Review Article
Phytoconstituents and Biological Activities of Genus Artemisia (Asteraceae): A Review
6135
Views & Citations5135
Likes & Shares
The genus “Artemisia” is one of the largest and widely distributed genus of the plant family “Asteraceae”, comprising more than 400 accepted species. Due to the structurally diverse bioactive phytochemical constituents from the Artemisia species, this genus has been used as folk remedies in various treatments since ancient times. The genus contains various classes of secondary metabolites comprising alkaloids, flavonoids, coumarins, lignans, phenylpropanoids, terpenes, monoterpenes, terpenoids, sesquiterpenoids, sterols, phenolics, fatty acids, caffeoylquinic acids and acetylenes. Phytochemicals and extracts of Artemisia species exhibit diverse pharmacological activities including anti-malarial, anti-cancerous, anti-oxidant, anticoagulant activity, anti-parasitic, anti-inflammatory, antiulcerogenic, anti-viral activity, anti-microbial, anti-tumor and anti-diabetic activity. The present review compiles phytochemical constituents and various pharmacological activities of the Artemisia species.
The aim of this review is to bring together most of the information about the phytochemical constituents and pharmacological activities to attract researcher for further research in drug discovery.
Keywords: Asteraceae, Artemisia, Phytochemicals, Flavonoids, Alkaloids, Coumarins, Lignans NMR, Pharmacological activities
Abbreviations: NMR: Nuclear magnetic resonance; CDCl3: Deuterated chloroform; CD3OD: Deuterated methanol; DMSO-d6: Dimethyl sulfoxide-d₆
INTRODUCTION
Since ancient times, medicinal plants have been used in healthcare. A number of plants have been used in traditional medicine for various treatments. According to WHO about 80% of the world population used medicinal plants and relies on traditional remedies for their preliminary health care [1].
The aster family (Asteraceae), also called Compositae is one of the largest angiosperm families, consisting of more than 1,620 genera and 23,600 species of herbaceous plants, shrubs, and trees. The Asteraceae family also recognized as, ‘sunflower family’, ‘thistle family’ or ‘daisy family’. The family has a widespread distribution throughout the world, except Antarctica. The plants are characterized by their composite flower heads and one-seeded achene fruits. Members of this family possess medicinal properties and are used as traditional medicine due to their various phytoconstituents [2,3].
The word ‘Artemisia’ comes from the ancient Greek word ‘Artemis’ means The Goddess (the Greek Queen Artemisia) and ‘absinthium’ means Unenjoyable or without sweetness. The genus "Artemisia", is one of the largest and widely distributed genus belongs to the flowering plant family Asteraceae, comprises hardy herbaceous plants and small shrubs, distributed mainly in the temperate zones of Europe, Asia and North America [4,5]. The genus consisting over 500 diverse species, out of which 474 are accepted species names [6]. Various species of the genus are called by the common names include mugwort, wormwood, sagebrush, southernwood, slovenwood, sweet Annie, sagewort, tarragon [7]. Most of the Artemisia species found in the temperate sectors of northern hemisphere, but limited numbers of species are also found in the southern hemisphere of the world. However, its center of diversification is Central Asia [8]. Plants of this genus have been used in various treatment as folk remedies due to the presence of diverse bioactive phytochemical compound. Phytochemical investigation on Artemisia species revealed that the genus contains various classes of secondary metabolites comprising alkaloids, flavonoids, coumarins, lignans, phenylpropanoids, terpenes, monoterpenes, terpenoids, sesquiterpenoids, sterols, phenolics, fatty acids, caffeoylquinic acids and acetylenes etc. which are reported to possess various biological activities including antimicrobial, antioxidant, cytotoxic, insecticidal, [9,10] anti-malarial [11], anti-cancerous[12], anti-tumor[13], anthelmintic activity [14] , anti-diabetic [15], antiulcerogenic [16], anti-inflammatory [17] and anti-viral activity [18].
The aim of this paper is to compile and accumulate information about the phytochemical constituents and various pharmacological studies of the different species of Artemisia.
BOTANICAL DESCRIPTION
Habitat
Artemisia species are widely distributed in temperate regions of North America (Mexico, the United States, and Canada), the Mediterranean region, Asia, Africa, and Australia. The majority of species have been found in Asia, including China, Japan, Iran, India, and Turkey [19]. The genus is mostly found in temperate areas of the northern hemisphere, with just few species recorded from the southern hemisphere [20]. However, Central Asia is the center of diversification, with around 150 species in China, 50 species in Japan, and 35 species in Iran, while the speciation areas are North West America, Irano-Turanian, 29 species in Pakistani flora, and the Mediterranean region. From Africa and Europe, only few species have been recorded [21].
Artemisia is thought to have originated in the northwestern Asian mountain regions, probably from meso-thermic subarctic or semihumid forest steppe conditions near the Ural Mountains [22].
Taxonomic classification [23]
Kingdom : Plantae
Phylum : Magnoliophyta
Class : Magnoliopsida
Order : Asterales
Family : Asteraceae
Genus : Artemisia
Morphology
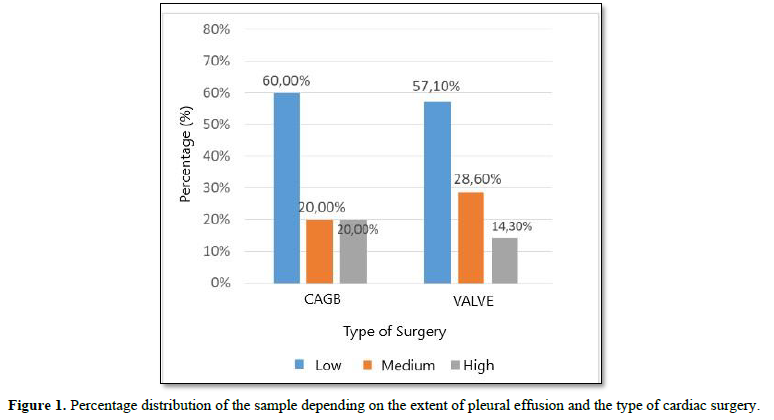
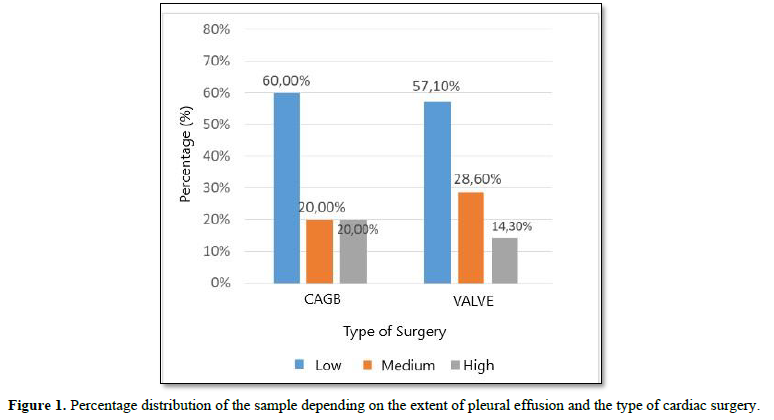
The leaves of the genus Artemisia are of various sizes, shapes, and textures, according to taxonomic characteristics. These are alternate and pinnatifid to pinnatisect. The inflorescence capitulum is small, often ellipsoid to ovate, arranged in the form of Paniculate Racemose, and contains tubular florets inserted on receptacle covered by involucral bracts, present in few rows. The corollas come in a variety of colors, including white, green, yellow, purplish, and sometimes brown [24] (Figure 1).
Cypsela may be oblique or terminal, with a scarred corolla, or elliptical, spheroidal, ovate, or compressed. Its color ranges from light brown to dark brown, and its surface can be glabrous or finely striated. Cypsela is 0.5-1.5×0.25-0.75mm in size [25]. Many species in this genus begin flowering at the end of the summer or during winter [26,27].
Ethnopharmacology
The genus Artemisia contains economically valuable plant species that have been used in pharmacology and various culinary applications for a long time. Artemisia extracts are used in a variety of biopharmaceutical products available on the market to treat a variety of ailments. In Chinese traditional medicine, Artemisia annua is used to treat malaria and chills. Decoctions of Artemisia herba- alba (Artemisia brevifolia Wall., Artemisia meritima L.) is used in traditional medicines to treat fever and nervous problems [28]. In addition, Artemisia absinthium (wormwood) has antiparasitic properties and is used to treat indigestion and anorexia. It is also used in gastric herbal preparations and in alcoholic beverages [29]. Among other species Artemisia biennis is used as antiseptics and spices. It's used to treat cuts, inflammation, and infections of the chest. Stomach cramps and painful menstruation are treated with the whole plant and seeds. It has been used to treat wounds and sores externally [30]. Artemisia argyi is a plant that grows primarily in China (where it is known as ai ye) and Japan (where it is known as gaiyou) and is used in herbal medicine to treat kidney, liver, and spleen disorder [31]. Essential oils are produced by the aerial parts of Artemisia scoparia (redstem wormwood) and are used as antibacterial, antipyretic, antiseptic, anti-cholesterolemic, insecticidal, purgative, diuretic, and gall bladder inflammation remedies [32].
Phytochemical Constituents
The genus Artemisia contains a rich source of structurally diverse secondary metabolites. Phytochemical investigation on Artemisia species showed the presence of various classes of phytochemicals comprising alkaloids, flavonoids, coumarins, lignans, phenylpropanoids, terpenes, monoterpenes, terpenoids, sesquiterpenoids, sterols, phenolics, fatty acids, caffeoylquinic acids and acetylenes etc. Among these the present review compiles and focuses mainly on flavonoids, alkaloids, coumarins and lignans.
Flavonoids isolated from the Artemisia species are compiled in Table 1 and the chemical structure of this isolated flavonoids compound are illustrated in Figure 2.






Alkaloids isolated from the Artemisia species are compiled in Table 2 and the chemical structure of this isolated alkaloids compound are illustrated in Figure 3











Alkaloids isolated from the Artemisia species are compiled in Table 2 and the chemical structure of this isolated alkaloids compound are illustrated in Figure 3





Coumarins isolated from the Artemisia species are compiled in Table 3 and the chemical structure of this isolated coumarins compound are illustrated in Figure 4.




Lignans isolated from the Artemisia species are compiled in Table 4 and the chemical structure of this isolated Lignans compound are illustrated in Figure 5.










