI, Nelson DB, Yosipovitch G (2016) Addressing treatment challenges in atopic dermatitis with novel topical therapies. J Dermatolog Treat 27(6): 568-576.
-
Escobar-Chávez JJ, Díaz-Torres R, Rodríguez-Cruz IM, Domínguez-Delgado CL, Morales RS, et al. (2012) Nanocarriers for transdermal drug delivery. Res Rep Transdermal Drug Deliv 1: 3-17.
-
Jeevanandam J, San Chan Y, Danquah MK (2016) Nano-formulations of drugs: recent developments impact and challenges. Biochimie 128: 99-112.
-
Liu D, Hu H, Lin Z, Chen D, Zhu Y, et al. (2013) Quercetin deformable liposome: Preparation and efficacy against ultraviolet B induced skin damages in vitro and in vivo. J Photochem Photobiol B 127: 8-17.
-
Di Marzio L, Ventura CA, Cosco D, Paolino D, Di Stefano A, et al. (2016) Nanotherapeutics for anti-inflammatory delivery. J Drug Deliv Sci Technol 32: 174-191.
-
Takahashi M, Kitamoto D, Asikin Y, Takara K, Wada K (2009) Liposomes encapsulating Aloe vera leaf gel extract significantly enhance proliferation and collagen synthesis in human skin cell lines. J Oleo Sci 58(12): 643-650.
-
Tan Q, Liu W, Guo C, Zhai G (2011) Preparation and evaluation of quercetin-loaded lecithin-chitosan nanoparticles for topical delivery. Int J Nanomedicine 6: 1621-1630.
-
Krausz AE, Adler BL, Cabral V, Navati M, Doerner J, et al. (2015) Curcumin-encapsulated nanoparticles as innovative antimicrobial and wound healing agent. Nanomedicine 11(1): 195-206.
-
Satyavani K, Ramanathan T, Gurudeeban S (2011) Plant mediated synthesis of biomedical silver nanoparticles by using leaf extract of Citrullus colocynthis. Res J Nansci Nanotechnol 1(2): 95-101.
-
Sutthanut K, Lu X, Sripanidkulchai B, Yenjai C, Jay M (2009) Solid liquid nanoparticles for transdermal delivery of Kaempferia parviflora extracts. J Biomed Nanotechnol 5(2): 224-232.
-
Sandhya S, Chandra SJ, Vinod KR, Rao KNV, Banji D (2012) Preclinical studies of a novel polyherbal phyto-complex hair growth promoting cream. Asian Pac J Trop Biomed 2(1): S296-S304.
-
Momenkiaei F, Raofie F (2019) Preparations of Curcuma longa L. extract nanoparticles using supercritical solution expansion. J Pharm Sci 108(4): 1581-1589.
-
Patel RD, Singh SK, Singh S, Sheth NR, Gendle R (2009) Development and characterization of curcumin loaded transfersome for transdermal delivery. J Pharm Sci Res 1(4): 71.
-
Chinembiri TN, Gerber M, Du Plessis LH, Du Preez JL, Hamman JH, et al. (2017) Topical delivery of Withania somnifera crude extracts in niosomes and solid lipid nanoparticles. Pharmacogn Mag 13(Suppl 3): S663-S671.