Some terpenes isolated from the Artemisia species are compiled in Table 5 and the chemical structure of this isolated terpenes and their derivatives are illustrated in Figure 6.




NMR
Artemetin [33]
1H NMR (500 MHz, CDCl3): δ 7.69 (1H, dd, J=8.4Hz, 2.2Hz, H-6'), 7.66 (1H, d, J=2.2Hz, H-2'), 6.99 (1H, d, J=8.4Hz, H-5'), 6.86(1H, s, H-8), 3.99 (3H, s, 7-OMe), 3.97 (3H, s, 3-OMe), 3.97 (3H, s, 3'- or 4'-OMe), 3.86 (3H, s, 6-OMe), 3.79 (3H, s, 4' - or 3'-OMe), 2.52 (3H, s, 5-OAc).
Artemisinin [37]
1H NMR (300 MHz, CDCl3): δ 1.31(m, H-1), 2.00/1.44 (m, H-2a/H-2b), 2.43/2.06 (ddd, H-3a/H-3b), 5.86 (s, H-5), 1.75 (m, H-7), 1.85/1.05 (m, H-8a/H-8b), 1.75/1.05 (m, H-9a/H-9b), 3.39 (dq, H–H), 1.18(d, 7.0 Hz, H-13), 0.98 (d, 6.0 Hz, H-14) and 1.42 (s, H-15).
13C NMR (75 MHz, CDCl3): δ 172.1(C-1), 105.4(C-2), 93.7(C-3), 79.5 (C-4), 50.1(C-5), 44.9(C-6), 37.5(C-7), 35.9(C-8), 33.6(C-9), 32.9(C-10), 25.2(C-11), 24.8(C-12), 23.4(C-13), 19.8(C-14), 12.5(C-15).
Scopoletin [37]
1H NMR (300 MHz, CDCl3): δ 6.20 (d, 9.4 Hz, H-3) 7.51 (d, 9.4 Hz, H-4), 6.86 (s, H-5), 6.82(s, H-8) and 3.82 (s, OCH3).
Chrysosplenetin [37]
1H NMR (300 MHz, CDCl3): δ 6.50 (s, H-1) 7.66 (d,2,1 Hz, H-2′), 7.05 (d,8.6 Hz, H-5′), 7.71 (dd,8.6 Hz, 2.1 Hz, H-6′), 12.61 (s, 5-OH), 5.74 (s, 4′-OH), 3.86 (s, 3′-OCH3), 3.93 (s, 6-OCH3), 3.99 (s, 7-OCH3), 3.96 (s, 3′-OCH3).
13C NMR (75 MHz, CDCl3): δ 155.9(C-2), 105.40(C-2), 138.7(C-3), 178.9(C-4), 152.8(C-5), 132.3(C-6), 158.7(C-7), 90.3(C-8), 152.3(C-9), 106.6(C-10), 122.4(C-1′), 110.9(C-2′), 146.3(C-3′), 148.4(C-4′), 114.6(C-5′), 122.6(C-6′), 60.1(3-OCH3), 60.9(6-OCH3), 56.1(7-OCH3), 56.3(3′CH3).
Eupatin [37]
1H NMR (300 MHz, CDCl3): δ 12.75 (s,5-OH), 7.74 (dd,3.0Hz,12Hz, H-6′), 7.61(d,3.0Hz, H-2′), 7.01(d,12Hz, H-5′), 6.81(s, H-8), 4.00(CH3O-6), 3.88(CH3O-7), 3.81(4′-OCH3).
13C NMR (75 MHz, CDCl3): δ 148.2(C-4′), 144.9(C-3′), 121.2(C-6′), 115.5(C-2′), 115.3(C-1′), 90.8(C-8), 59.6(6-OCH3), 59.3(7-OCH3), 55.9(4′-OCH3).
Casticin [35]
1H NMR (500 MHz, DMSO-d6): δ 12.61 (1H, s, 5-OH), 9.90 (1H, s, 3-OH), 7.65 (1H, d, J = 2.0 Hz, H-2), 7.61(1H, dd, J = 8.0 Hz, 2.0 Hz, H-6), 6.94(1H, d, J = 8.0 Hz, H-5), 6.90(1H, s, H-5), 3.90 (3H, s, 7- OCH3), 3.85(3H, s, 4 - OCH3), 3.78(3H, s,3- OCH3), 3.71(3H, s, 6- OCH3).
13C NMR (500 MHz, DMSO-d6): δ 178.3(C-4), 158.7(C-7), 155.8(C-2), 151.8(C-9), 151.7(C-5), 150.0(C-3), 147.5(C-4), 137.8(C-3), 131.7(C-6), 122.4(C-1), 120.8(C-6), 115.7(C-2), 112.1(C-5), 105.6(C-10), 91.5(C-8), 60.1(6- OCH3), 59.8(3- OCH3), 56.6(7- OCH3),55.9(4- OCH3).
Artemisinin G [87]
1H NMR (400 MHz, CDCl3): δ 0.97(3H. d, J=6.3Hz), 1.19 (3H, d, J=7.1Hz), 2.15(3H. s), 3.15(IH, m), 3.93 (1H, m), 4.20 (IH, m), 6.63(1H, s).
13C NMR (90 MHz, CDCl3): δ 12.40, 20.26, 21.10, 24.22, 27.58, 30.82, 34.56 34.92, 46.59, 54.75, 69.14, 79.31, 92.94, 168.30, 171.50.
Quercetagetin 4'-methylether [34]
1H NMR (CD3OD): δ 7.80 (1H, d, J=2 Hz, C-2'), 7.65 (1H, dd, J=9 and 2 Hz, C-6'), 6.90 (1H, d, J=9 Hz, C-5'), 6.72 (1H, s, C-8), 4.01 (3H, s, C-4'-OMe).
2,2-Dihydroxy-6-methoxychromene [34]
1H NMR (CD3OD): δ 7.60 (1H, d, J=10 Hz, C-3), 7.18 (1H, d, J=2 Hz, C-5), 7.04 (1H, dd, J=6 and 2 Hz, C-7), 6.82 (1H, d, J=6 Hz, C-8), 6.31 (1H, d, J=l0 Hz, C-4), 3.86 (3H, s, C-6-OMe).
2,2,6-Trihydroxychromene [34]
1H NMR (CD3 OD): δ 7.48 (1H, d, J= 10Hz, C-3), 7.05 (1H, d, J= 2Hz, C-5), 6.90 (1H, dd, J=6 and 2 Hz, C-7), 6.72 (1H, d, J=6 Hz, C-8), 6.20 (IH, d, J=10 Hz, C-4).
2',4',5,7-tetradroxy-5',6-dimethoxyflavone [40]
1H NMR (300 MHz, DMSO-d6): δ 3.74 (3H, s, 5’- OCH3), 3.79 (3H, s, 6- OCH3), 6.55 (1H, s, H-3’), 6.61 (1H, s, H-8), 7.02 (1H, s, H-3), 7.37 (1H, s, H-6′), 9.99 (1H, s, 4’-OH), 10.33 (1H, s, 2’-OH), 10.38 (1H, s, 7-OH), 13.00 (1H, s, 5-OH).
13C NMR (75 MHz, DMSO-d6): δ 182.6 (C-4), 162.2 (C-2), 157.4 (C-7), 153.4 (C-2′), 153.1 (C-4′), 152.8 (C-5), 152.8 (C-9), 148.1 (C-3′), 131.5 (C-6), 112.1 (C-6′), 106.9 (C-3), 94.7 (C-8), 107.4 (C-1′), 104.8 (C-5′), 104.3 (C-10), 60.4 (3’- OCH3), 56.9 (6-OCH3).
Eupatilin [40]
1H NMR(300 MHz, DMSO-d6): δ 3.76 (3H, s, 6- OCH3), 3.85 (3H, s, 3’- OCH3), 3.87 (3H, s, 4’- OCH3 ), 6.63 (1H, s, H-8), 6.95 (1H, s, H-3), 7.10 (1H, d, J=3.0 Hz, H-2’), 7.55 (1H, d, J = 9.0 Hz, H-5’), 7.66 (1H, dd, J=9.0,3.0 Hz, H-6’), 7.66 (1H, s, H-3), 13,00 (1H, s, 5-OH), 10.69 (1H, s, 7-OH).
13C NMR (75 MHz, DMSO-d6): δ 182.6 (C-4), 163.8 (C-2), 157,8 (C-5), 153.2 (C-7), 152.9 (C-9), 152.6 (C-4’), 149.4(C-3’), 131.8 (C-6), 123,4 (C-1’), 120.5 (C-6’), 112.1 (C-2’), 109.8 (C-5’), 104.6 (C-10), 103.8 (C-3), 94.8 (C-8), 60.4 (6- OCH3), 56,3 (3´- OCH3) 56,2 (4´- OCH3).
Dimethoxycentaureidin [40]
1H NMR(300 MHz, DMSO-d6): δ 3.79 (3H, s, 6- OCH3), 3.92 (3H, s, 4’- OCH3), 6.65 (1H, s, H-8), 6.93 (1H, s, H-3), 6.95 (1H, d, J=9.0 Hz, H-5′), 7.60 (1H, d, J=2.0 Hz, H-2′), 7.58 (1H, dd, J=9.0,2.0 Hz, H-6′), 13.12 (1H, s, 5-OH), 9.99 (1H, s, 3’-OH), 10.71 (1H, s, 7-OH).
13C NMR (75 MHz, DMSO-d6) δ: 182.6 (C-4), 164.2 (C-2), 157.7 (C-7), 153.2 (C-5), 152.8 (C-9), 151.1 (C-3′), 148.1 (C-4′),131.8 (C-6), 122.0 (C-1′), 120.8 (C-6′), 116.2 (C-5′), 110.6 (C-2′), 104.5 (C-10), 103.2 (C-3), 94.8 (C-8), 60.5 (4’- OCH3), 56.4 (6- OCH3).
Cirsiliol [40]
1H NMR (300 MHz, DMSO-d6): δ 3.75 (3H, s, 6- OCH3), 3.95 (3H, s, 7- OCH3), 6.76 (1H, s, H-3), 6.90 (1H, d, J=9.0 Hz, H-5′), 6.93 (1H, s, H-8), 7.46 (1H, s, H-2’), 7.49 (1H, d, J=9.0 Hz, H-6′), 13.09 (1H, s, 5-OH), 8.32 (1H, s, 3’-OH), 8.27 (1H, s, 4’-OH).
13C NMR (75 MHz, DMSO-d6) δ: 182.6 (C-4), 164.7 (C-2), 159.0 (C-7), 153.0 (C-5), 152.8 (C-9), 150.4 (C-4′), 146.3 (C-3′), 132.3 (C-6), 121.8 (C-1′), 119.5 (C-6′), 116.4 (C-5′), 113.9 (C-2′), 105.5 (C-10), 103.1 (C-3), 91.9 (C-8), 60.5 (7- OCH3), 56.4 (6- OCH3).
Luteolin [42]
1H NMR (400 MHz, CD3OD): δ 6.22 (1H, d, J = 2.0 Hz, H-6), 6.45 (1H, d, J = 2.0 Hz, H-8), 6.55 (1H, s, H-3), 6.92 (1H, d, J = 8.8 Hz, H-5´), 7.39 (1H, d, J = 2.0 Hz, H-2´), 7.40 (1H, dd, J = 2.0, 8.8 Hz, H-6´).
Kaempferol [42]
1H NMR (400 MHz, CD3OD): δ 6.20 (1H, d, J = 2.0 Hz, H-6), 6.41 (1H, d, J = 2.0 Hz, H-8), 6.93 (2H, d, J = 8.4 Hz, H-3´,5´), 8.11 (2H, d, J = 8.4 Hz, H-2´, 6´).
Apigenin [42]
1H NMR (400 MHz, CD3OD): δ 6.22 (1H, d, J = 2.0 Hz, H-6), 6.47 (1H, d, J = 2.0 Hz, H-8), 6.61 (1H, s, H-3), 6.95 (2H, d, J = 8.8 Hz, H-3´, 5´), 7.87 (2H, d, J = 8.8 Hz, H-2´, 6´).
Scoparone [78]
1H NMR (400 MHz, CD3OD): δ 3. 87 (3H, s, 7- OCH3), 3.92 (3H, s, 6- OCH3), 6.26 (H, d, J=9.6 Hz, H-3), 7.88 (1H, d, J=9.6 Hz, H-4), 7.13 (1H, s, H-5), 6.98 (1H, s, H-8).
13C NMR (100 MHz, CD3OD): δ 56.9 (2x– OCH3), 163.8 (C-2), 110.0 (C-3), 145.9 (C-4), 113.6 (C-5),148.2 (C-6), 154.8 (C-7), 101.0 (C-8), 151.3 (C-9), 113.1 (C-10).
Isofraxidin [78]
1H NMR (400 MHz, CD3OD): δ 3.87 (3H, s, 7- OCH3), 3.92(3H, s, 6- OCH3), 6.26 (1H, d, J=9.4 Hz, H-3), 7.13 (1H, s, H-5), 7.88 (1H, d, J=9.4 Hz, H-4).
13C NMR (100 MHz, CD3OD): δ 56. 9 (2×– OCH3), 101.0 (C-8), 110.0 (C-3), 113.1 (C-10), 113.6 (C-5), 145.9 (C-4), 148.2(C-6), 151.3 (C-9), 154.8 (C-7), 163.8 (C-2).
6,7-dimethoxycoumarin [75]
1H NMR (500 MHz, CDCl3): δ 6.31 (1H, d, J = 9.5 Hz, H-3), 7.65 (1H, d, J = 9.5 Hz, H-4), 6.86 (1H, s, H-5), 6.88 (1H, s, H-8), 3.94 (3H, s, 6-OCH3), 3.97 (3H, s, 7-OCH3).
13C NMR (125 MHz, CDCl3): δ 161.5 (C-2), 113.6 (C-3), 143.3 (C-4), 107.9 (C-5), 146.3 (C-6), 152.8 (C-7), 100.0 (C-8), 150.0 (C-9), 111.4 (C-10), 56.4 (6-OCH3), 56.3 (7-OCH3).
6,7,8-trimethoxycoumarin [75]
1H NMR (500 MHz, CDCl3): δ 6.06 (1H, d, J = 9.0 Hz, H-3), 7.52 (1H, d, J = 9.0 Hz, H-4), 7.30 (1H, s, H-5), 3.88 (3H, s, 6-OCH3), 3.86 (3H, s, 8-OCH3), 3.82 (3H, s, 7-OCH3).
13C NMR (125 MHz, CDCl3): δ 165.4 (C-2), 115.5 (C-3), 140.3 (C-4), 114.9(C-5), 145.0 (C-6), 125.1 (C-7), 133.5 (C-8), 134.4 (C-9), 120.7 (C-10), 56.4 (6-OCH3), 56.1 (8-OCH3), 55.8 (7- OCH3).
6-hydroxy-7-methoxycoumarin [75]
1H NMR (500 MHz, CDCl3): δ 6.31 (1H, d, J = 9.5 Hz, H-3), 7.64 (1H, d, J = 9.5 Hz, H-4), 6.93 (1H, s, H-5), 6.85 (1H, s, H-8), 3.91 (3H, s, 7-OCH3).
13C NMR (125 MHz, CDCl3): δ 161.6 (C-2), 113.5 (C-3), 143.5 (C-4), 108.3 (C-5), 147.3 (C-6), 152.0(C-7), 103.0 (C-8), 153.0 (C-9), 113.4 (C-10), 56.5 (7-OCH3).
4-hydroxylacetophenone [75]
1H NMR (500 MHz, CDCl3): δ 7.93 (2H, d, J = 8.5 Hz, H-2,6), 6.91 (2H, d, J = 8.5 Hz, H-3,5), 2.58 (3H, s, - CH3).
13C NMR (125 MHz, CDCl3): δ 130.4 (C-1), 131.0 (C-2), 115.3 (C-3), 160.1 (C-4), 115.3 (C-5), 131.0 (C-6), 197.9 (C=O), 26.3 (-CH3).
4-hydroxy-5-methoxylacetophenone [75]
1H NMR (500 MHz, CDCl3): δ 7.59 (1H, d, J = 2.0 Hz, H-2), 6.98 (1H, d, J = 8.0 Hz, H-5), 7.62 (1H, d, J = 8.0, 2.0 Hz, H-6), 3.90 (3H, s, -OCH3), 2.51 (3H, s, CH3).
13C NMR (125 MHz, CDCl3): δ 129.9 (C-1), 111.1 (C-2), 147.0 (C-3)146.8(C-4), 114.4 (C-5), 126.9 (C-6), 190.3 (C=O), 56.8 (-OCH3), 26.3 (-CH3).
4-hydroxybenzaldehyde [75]
1H NMR (500 MHz, CDCl3): δ 7.82 (2H, d, J = 8.5 Hz, H-2,6), 7.02 (2H, d, J = 8.5 Hz, H-3,5), 9.85 (1H, s, -CHO).
13C NMR (125 MHz, CDCl3): δ 139.3 (C-1), 132.5 (C-2), 116.0 (C-3), 162.0 (C-4), 116.0 (C-5), 132.5 (C-6), 191.3 (-CHO).
4-hydroxy-5-methoxybenzaldehyde [75]
1H NMR (500 MHz, CDCl3): δ 7.43 (1H, brs, H-2), 7.05 (1H, d, J = 8.5 Hz, H-5), 7.45 (1H, brd, J = 8.5 Hz, H-6), 9.83 (1H, s, -CHO), 3.99 (3H, s, -OCH3).
13C NMR (125 MHz, CDCl3): δ 129.9 (C-1), 108.8 (C-2), 151.7 (C-3), 147.2 (C-4), 114.4 (C-5), 127.6 (C-6), 191.0 (C=O), 56.1 (-OCH3).
4,5-dihydroxybenzaldehyde [75]
1H NMR (500 MHz, CDCl3): δ 7.44 (1H, d, J = 2.0 Hz, H-2), 6.96 (1H, d, J = 8.0 Hz, H-5), 7.46 (1H, brd, J = 8.0, 2.0 Hz, H-6), 9.85 (1H, s, -CHO).
13C NMR (125 MHz, CDCl3): δ 129.8 (C-1), 108.9 (C-2), 146.8 (C-3), 146.2 (C-4), 114.3 (C-5), 127.7 (C-6), 191.0 (C=O).
Rupestine A [57]
1H NMR (400 MHz, CDCl3): δ 6.92 (d, J =8.0 Hz, H-3), 7.31 (d, J=8.0 Hz, H-4), 3.04 (m, H-5), 1.76 – 1.84 (m, Ha-6, Hb-6), 1.76 – 1.84 (m, Ha-7, Hb-7), 2.75 – 2.85 (m, H-8), 3.15 (d, J= 13.6 Hz, Ha-9), 3.29 (dd, J= 14.4,10 Hz, Hb-9), 5.58 (s, Ha-14), 6.18 (s, Hb-14), 2.50 (s, CH3-15), 1.30 (d, J=7.2 Hz, CH3-16), 4.21 (q, J=7.2 Hz, CH2-1’), 1.31 (t, J= 7.2 Hz, CH3-2’).
13C NMR (100 MHz, CDCl3): δ 154.63 (C-2), 121.04 (C-3), 136.79 (C-4), 37.94 (C-5), 33.03 (C-6), 31.68 (C-7), 38.10 (C-8), 43.78 (C-9), 158.61 (C-10), 137.61 (C-11), 146.45 (C-12), 167.04 (C-13), 122.86 (C-14), 23.86 (C-15), 18.33 (C-16), 60.66 (C-1'), 14.22 (C-2').
Rupestine B [57]
1H NMR (400 MHz, CDCl3): δ 6.98 (d, J=8 Hz, H-3), 7.38 (d, J= 8 Hz, H-4), 2.99 – 3.04 (m, H-5), 1.22 – 1.27 (m, Ha-6), 1.82 – 1.94 (m, Hb-6), 1.82 – 1.94 (m, Ha-7), 1.98 – 2.08 (m, Hb-7), 2.47 – 2.60 (m, H-8), 3.09 (d, J=14 Hz, Ha-9), 3.24 (dd, J=14, 10.8 Hz, Hb-9), 2.52 (q, J= 7.2 Hz, CH2-13), 1.04 (t, J=7.2 Hz, Ha-14), 2.51 (s, CH3-15), 1.31 (d, J=7.6 Hz, CH3-16).
13C NMR (100 MHz, CDCl3): δ 154.39 (C-2), 121.17 (C-3), 132.48 (C-4), 34.79 (C-5), 35.08 (C-6), 33.22 (C-7), 48.60 (C-8), 39.73 (C-9), 159.36 (C-10), 137.90 (C-11), 213.71 (C-12), 34.38 (C-13), 7.83 (C-14), 23.79 (C-15), 20.38 (C-16).
Rupestine C [57]
1H NMR (400 MHz, CDCl3): δ 6.94 (d, J=7.6 Hz, H-3), 7.33 (d, J=7.6 Hz, H-4), 2.95 – 3.04 (m, H-5), 1.72 – 1.88 (m, Ha-6), 1.72 – 1.88 (m, Ha-7), 2.00 – 2.10 (m, Hb-7), 2.67 – 2.75 (m, H-8), 3.16 – 3.24 (m, Ha-9), 3.31 – 3.41 (m, Hb-9), 2.60 (q, J=7.2 Hz, CH2-13), 1.02 (q, J=7.2 Hz, Ha-14), 2.50 (s, CH3-15), 1.31 (d, J=7.6 Hz, CH3-16).
13C NMR (100 MHz, CDCl3): δ 154.63 (C-2), 121.42 (C-3), 136.59 (C-4), 37.65 (C-5), 32.11 (C-6), 28.40 (C-7), 48.50 (C-8), 39.57 (C-9), 157.63 (C-10), 138.14 (C-11), 213.38 (C-12), 34.29 (C-13), 7.76 (C-14), 23.56 (C-15), 18.85 (C-16).
Rupestine D [57]
1H NMR (400 MHz, CDCl3): δ 7.00 (d, J=8.0 Hz, H-3), 7.40 (d, J= 8.0 Hz, H-4), 2.94 - 3.04 (m, H-5), 1.23 - 1.30 (m, Ha-6), 1.82 - 1.94 (m, Hb-6), 1.82 - 1.94 (m, Ha-7), 2.04 – 2.11 (m, Hb-7), 2.54 - 2.60 (m, H-8), 3.13 - 3.28 (m, Ha-9), 2.23 (s, CH2-13), 2.51 (s, Ha-14), 1.35 (d, J= 7.2 Hz, CH3-15).
13C NMR (100 MHz, CDCl3): δ 154.36 (C-2), 121.24 (C-3), 132.60 (C-4), 34.76 (C-5), 34.96 (C-6), 32.92 (C-7), 49.47 (C-8), 39.43 (C-9), 159.05 (C-10), 137.90 (C-11), 211.07 (C-12), 28.49 (C-13), 23.71 (C-14), 20.32 (C-15).
Caruilignan C [85]
1H NMR (500 MHz, CDCl3) δ: 6.51 (s, 2H, H2,6), 4.95 (d, 1H, J=6.0 Hz, H7), 4.53 (d, 1H, J= 9.5 Hz, Hβ9), 4.10 (dd, 1H, J1=8.0 Hz, J2=9.5 Hz, H β9′), 3.98 (dd, 1H, J1= 6.5 Hz, J2 =9.5 Hz, Hα9), 3.88 (s, 6H, 3,5OCH3), 3.85 (s, 3H, 4OCH3), 3.83 (dd, 1H, overlapped, Hα9′), 3.39 (m, 1H, H8′).
13C NMR (125 MHz, CDCl3) δ: 178.6 (C7′), 153.5 (C3,5), 137.4 (C4), 132.1 (C1), 102.7 (C2,6), 84.2 (C7), 70.9 (C9), 68.4 (C9′), 60.9 (4OCH3), 56.2 (3,5OCH3), 45.9 (C8), 43.5 (C8′).
7βCaruilignan C [85]
1H NMR (500 MHz, CDCl3) δ: 6.57 (s, 2H, H2,6), 4.62 (d, 1H, J=7.0 Hz, H7), 4.52 (dd, 1H, J1=6.5 Hz, J2=9.5 Hz, Hβ9), 4.40 (t, 1H, J= 9.0 Hz, Hβ9′), 4.37 (dd, 1H, J1=2.0 Hz, J2=9.8 Hz, Hα9), 4.22 (dd, 1H, J1=4.0 Hz, J2=9.0 Hz, Hα9′), 3.88 (s, 6H, 3′,5′OCH3), 3.85 (s, 3H, 4′OCH3), 3.46 (dt, 1H, J1=4.0 Hz, J2=9.0 Hz, J39.0 Hz, H8′), 3.14 (m, 1H, H8).
13C NMR (125 MHz, CDCl3) δ: 178.0 (C7′), 153.6 (C3,5), 138.0 (C4), 134.5 (C1), 102,8 (C2,6), 86.2 (C7), 70.2 (C9′), 69.8 (C9), 60.8 (4OCH3), 56.2 (3,5OCH3), 48.5 (C8), 46.0 (C8′).
Yangambin [85]
1H NMR (500 MHz, CDCl3) δ: 6.58 (s, 4H, H2,6,2′,6′), 4.76 (d, 2H, J =4.0 Hz, H7,7′), 4.32 (dd, 2H, J1=7.0 Hz, J2=9.0 Hz, Hα9,9′), 3.94 (dd, 2H, J1=3.0 Hz, J2=9.0 Hz, Hβ9,9′), 3.88 (s, 12H, 3,3′,5,5′OCH3), 3.85 (s, 6H, 4,4′OCH3), 3.11 (m, 2H, H8,8′).
13C NMR (125 MHz, CDCl3) δ: 153.4 (C3,5,3′,5′), 136.7 (C1,1′), 137.5 (C4,4′), 102.8 (C2,6,2′,6′), 85.9 (C7,7′), 72.0 (C9,9′,60.8 (4,4′OCH3), 56.2 (3,5,3′,5′OCH3), 54.3 (C8,8′).
Diayangambin [85]
1H NMR (500 MHz, CDCl3) δ: 6.61 (s, 4H, H2,6,2′,6′), 4.92 (d, 2H, J=4.5 Hz, H7,7′), 3.89 (s, 12H,3,5,3′,5′OMe), 3.86 (s,6H, 4,4′OMe), 3.75 (dd, 2H, J1=1.5 Hz, J2=9.5 Hz, Hα9,9′), 3.60 (dd, 2H, J1=7 Hz, J2=10 Hz, Hβ9,9′), 3.21 (m, 2H, H8,8′).
13C NMR (125 MHz, CDCl3) δ: 153.2 (C3,5,3′,5′), 137.1 (C1,1′), 134.6 (C4,4′), 103.2 (C2,6,2′,6′), 84.1 (C7,7′), 68.9 (C9,9′), 60.9 (4,4′OMe), 56.1 (3,5,3′,5′OMe), 49.4 (C8,8′).
Epiyangambin [85]
1H NMR (500 MHz, CDCl3) δ: 6.60 (s, 2H, H2,6), 6.59 (s, 2H, H2′,6′), 4.87 (d, 1H, J = 5.5 Hz, H7), 4.45 (d, 1H, J =7.0 Hz, H7′), 4.17 (d, 1H, J =9.5 Hz, Hβ9′), 3.91 (m, 2H, Hα9,9′), 3.89-3.85 (m, 18H, 3,4,5,3′,4′,5′OMe), 3.37 (m, 1H, H8), 3.36 (m, 1H, Hβ9), 2.93 (m, 1H, H8′).
13C NMR (125 MHz, CDCl3) δ: 153.4 (C3′,5′), 153.2 (C3,5), 137.6 (C4′), 137.0 (C4), 136.8 (C1′), 134.0 (C1), 103.0 (C2′,6′), 102.6 (C2,6), 87.8 (C7′), 82.2 (C7), 71.1 (C9′), 69.8 (C9), 60.9 (4′OMe), 60.8 (4OMe), 56.2 (3,5,3′,5′OMe), 54.5 (C8′), 50.0 (C8).
Sesartemin [85]
1H NMR (500 MHz, CDCl3) δ: 6.57 (s, 2H, H2,6), 6.55 (d, 1H, J=1.5 Hz, H6′), 6.53 (d, 1H, J=1.5 Hz, H2′), 5.95 (s, 2H, OCH2O), 4.72 (d, 2H, J=4.5 Hz, H7,7′), 4.29 (dd, 1H, J1=6.7 Hz, J2=9.2 Hz, Hα9), 4.26 (dd, 1H, J1=6.7 Hz, J2=9.2 Hz, Hα9′), 3.92 (dd, 1H, J1=3.6 Hz, J2=9.2 Hz, Hβ9), 3.91 (s, 3H,5′OMe), 3.90 (dd, 1H, J1=3.6 Hz, J2=9.2 Hz, Hβ9′), 3.87 (s, 6H, 3,5OMe), 3.83 (s, 3H, 4OMe), 3.07 (m, 2H, H8,8′).
13C NMR (125 MHz, CDCl3) δ: 153.4 (C3,5), 149.1 (C3′), 143.4 (C5′), 137.4 (C4), 136.7 (C1), 135.7 (C1′), 134.6 (C4′), 105.5 (C6′), 102.8 (C2,6), 101.4 (OCH2O), 100.0 (C2′), 85.9 (C7′), 85.7 (C7), 71.9 (C9), 71.7 (C9′), 60.8 (4OMe), 56.6 (5′OMe), 56.1 (3,5OMe), 54.3 (C8,8′).
(+) Arborone [85]
1H NMR (500 MHz, CDCl3) δ: 7.43 (s, 2H, H2,6), 6.55 (s, 2H, H2′,6′), 5.03 (d, 1H, J=6.0 Hz, H7′), 4.44 (t, 1H, J=8.0 Hz, Hβ9), 4.33 (d, 1H, J1=2.8 Hz, J2=5.6 Hz, J3=8.0 Hz, H8), 4.26 (d, 1H, J1=2.8 Hz, J2=8.0 Hz, Hα9), 3.94 (s, 3H, 4OMe), 3.93 (s, 6H, 3,5OMe), 3.87 (s, 6H, 3′,5′OMe), 3.84 (s, 3H, 4′OMe), 3.44 (d, 2H, J=6.8 Hz, H9′), 2.91 (m, 1H, H8′).
13C NMR (125 MHz, CDCl3) δ: 198.5 (C7), 153.4 (C3,5), 153.2 (C3′,5′), 143.0 (C4), 137.1 (C4′), 133.6 (C1′), 131.3 (C1), 106.4 (C2,6), 102.5 (C2′,6′), 81.6 (C7′), 69.1 (C 9), 62.0 (C9′), 61.0 (4OMe), 60.9 (4′OMe), 56.4 (3,5OMe), 56.2 (3′,5′OMe), 49.6 (C8′), 48.8 (C8).
Syringaresinol [85]
1H NMR (500 MHz, CDCl3) δ: 6.59 (s, 4H, H2,6,2′,6′), 5.52 (brs, 2H, 4,4′OH), 4.74 (d, 2H, J=4.0 Hz, H7,7′), 4.29 (dd, 2H, J1=6.5 Hz, J2=8.5 Hz, Hβ9,9′), 3.92 (dd, 2H, J1=2.9 Hz, J2=8.5 Hz, Hα9,9′), 3.90 (s, 12H, 3,5,3′,5′OMe), 3.10 (m, 2H, H8,8′).
13C NMR (125 MHz, CDCl3) δ: 147.1 (C3,5,3′,5′), 134.3 (C4,4′), 132.1 (C1,1′), 102.7 (C2,6,2′,6′), 86.0 (C7,7′), 71.8 (C9,9′), 56.4 (3,5,3′,5′OMe), 54.3 (C8,8′).
Epiashchantin [85]
1H NMR (500 MHz, CDCl3) δ: 6.78-6.88 (m, 3H, H2′,5′,6′), 6.59 (s, 2H, H2,6), 5.96 (s, 2H, OCH2O), 4.86 (d, 1H, J=5.5 Hz, H7), 4.44 (d, 1H, J=7.0 Hz, H7′), 4.13 (dd, 1H, J1=1.4 Hz, J2=9.5 Hz, Hβ9′), 3.89 (s, 6H, 3,5OMe), 3.86 (s, 3H, 4OMe), 3.85 (m, 2H, Hα9,9′), 3.36 (m, 1H, H8), 3.34 (m, 1H, Hβ9), 2.89 (m, 1H, H8′).
13C NMR (125 MHz, CDCl3) δ: 153.2 (C3,5), 148.0 (C3′), 147.2 (C4′), 136.9 (C4), 135.1 (C1′), 134.0 (C1), 119.5 (C6′), 108.2 (C5′), 106.5 (C2′), 102.6 (C2,6), 101.0 (OCH2O), 87.6 (C7′), 82.2 (C7), 71.0 (C9′), 69.7 (C9), 60.9 (4OMe), 56.2 (3,5OMe), 54.5 (C8′), 50.1 (C8).
PHARMACOLOGICAL ACTIVITY
Antioxidant activity
The antioxidant properties of plant extracts are primarily due to their phenolic compounds/flavonoids. An antioxidant activity of A. Vulgaris has been studied in vitro by free radical scavenging activity. The radical scavenging activity of methanolic extract of A. vulgaris (MEAV) leaves was determined by Calorimetric assay using 2,2-diphenyl-1-picrylhydrazyl (DPPH) according to the method of Blois with a slight modification. This study found that the percentage inhibition of MEAV extract was 68.06% at 60 μg/ml concentrations comparable to that of ascorbic acid (93.53%). The results showed a concentration dependent DPPH radical scavenging property, that estimated that the inhibition percentage was also increase with increase in concentration of MEAV, it showed that methanolic extract of A. vulgaris (MEAV) leaves has a potential antioxidant activity. In order to confirm the antioxidant activities, the plant extract was further analyzed by reducing power assay. where it was found that the ferric reducing power of MEAV was 0.95 ± 0.05 at100 μg/ml concentration comparable to ascorbic acid (1.04 ± 0.05). It showed that the tested extract has ability to transform the ferric ion (Fe3+) to ferrous ion (Fe2+) as reducing power with the increase of concentration of the extract [94]. Another study investigated the methanolic extract of A. absinthium aerial part at flowering stage and reported to have DPPH radical-scavenging activity [95].
The methanolic extracts of eight Artemesia sp. were investigated to evaluate potential antioxidant activity. This investigation reported that the extract of A. keiskeana, A. selengensis, A.capillaries, A.japonica, A scoparia, A stolonifera, A.montana, A.sylvatica showed Potent antioxidant activity in DPPH/ ABTS (2,2'-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) radical quenching activity [96].
Anticancer activity
Hye-Yeon Han and his colleagues were investigated the anticancer properties of a flavonoid compound jaceosidin from A. princeps using MTT assay. Their investigation has reported that jaceosidin selectively inhibits OSCC (oral squamous cell carcinoma) cell proliferation by inducing caspase-dependent apoptosis and inhibiting the Akt pathway by blocking Akt phosphorylation in OSCC cells. The study also demonstrates that jaceosidin does not show any effect on normal epithelial keratinocyte cells [52].
Methanolic extract from A. capillaris, A. sylvatica and A. selengensis also has been reported to shows anticancer activity [97-100]. Artemisinin, the active ingredient of A. annua, showed cell toxicity against human lymphoid leukemia (Molt-4) cells [101]. An in vitro study of ethanol extract of A. kulbadica, A. diffusa, A. sieberi, A. santolina and A. turanica against HepG-2 and Hep-2 cell lines were investigated. Results shown a concentration-dependent toxicity for all the extracts and the overall toxicity on HepG-2 cells are more than that on Hep-2 cells [102].
Anticoagulant activity
β-sitosterol and a known compound 2-(3,4-dimethoxyphenyl)-6-methoxy-4-oxo-4H-chromene-5,7-dicarboxylic acid was isolated from A. argyi for the first time in 1992, and both were shown to inhibit platelet aggregation [103]. In vitro anticoagulation activities of two newly purified flavonoids, eupatilin 7-O-β-D-glucopyranoside and 5,6,2′,4′-tetrahydroxy-7,5′-dimethoxyflavone, were recently investigated [104]. Both compounds retarded blood clotting by extending thrombin time (TT) and prothrombin time (PT), according to the findings. The anticoagulant property of A. argyi essential oil (AAEO) was confirmed in vivo by using an ice water bath to create an acute blood stasis rat model. AAEO decreased the blood viscosity of low, medium, and high shear rates at a skin administration dosage of 0.125–0.50 mL/kg. Additionally, this behavior has been linked to the ability to reduce erythrocyte aggregation [105].
Anti-inflammatory activity
A study was carried out to investigate the anti-inflammatory activity of three eudesmanolides compound from Artemisia burrelieri. This study has tested the anti-inflammatory effect of three eudesmanolides, barrelierin, artemalin and barrelin, isolated from aerial parts of A. burrelieri by studying their influence on carrageenan-induced rat paw oedema. According to the findings the percentage inhibition of barrelin was 33% at 15 mg/kg, more than 50% at 30mg/kg, and about 80% at 90 mg/kg. On the other hand, compound barrelierin and artemalin showed similar activity, but appears to be less potent, since with the lowest and highest doses the reduction of the inflammation was about 15% and 40%, respectively. This demonstrates that the compounds were reduced the inflammation in a dose-dependent manner [17]. Inhibition of nitrite synthesis in lipopolysaccharide (LPS)-stimulated macrophage cultures were investigated to assess the extracts' anti-inflammatory activity. In the presence of LPS, methanolic extracts of A. stolonifera, A. selengensis, A. capillaris, and A. keiskeana were found to reduce nitric oxide production at higher concentrations than control cells [97]. Methanolic leaf extract of A. vulgaris were also assessed to evaluate anti-inflammatory activity in wister albino rats by cotton pellet granuloma method. The result revealed that A. vulgaris extract possess a significant anti-inflammatory activity [106].
Antimalarial Activity
The aqueous, cold alcoholic and hot alcoholic extract of Artemisia absinthium was conducted to tested their antimalarial activity in vitro. The result of in vitro assay showed 35%, 55% and 21% inhibition in growth of Plasmodium falciparum, respectively at 2.00 mg/ml [107]. Another in vivo study was undertaken to investigate the antimalarial activity of ethanolic leaf extract from A. vulgaris against the P. berghei murine malaria model in terms of antiparasitic activity. The assay revealed that the leaf extract possesses potent antimalarial action [108]. The various organic (n-hexane, chloroform, petroleum ether, ethanol, methanol and aqueous) leaf extracts of A. nilagirica were assayed for antimalarial activity against P. falciparum FCR-3 strain. It was observed that, all tested leaf extracts showed a significant IC50 value [109]. The dichloromethane extract of A. armeniaca, A. aucheri and A. ciniforms was also investigated and reported to has antimalarial activity [109-114]. Another study revealed that by potentiating artemisinin activity the hydro alcoholic and aqueous extracts of A. annua L. showed antimalarial activity on plasmodium [115].
Antifungal and Antibacterial activity
The antibacterial and antifungal activity of ethanolic extracts of A. abrotanum and A. pallens against both gram positive and gram-negative bacteria was tested using the cup plate method. These extracts showed maximum zone of inhibition against Pseudomonas cepacia (28.6mm) and Bacillus stearothermophilus (27.6mm) respectively. The antifungal activity of both plant extracts was maximum against Trichosporon beigelii (17mm). These findings indicate that A. abrotanum and A. pallens ethanolic extracts have antibacterial and antifungal properties [116]. The antifungal and antibacterial activities of essential oils isolated from A. absinthium, A. dracunculus, A. santonicum, and A. spicigera (20 L/Petri dish) were tested against phytopathogenic fungal species and bacterial strains. This extract exhibited significant antifungal activity and antibacterial activity against microbial growth [117]. Three Gram positive bacteria, Staphylococcus aureus, Enterococcus faecalis, Bacillus cereus, and three Gram negative bacteria, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Escherichia coli, were tested to evaluate the antibacterial activity of ethanol extract of A. nilagirica. In terms of zone of inhibition, the results revealed that the extract has good antibacterial activity [118]. An antibacterial analysis of methanolic extract of A. campestris was performed, and the extract was found to have antibacterial properties [119,120]. The antibacterial properties of water extracts of A. annua have been studied, and the results indicate that the water extracts have stronger antibacterial properties [121].
Antitumor Activity
The methanolic extracts of the aerial parts of A. argyi were investigated for antitumor activity. The study showed that the compound 5,6,4'-trihydroxy-7,3'-dimethoxyflavone isolated from extract inhibit proliferation of a couple of tumor cell lines [122]. Flavonoids of A. absinthium, A. sieversiana and A. xanthochroa were assessed for antitumor activity in mice with melanoma 16, they possessed a slight inhibitory effect on Pliss lymphosarcoma in rats [123]. Ethyl acetate extract of A. indica also have been reported to showed antitumor activity [124].
Antiviral Activity
Hot water extract of A. capillaris were investigated and reported to possess antiviral activity against enterovirus 71(EV71) [98]. Artemisinin used in the treatment of malaria have been reported to have broad spectrum of potential antiviral effect. Artemisinin from A. annua give antiviral effect against Bovine Viral Diarrhoea Virus (BVDV) [18]. Other’s artemisinin derivatives such as arteannuin B is a structural derivative of artemisinin that reported to showed an anti-SARS-CoV-2 effect in vitro [125]. An In vitro study of antiviral activity of subset extracts from A. incana, A. chamaemelifolia, A. campesteris, A. fragrans, A. annua, A. vulgaris, and A. persica was investigated against Herpes Simplex virus type 1 (HSV1). Results showed that the extracts of aerial parts of A. annua had the highest anti-herpetic activity while those of A. chamaemelifolia showed the lowest activity [126].
Antidiabetic Activity
Antidiabetic study was carried out on the water and alcoholic extracts of A. judaica in diabetic rats. The result showed that oral administration of all doses of the aqueous and ethanolic extracts produced significant decrease in blood glucose level when compared to the control diabetic group [125]. Oral administration of an aqueous extract (0.39 g/kg) of the aerial parts of A. herba alba to normoglycemic and to alloxandiabetic rabbits was investigated and found to have significant hypoglycemic activity, which was consistent and time-dependent [126].
Another study used an aqueous extract of the aerial parts of the A. herba alba plant on diabetic rats and rabbits weighing 0.39 g/kg body weight. In this research these extracts also demonstrated a substantial reduction in blood glucose levels [127]. The anti-diabetic properties of petroleum ether, ethyl acetate, methanol, and hydroethanolic extracts of A. amygdalina were investigated in diabetic rats. The result confirms that the extract was significantly reduced glucose levels in diabetic rats [128]. According to a study, the methanolic leaf extract of A. absinthium showed possible antidiabetic activity against hyperglycemia and hypoinsulinemia in experimental Streptozotocin (STZ) induced diabetic rats [129].
Antiulcerogenic activity
The compounds artemisinin, dihydro-epideoxyarteannuin B and deoxyartemisinin obtained from ethanolic extract of A. annua were tested on ethanol and indomethacin induced ulcer models. The result indicated that the extract showed an inhibitory effect on the ulcerative lesion index in all experimental models tested, in rats [16]. Another study was undertaken to investigate the protective effect of A. campestris aqueous extract on aspirin-induced gastric ulceration. The result showed that the extract possesses potent antiulcer activity [130-132].
CONCLUSION
The genus Artemisia (Asteraceae) is a rich source of bioactive secondary metabolites. Species of this genus possess potential sources of pharmacological activity. Phytochemical investigation on Artemisia species revealed that the genus contains various classes of secondary metabolites with promising pharmacological activity. Terpenoids, flavonoids, coumarins, alkaloids, lignans caffeoylquinic acids and sterols constitute are major classes of phytoconstituents of the genus. The present review emphasizes the phytochemical constituents, pharmacological activities and NMR of structurally diverse phytochemicals. This review concluded that the presence of structurally diverse bioactive phytochemical constituents may attract the researchers for further research in new drug lead secondary metabolites from the genus. The included NMR of different phytochemical compound obtained from Artemisia species may help the researcher to elucidate structures.
- Rauf A, Jehan N (2015) The Folkloric Uses of Medicinal Plants in Public Health Care. pp: 1-12.
- Petruzzello M (2018) List of plants in the family Asteraceae. Encyclopedia Britannica. Available online at: https://www.britannica.com/topic/list-of-plants-in-the-family-Asteraceae-2040400
- Barreda V, Palazzesi L, Tellería M, Olivero E, Raine J (2015) Early evolution of the angiosperm clade Asteraceae in the Cretaceous of Antarctica. Proc Natl Acad Sci U S A 112(35): 10989-10994.
- Watson LE, Bates PL, Evans TM, Unwin MM, Estes JR (2002) Molecular phylogeny of Subtribe Artemisiinae (Asteraceae), including Artemisia and its allied and segregate genera. BMC Evol Biol 2: 17.
- Mehrdad I, Seyed EA, Meysam MS (2007) Detection of sesquiterpene lactones in ten Artemisia species population of Khorasan provinces. Iran J Basic Medi Sci 10: 183-188.
- Artemisia (2012) Available online at: http://www.theplantlist.org/browse/A/Compositae/Artemisia/
- Kapustina LA, Torrell M, Vallès J (2001) Artemisia communities in arid zones of Uzbekistan (Central Asia). In E. D. McArthur, Fairbanks D J (Eds.) comps. Shrubland ecosystem genetics and biodiversity: Proceedings; 2000 June 13-15; Provo, UT. Proc. RMRS-P-21: 104-112. Ogden, UT: US Department of Agriculture, Forest Service, Rocky Mountain Research Station.
- Vallès J, McArthur ED (2001) Artemisia systematics and phylogeny: Cytogenetic and molecular insights. USDA Forest Service Proceedings 21: 67-74.
- Tan RX, Zheng WF, Tang HQ (1998) Biologically active substances from the genus Artemisia. Planta Med 64: 295-302.
- Maham M, Moslemzadeh H, Jalilzadeh-Amin G (2014) Antinociceptive effect of the essential oil of tarragon (Artemisia dracunculus). Pharm Biol 52: 208-212.
- Mojarrab M, Emami SA, Gheibi S, Taleb AM, Afshar FH (2016) Evaluation of antimalarial activity of Artemisia turcomanica and kopetdaghensis by cellfree ß-hematin formation assay. Res J Pharmacognosy 3: 59-65.
- Shafi G, Hasan TN, Syed NA, Al-Hazzani AA, Alshatwi AA, et al. (2012) Artemisia absinthium (AA) a novel potential complementary and alternative medicine for breast cancer. Mol Biol Rep 39: 7373-7379.
- Ashok PK, Upadhyaya K (2013) Preliminary Phytochemical 511 Screening and Physico - Chemical Parameters of Artemisia absinthium and Artemisia annua. J Pharmacogn Phytochem 1: 229-235.
- Rajeshkumar PP, Hosagoudar VB (2012) Mycorrhizal fungi of Artemisia japonica. Bulletin Basic Applied Plant Biol 2: 7-10.
- Nathar VN, Yatoo GM (2014) Micropropagation of an antidiabetic medicinal plant, Artemisia pallens. Turk J Bot 38: 491-498.
- Foglio M A, Dias P C, Antonio M A, Possenti A, Rodrigues R A F, et al. (2002) Antiulcerogenic activity of some sesquiterpene lactones isolated from Artemisia annua. Planta Medica 68(6): 515-518.
- Zafra-Polo MC, Blazquez MA (1991) Anti-inflammatory activity of Sesquiterpene lactones from Artemisia barrelieri in rats. Phytother Res 5: 91-93.
- Romero MR, Serrano MA, Vallejo M, Efferth T, Alvarez M, et al. (2006) Antiviral effect of artemisinin from Artemisia annua against a model member of the Flaviviridae family, the bovine viral diarrhea virus (BVDV). Planta Med 72(13): 1169-1174.
- Koul B, Taak P, Kumar A, Khatri T, Sanyal I (2017) The Artemisia Genus: A Review on Traditional Uses, Phytochemical Constituents, Pharmacological Properties and Germplasm Conservation. J Glycomics Lipidomics 7: 142.
- Ling Y (1994) The genera Artemisia and Seriphidium (Bess.) Poljak in the world. Compositae Newsl pp: 39-45.
- Shultz LM (2006) Artemisia Flora of the North America Editorial Committee (eds.), 1993+.Flora of the North America North of Mexico12+ vols. Oxford University Press, New York 19: 503-534.
- Ling YR (1982) On the system of genus Artemisia and the relationship with its allies. Bulletin of the Botanical Laboratory of the North-Eastern Forestry Institute 2: 1-60.
- Artemisia (genus) Available online at: https://www.newworldencyclopedia.org/entry/Artemisia_(genus)
- Bremer K, Anderberg AA (1994) Asteraceae: cladistics and classification.
- Abid R, Qaiser M (2008) Cypsela morphology and its taxonomic significance of the genus Artemisia (Anthemideae-Asteraceae) from Pakistan. Pak J Bot 40: 1827-1837.
- Garnock-Jones P (1986) Floret specialization, seed production and gender in Artemisia vulgaris (Asteraceae, Anthemideae). Bot J Linn Soc 92: 285-302.
- Zeb S, Ali A, Zaman W, Zeb S, Ali S, et al. (2019) Pharmacology, taxonomy and phytochemistry of the genus Artemisia specifically from Pakistan: A comprehensive review. Pharm Biomed Res 4(4): 1-12.
- Azadbakht M, Ziai H, Shaaban KB (2003) Effect of essential oils of artemisia aucheri Zataria multiflora boiss and myrtus communis l. On trichomonas vaginalis. Iran Pharm Res 8: 35-40.
- Lachenmeier DW (2010) Wormwood (Artemisia absinthium) - A curious plant with both neurotoxic and neuroprotective properties? J Ethnopharmacol 131: 224-227.
- Kershaw L (2000) Edible and medicinal plants of the rockies. Lone Pine Pub.
- Otsuka K, Shoji J, Takido M, Cho S (1992) A Pictorial Encyclopedia of Chinese Medical Herbs (I). Chuokoran-Sha Inc.: Tokyo, Japan.
- Kelly JP, Kaufman DW, Kelley K, Rosenberg L, Anderson TE, et al. (2005) Recent trends in use of herbal and other natural products. Arch Int Med 165: 281-286.
- Zheng GQ (1994) Cytotoxic terpenoids and flavonoids from Artemisia annua. Planta Med. 60(1): 54-57.
- Yang S, Roberts M, O'Neill M, Bucar F, Phillipson J (1995) Flavonoids and chromenes from Artemisia annua. Phytochemistry 38(1): 255-257.
- Han X, Ma X, Zhang T, Zhang Y, Liu Q, et al. (2007) Isolation of high-purity casticin from Artemisia annua by high-speed counter-current chromatography. J Chromatography A 1151(1-2): 180-182.
- Anshul N, Bhakuni R, Gaur R, Singh D (2013) Isomeric Flavonoids of Artemisia annua (Asterales: Asteraceae) as Insect Growth Inhibitors Against Helicoverpa armigera (Lepidoptera: Noctuidae). Florida Entomologist 96(3): 897-903.
- Chougouo R, Nguekeu Y, Dzoyem, J, Awouafack MD, Jonas K, et al. (2016) Anti‑inflammatory and acetylcholinesterase activity of extract, fractions and five compounds isolated from the leaves and twigs of Artemisia annua growing in Cameroon. Springer Plus 5: 1525.
- Cao Y, Zang Y, Huang X, Cheng Z (2019) Chemical constituents from Artemisia rupestris and their neuraminidase inhibitory activity. Nat Product Res pp: 1-8.
- Vasconcelos J, Silva A, Cavaleiro J (1998) Chromones and flavanones from artemisia campestris maritima. Phytochemistry 49(5): 1421-1424.
- Metoui R, Bouajila J, Znati M, Cazaux S, Neffati M, et al. (2017) Bioactive flavones isolated from Tunisian Artemisia campestris Leaves. Cell Mol Biol 63: 86.
- Ji TF, Yang JB, Song WX, Wang AG, Su YL, et al. (2007) Studies on chemical constituents of Artemisia rupestris (II). Zhongguo Zhong Yao Za Zhi 32(12): 1187-1189.
- Ferreira JF, Luthria DL, Sasaki T, Heyerick A (2010) Flavonoids from Artemisia annua as antioxidants and their potential synergism with artemisinin against malaria and cancer. Molecules 15(5): 3135-3170.
- Msaada K, Salem N, Bachrouch O, Bousselmi S, Tammar S, et al. (2015) Chemical composition and antioxidant and antimicrobial activities of wormwood (Artemisia absinthium) essential oils and phenolics. J. Chem 2015: 1-12.
- Hurabielle M, Eberle J, Paris M (1982) Etude des flavonoïdes d’Artemisia campestris sous-espèce glutinosa [Flavonoids of Artemisia campestris, ssp. glutinosa]. Planta Med 46(2): 124-125.
- Wang Q, Pa B, Gong J, Bao W, Hao J, et al. (2019) Phenylpropanoids, flavonoids, and terpenoids from Artemisia ordosica Magn Reson Chem 57(6): 326-330.
- Oana C, Daniel C, Alexander G, Liana T, Elena U, et al (2012) Evaluation of antioxidant and cytoprotective activities of Arnica montana and Artemisia absinthium L. ethanolic extracts. Chem Cent J 6: 97.
- Mamatova A, Korona-Glowniak I, Skalicka-Woźniak K, Józefczyk A, Wojtanowski K, et al (2019). Phytochemical composition of wormwood (Artemisia gmelinii) extracts in respect of their antimicrobial activity. BMC Compl Alternative Med 19(1): 288.
- Sun M, Chen C, Li Y, Gao K (2016) Phytochemical Investigation of the Seeds of Artemisia sphaerocephala. Chem Nat Compd 52(2): 320-321.
- Xiao M, Ye J, Huang Y, Zhang X (2014) Response surface optimization for extraction of flavonoids from artemisia lactiflora wall. ex dc. and evaluation of antioxidant capacities in vitro. Asia J Chemistry 26: 2802-2808.
- Li Y-J, He X, Liu L-N, Lan Y-Y, Wang A-M, et al. (2006) Studies on chemical constituents in herb from Artemisia rupestris. Zhongguo Zhong Yao Za Zhi 31: 1790-1792.
- Esmail A, Mohamed A, El-Sayed M, Hegazy ME, Helaly S, et al. (2015) Chemical constituents and biological activities of Artemisia herba-alba. Rec Nat Prod 4(1): 1-25.
- Han HY, Kim HJ, Jeong SH, Kim J, Jeong SH, et al. (2018) The Flavonoid Jaceosidin from Artemisia princeps Induces Apoptotic Cell Death and Inhibits the Akt Pathway in Oral Cancer Cells. Evid Based Complement Alternat Med 2018: 5765047.
- Moscatelli V, Hnatyszyn O, Acevedo C, Megías J, Alcaraz MJ, et al. (2006) Flavonoids from Artemisia copa with anti-inflammatory activity. Planta Med 72(1): 72-74.
- Lee SJ, Chung H-Y, Maier CGA, Wood AR, Dixon RA, et al. (1998) Estrogenic Flavonoids from Artemisia vulgaris J Agr Food Chem 46(8): 3325-3329.
- Cha JD, Jeong MR, Choi HJ, Jeong S-I, Moon SE, et al. (2005) Chemical composition and antimicrobial activity of the essential oil of Artemisia lavandulaefolia. Planta Med 71(6): 575-577.
- Wang XQ, Zhou CJ, Zhang N, Wu G, Li MH (2011) Studies on the chemical constituents of Artemisia lavandulaefolia. Zhong Yao Cai 34(2): 234-236.
- Su Z, Wu HK, He F, Slukhan U, Aisa HA (2010) New guaipyridine sesquiterpene alkaloids from Artemisia rupestris Helvetica Chimica Acta 93(1): 33-38.
- Su Z, Wu H, Yang Y, Aisa HA, Slukhan U, et al. (2008) Preparative isolation of guaipyridine sesquiterpene alkaloid from Artemisia rupestris flowers using high‐speed counter‐current chromatography. J Sep Sci 31(12): 2161-2166.
- He F, Nugroho AE, Wong CP, Hirasawa Y, Shirota O, et al. (2012) Rupestines F-M, New guaipyridine sesquiterpene alkaloids from Artemisia rupestris. Chem Pharm Bull 60(2): 213-218.
- Sham'yanov ID, Tashkhodzhaev B, Mukhamatkhanova RF, Sultankhodzhaev MN, Levkovich MG, et al. (2012) Sesquiterpene lactones and new diterpenoid alkaloids from Artemisia korshinskyi. Chem Nat Compd 48(4): 616-6121.
- Fontaine P, Wong V, Williams TJ, Garcia C, Adams JD Jr (2013) Chemical composition and antinociceptive activity of California sagebrush (Artemisia californica). J Pharmacogn Phytotherapy 5(1): 1-7.
- Wang H, Ye HC, Liu BY, Li ZQ, Li GF (2003) Advances in molecular regulation of artemisinin biosynthesis. Chinese J Biotechnol 19(6): 646-650.
- Ma HY, Sun Y, Zhou YZ, Hong M, Pei YH (2008) Two new constituents from Artemisia capillaris Molecules 3(2): 267-271.
- Shukla A, Abad F, AH, Shukla YN (1997) A new adenine derivative from Artemisia annua. J Indian Chem Soc 74(1): 59.
- Lu H, Zou WX, Meng JC, Hu J, Tan RX (2000) New bioactive metabolites produced by Colletotrichum sp., an endophytic fungus in Artemisia annua. Plant Sci 151(1): 67-73.
- Liu SJ, Liao ZX, Liu C, Ji LJ, Sun HF (2014) Two new sesquiterpenes from Artemisia sieversiana. Fitoterapia 97: 43-49.
- Zou Y, Shi J, Shi H (1999) Analysis of volatile components from Artemisia annua Fenxi Ceshi Xuebao 18: 55-57.
- Choi JY, Cho IH, Kim YS, Lee HJ (2014) Aroma‐active compounds of Korean mugwort (Artemisia princeps orientalis). J Korean Soc Appl Biol 57(3): 323-329.
- Giang PM, Nhan TT, Chinh TT, Son PT, Matsunami K (2015) Phytochemical Constituents of Artemisia dubia longeracemosa Forma tonkinensis. Chem Nat Compd 51(2): 378-380.
- Bourgou S, Rebey IB, Mkadmini K, Isoda H, Ksouri R, et al. (2017) LC‐ESI‐TOF‐MS and GC‐MS profiling of Artemisia herba-alba and evaluation of its bioactive properties. Food Res Int 99: 702-712.
- Nguyen HT, Nguyen HT, Islam MZ, Obi T, Pothinuch P, et al. (2016) Pharmacological characteristics of Artemisia vulgaris in isolated porcine basilar artery. J Ethnopharmacol 182: 16-26.
- Megdiche‐Ksouri W, Trabelsi N, Mkadmini K, Bourgou S, Noumi A, et al. (2015) Artemisia campestris phenolic compounds have antioxidant and antimicrobial activity. Indust Crop Product 63: 104-113.
- Lee S-H, Ding Y, Xi TY, Kim YH, Jang H-D (2013) Scopoletin and Scopolin Isolated from Artemisia iwayomogi Suppress Differentiation of Osteoclastic Macrophage RAW 264.7 Cells by Scavenging Reactive Oxygen Species. J Nat Prod 76(4): 615-620.
- Dib I, Angenot L, Mihamou A, Ziyyat A, Tits M (2016) Artemisia campestris: Ethnomedicinal, phytochemical and pharmacological review. J Herbal Med 7: 1-10.
- Bao, W, Wang Q, Hao J (2019) Structural Elucidation of a Coumarin with New Skeleton from Artemisia ordosica. Rec of Natural Products 13: 413-417.
- Cui FX, Zhang C, Jiang Y, Tu PF (2013) Chemical constituents from ethyl acetate extract of Artemisia rupestris. Zhongguo Zhong Yao Za Zhi 38(11): 1757-1759.
- Tang S, Ma Y-B, Geng C-A, Shen C, Li TZ, et al. (2020) Artemyrianins A-G from Artemisia myriantha and Their Cytotoxicity Against HepG2 Cells. Nat Prod Bioprospect 10(4): 251-260.
- Cho JY, Jeong SJ, Lee HL, Park KH, Hwang DY, et al. (2016) Sesquiterpene lactones and scopoletins from Artemisia scoparia & Kit and their angiotensin I-converting enzyme inhibitory activities. Food Sci Biotechnol 25: 1701-1708.
- Greger H (1981) Sesamin-type lignans as chemical markers within Artemisia. Biochem Syst Ecol 9(2-3): 165-169.
- Ortet R, Prado S, Regalado E, Valeriote F, Media J, et al. (2011) Furfuran lignans and a flavone from Artemisia gorgonum Webb and their in vitro activity against Plasmodium falciparum. J Ethnopharmacol 138(2): 637-640.
- Tan R, Tang H, Hu J, Shuai B (1998) Lignans and Sesquiterpene Lactones from Artemisia Sieversiana and Inula Racemosa. Phytochemistry 49(1): 157-161.
- Liu S, Liao Z, Liu C, Ji L, Sun H (2014) Two new sesquiterpenes from Artemisia sieversiana. Fitoterapia 97: 43-49.
- Marco AJ, Sanz-Cervera JF, Lliso GV, Xirau JV (1997) Sesquiterpene lactones and lignans from Artemisia arborescens. Phytochemistry 44(6): 1133-1137.
- Ma C, Nakamura N, Min B, Hattori M (2001) Triterpenes and Lignans from Artemisia caruifolia and Their Cytotoxic Effects on Meth-A and LLC Tumor Cell Lines. Chem Pharm Bull 49(2): 183-187.
- Tulake A, Tu P (2012) Nine lignans from Artemisia absinthium J Chinese Pharm Sci 21(4): 360-364.
- He Z, Yan J, Song Z, Ye F, Liao X, et al. (2009) Chemical Constituents from the Aerial Parts of Artemisia J Nat Prod 72(6): 1198-1201.
- Wei ZX, Pan JP, Li Y (1992) Artemisinin G: A Sesquiterpene from Artemisia annua. Planta Med 58(3): 300.
- Hajdú Z, Hohmann J, Forgo P, Máthé I, Molnár J, et al. (2014) Antiproliferative activity of Artemisia asiatica extract and its constituents on human tumor cell lines. Planta Med 80: 1692-1697.
- Wang S, Sun J, Zeng K, Chen X, Zhou W, et al. (2014) Sesquiterpenes from Artemisia argyi: absolute configurations and biological activities. Europ J Org Chem 2014: 973-983.
- Hanh TTH, Hang LTT, Huong PTT, Trung NQ, Cuong TV, et al. (2018) Two new guaiane sesquiterpene lactones from the aerial parts of Artemisia vulgaris. J Asian Nat Prod Res 20(8): 752-756.
- Zan K, Chai XY, Chen XQ, Wu Q, Fu Q, et al. 92012) Artanomadimers A-F six new dimeric guaianolides from Artemisia anomala. Tetrahedron 68: 5060-5065.
- Wen J, Shi H, Xu Z, Chang H, Jia C, et al. (2009) Dimeric guaianolides and sesquiterpenoids from Artemisia anomala. J Nat Prod 73: 67-70.
- Zan K, Chen XQ, Chai XY, Wu Q, Fu Q, et al. (2012) Two new cytotoxic eudesmane sesquiterpenoids from Artemisia anomala. Phytochem Lett 5: 313-315.
- Thangjam N, Taijong J, Kumar A (2020) Phytochemical and pharmacological activities of methanol extract of Artemisia vulgaris leaves. Clin Phytosci 6: 72.
- Mitra M, Ebrahimzadeh MA, Ansaroudi F, Nabavi SF (2009) Antidepressant and antioxidant activities of Artemisia absinthium at flowering stage. Afr J Biotechnol 8(24): 7170-7175.
- Lee JH (2014) Evaluation for Antioxidant Activity of Artemisia Plants. Res J Med Plant 8(6): 258-268.
- Choi E, Park H, Lee J, Kim G (2013) Anticancer, anti-obesity, and anti-inflammatory activity of Artemisia species in vitro. J Tradit Chin Med 33(1): 92-97.
- Yen M, Huang C, Lee M, Cheng Y, Hsieh C, et al. (2018) Artemisia capillaris inhibited enterovirus 71-induced cell injury by preventing viral internalization. Kaohsiung J Med Sci 34(3): 150-159.
- Kiso Y, Ogasawara S, Hirota K, Watanabe N, Oshima Y, et al. (1984) Antihepatotoxic principles of Artemisia capillaris Planta Med 50: 81-85.
- Hu YQ, Tan R.X, Chu M.Y, Zhou J (2000) Apoptosis in human hepatoma cell line SMMC-7721 induced by water-soluble macromolecular components of Artemisia capillaries Japan J Cancer Res 91(1): 113-117.
- Singh NP, Lai HC (2007) Artemisinin induces apoptosis in human cancer cells. Anticancer Res 24: 2277-2280.
- Emami SA, Mashhadian NV, Vosough R, Oghazian MB (2009) The anticancer activity of five species of Artemisia on Hep2 and HepG2 cell lines. Pharmacol Online 3: 327-339.
- Zhong Y, Cui S (1992) Effective chemical constituents of Artemisia argyi Et Vant for inhibition of platelet aggregation. China J Chinese Mater Med 17(6): 353-354.
- Lv JL, Li ZZ, Zhang LB (2018) Two new flavonoids from Artemisia argyi with their anticoagulation activities. Nat Prod Res 32(6): 632-639.
- Ge YB, Wang ZG, Xiong Y, Huang XJ, Mei ZN, et al. (2016) Anti-inflammatory and blood stasis activities of essential oil extracted from Artemisia argyi leaf in animals. J Nat Med 70(3): 531-538.
- Afsar SK, Kumar KR, Gopal JV, Raveesha P (2013) Assessment of anti-inflammatory activity of Artemisia vulgaris leaves by cotton pellet granuloma method in Wistar albino rats. J Pharm Res 7(6): 463-467.
- Irshad S, Mirza AM (2011) Antimalarial Activity of Three Pakistani Medicinal Plants. Pakistan J Pharm Sci 24(4): 589-591.
- Bamunuarachchi G, Ratnasooriya W, Premakumara S, Udagama P (2013) Study of Anti-malarial Activity of Artemisia vulgaris Leaf Extract, using the Plasmodium berghei murine model. J Vector Borne Dis 50: 278-284.
- Panda S, Rout J, Pati P, Ranjit M, Sahoo S (2017) Antimalarial activity of Artemisia nilagirica against Plasmodium falciparum. J Parasitic Dis 42(1): 22-27.
- Erel SB, Reznicek G, Şenol SG, Yavaşoğulu NUK, Konyalioğlu S, et al. (2012) Antimicrobial and antioxidant properties of Artemisia species from western Anatolia. Turkish J Biol 36(2012): 75-84.
- Mojarrab M, Naderi R, Afsha FH (2015) Screening of different extracts from Artemisia species for their potential antimalarial activity. Iran J Pharm Res 14(2): 603-608.
- Kassa M, Mshana R, Regassa A, Assefa G (1998) In vitro test of five Ethiopian medicinal plants for antimalarial activity against plasmodium falciparum. SINET Ethiop J Sci 21(1): 81-89.
- Maqsood M, Qureshi R, Ikram M, Ali S, Rafi M, et al. (2015) Preliminary screening of methanolic plant extracts against human rhabdomyo sarcoma cell line from salt range Pakistan. Pakistan J Botany 47(1): 353-357.
- Afshar F H, Delazar A, Janneh O, Nazemiyeh H, Pasdaran A, et al. (2011) Evaluation of antimalarial, free-radical scavenging and insecticidal activities of Artemisia scoparia and spicigera, Asteraceae. Braz J Pharmacog 21(6): 986-990.
- Diawara HZ, Ganfon H, Gbaguidi F, Yemoa A, Bero J, et al. (2015) The antimalarial action of aqueous and hydro alcoholic extracts of Artemisia annua Cultivated in Benin: In vitro and in vivo studies. J Chem Pharm Res 7(8): 817-823.
- Suresh J, Vasavi RA, Rajan D, Ihsanullah M, Khan MN (2010) Antimicrobial activity of Artemisia abrotanum and Artemisia pallens. Int J Pharmacog Phytochem Res 3(2): 18-20.
- Kordali S, Kotan R, Mavi A, Cakir A, Ala A (2005) Yildirim. Determination of the chemical composition and antioxidant activity of the essential oil of Artemisia dracunculus and of the antifungal and antibacterial activities of Turkish Artemisia absinthium, dracunculus, Artemisia santonicum, and Artemisia spicigera essential oils. J Agric Food Chemy 53(24): 9452-9458.
- Devmurari VP, Jivani NP (2011) Phytochemical screening and antibacterial activity of ethanolic extract of Artemisia Nilagirica. Ann Biol Res 1(1): 10-14.
- El Abed N, Guesmi F, Mejri M, Marzouki MN, Ahmed SBH (2014) Phytochemical screening and assessment of antioxidant, antibacterial and cytotoxicity activities of five Tunisian medicinal Plants. Int J Pharm Res Biol Sci 3(4): 770-789.
- Naili MB, Alghazeer RO, Saleh NA, Al-Najjar AY (2010) Evaluation of antibacterial and antioxidant activities of Artemisia campestris (Astraceae) and Ziziphus lotus (Rhamnacea). Arab J Chem 3(2): 79-84.
- Nageeb A, Al-Tawashi A, Emwas AHM, Al-Talla ZAH, Al-Rifai N (2013) Comparison of Artemisia annua bioactivities between traditional medicine and chemical extracts. Curr Bioactive Compd 9(4): 324-332.
- Seo JM, Kang HM, Son KH, Kim JH, Lee CW, et al. (2003) Antitumor activity of flavones isolated from Artemisia argyi. Planta Med 69(3): 218-222.
- Chemesova LL, Belenovskaya LM, Stukov AN (1987) Anti-tumour activity of flavonoids from some Artemisia Rastitel'nye Res 23: 100-103.
- Zeng YT, Jiang JM, Lao HY, Guo JW, Lun NY, et al. (2015) Antitumor and apoptotic activities of the chemical constituents from the ethyl acetate extract of Artemisia indica. Mol Med Rep 11(3): 2234-2240.
- Cao R, Hu H, Li Y, Wang X, Xu M, et al. (2020) Anti-SARS-CoV-2 Potential of Artemisinins In Vitro. ACS Infect Dis 6(9): 2524-2531.
- Karamoddini MK, Emami SA, Ghannad MS, Sani EA, Sahebkar A (2017) Antiviral activities of aerial subsets of Artemisia species against Herpes Simplex virus type 1 (HSV1) in vitro. Asian Biomed 5(1): 63-68.
- Nofal SM, Mahmoud SS, Ramadan A, Soliman GA, Fawzy R (2009) Anti-diabetic effect of Artemisia Judaica Res J Med Sci 4(1): 42-48.
- Twaij HAA, Al-Badr AA (1988) Hypoglycemic activity of Artemisia herba-alba. J Ethnopharmacol 24(2-3): 123-126.
- Al-Shamaony LA, Al-Khazraji SM, Twaij HAA (1994) Hypoglycaemic effect of Artemisia herba alba. II. Effect of a valuable extract on some blood parameters in diabetic animals. J Ethnopharmacol 43(3): 167-171.
- Ghazanfar K, Ganai BA, Akbar S, Mubashir K, Dar SA, et al. (2014) Antidiabetic Activity of Artemisia amygdalina Decne in Streptozotocin Induced Diabetic Rats. BioMed Res Int 2014: 1-10.
- Jayasimha GB, Chikka SBK (2016) Antidiabetic Activity of Artemisia Absinthium Versus Metformin in Stz Induced Diabetic Rats. Int J Adv Res Eng Appl Sci 5(11): 1-12.
- Sebai H, Jabri M, Souli A, Hosni K, Selmi S, et al. (2014) Protective effect of Artemisia campestris extract against aspirin-induced gastric lesions and oxidative stress in rat. RSC Adv 4(91): 49831-49841.
















