2150
Views & Citations1150
Likes & Shares
Tuberculosis, a major cause of illness and death worldwide, ranks among the top 10 diseases leading to mortality. In fact, tuberculosis is among the top three fatal infectious diseases worldwide, with HIV/AIDS being the leading cause of death for 3 million people annually, followed by TB which kills 2 million individuals, and malaria, which claims the lives of 1 million people [2]. With the COVID-19 pandemic, the number of cases of TB is expected to increase [3].
Effective control of Mycobacterium tuberculosis infection is dependent on various factors, including the presence of CD4+ T cells and cytokines such as IL-12, IFN-γ, and TNF [4].
Despite advancements in diagnosing and treating tuberculosis, this disease continues to claim the lives of millions of individuals. The Global Tuberculosis Report of 2018 reveals that around 10 million new cases of tuberculosis occur every year, which is equivalent to 133 cases per 100,000 people [5]. Drug-resistant tuberculosis, particularly multi-drug-resistant TB (MDR-TB), has been identified as a major threat to global public health in recent years. The initial report was based on data from around 50,000 patients in 35 countries across five continents, revealing resistance to drugs such as isoniazid and streptomycin. In a subsequent report, published in April 2000, surveillance was expanded to include 72 countries, with data showing trends in TB drug resistance [6].
TYPES OF TB
Primary Pulmonary TB
It is seen in patients not previously exposed to Mycobacterium tuberculosis. About two-thirds of individuals with this form of TB do not exhibit any symptoms [7].
Endobronchial TB
Endobronchial tuberculosis is caused by the spread of TB from a pulmonary source or through the inhalation of infected sputum, which directly affects the bronchial tree [8].
Extrapulmonary TB
Among individuals with a normal immune system, extrapulmonary tuberculosis represents approximately 15% of all TB cases [9].
Pleural tuberculosis
Pleural tuberculosis is the second most common form of extrapulmonary TB, accounting for approximately 4% of all TB cases [10].
Central nervous Tuberculosis
Central nervous Tuberculosis can severely affect the central nervous system, with central nervous system tuberculosis occurring in about 1% of all cases of TB [11].
Tuberculous peritonitis
Tuberculous peritonitis is the most prevalent form of TB in the gastrointestinal tract [12].
Miliary tuberculosis
The dissemination of TB through the lymphatic and bloodstream is known as miliary tuberculosis [13].
Indian scenario: Approximately 27% of the global burden of tuberculosis cases are reported in India. To address this issue, India has implemented the World Health Organization-endorsed Directly Observed Treatment, Short-Course (DOTS) as part of its Revised National Tuberculosis Control Program (RNTCP) since 1997 [14]. Despite the efforts made by the Revised National Tuberculosis Control Program, tuberculosis continues to be the primary infectious cause of death in India, claiming the lives of nearly 500,000 individuals annually. India has a high prevalence of tuberculosis in the world, with about 2 million new instances every year [15]. India has been dealing with drug-resistant tuberculosis for a long time, dating back to the introduction of anti-tuberculosis drugs for the treatment of the disease. However, due to the limited availability of culture and susceptibility testing facilities, there is a lack of comprehensive reports on the subject [16]. Between 2000 and 2003, a nationwide study conducted in India estimated the average annual risk of tuberculosis Infection (ARTI) to be 1.5%. Furthermore, an upward trend has been observed in the prevalence of HIV among tuberculosis cases [17].
Based on many study results, the prevalence rate of latent tuberculosis infection can be estimated to be 3.5 per 1000 individuals. In comparison, the prevalence of active non-infectious tuberculosis in individuals aged 15 years and above has consistently been reported to be 16 per 1000 [18]. A survey conducted in southern India, covering 71,874 adults in rural Bangalore, found an overall prevalence of 196 cases per 100,000 population who were bacteriologically positive [19]. The DOTS strategy has been enforced in the whole district since 2002.
The Revised National Tuberculosis Control Programme (RNTCP) presently known as the National Tuberculosis Elimination Programme (NTEP), is the Public Health initiative of the Government of India that organizes its anti-Tuberculosis efforts [20].
Its Vision is TB-Free India with zero deaths, disease, and poverty due to tuberculosis, Goal: To achieve a rapid decline in the burden of TB, morbidity, and mortality while working towards elimination of TB in India by 2025.
The National Strategic Plan ((NSP) for TB Elimination 2017-25 [21] is a bold strategic framework to drive the acceleration of progress toward TB Elimination, and achieving the Sustainable Development Goal (SDG) and End TB targets for India.
It expects to guide the activities of all stakeholders including the national and state governments, development partners, civil society organizations, international agencies, research institutions, the private sector, and many others whose work is relevant to TB elimination in India.
It adopts strategies under four groups: DETECT, TREAT, PREVENT, BUILD.
Standard treatment regimen
For initial empiric treatment of TB, start patients on a 4-drug regimen [22]: isoniazid, rifampin, pyrazinamide, and either ethambutol or streptomycin. Once the TB isolate is known to be fully susceptible, ethambutol (or streptomycin, if it is used as a fourth drug) can be discontinued.
DOTS is currently the WHO-recommended strategy for TB control. Directly Observed Therapy (DOT) is the practice of observing a patient swallow his or her tuberculosis (TB) medications. National guidelines recommend DOT as part of the standard of care for TB treatment, and DOT is used by TB programs throughout the world including India.
DOTS involved treatment with a four-drug regimen. These were isoniazid (INH), Rifampicin (Rif), Prazinamide (PZA) and Ethambutol (EMB) for 6-9 months.
DOTS must be used throughout the entire course of therapy for best cure rates. All patients with DS-TB without documented resistance to isoniazid and rifampicin may be treated using the 6-month rifampicin-containing regimen 2HRZ(E)/4HR, which comprises isoniazid, rifampicin, pyrazinamide and ethambutol, for 2 months followed by isoniazid and rifampicin for 4 months.
Given the global burden of tuberculosis, shortened treatment regimens are needed for tuberculosis control. The long duration of treatment of drug-susceptible tuberculosis (DS-TB) is associated with nonadherence and loss to follow-up, and the treatment success rate of multidrug-resistant tuberculosis (MDR-TB) is low (approximately 50%) with longer regimens.
There are two different 4-month regimens available for treatment. The first regimen consists of rifapentine, isoniazid, pyrazinamide, and ethambutol and is used for the treatment of adults with tuberculosis.
The second 4-month rifapentine-moxifloxacin regimen has an intensive phase of 8 weeks of daily treatment with rifapentine, isoniazid, pyrazinamide, and moxifloxacin followed by a continuation phase of 9 weeks of daily treatment with rifapentine, isoniazid, and moxifloxacin (a total of 17 weeks for treatment) [23].
A trial conducted in 13 countries comparing 4-month rifapentine based regimens with a standard 6-month regimen in people with drug-susceptible TB was reviewed by a guideline development group (GDG) convened by the WHO in April 2021. The GDG found that a 4-month regimen consisting of rifapentine, isoniazid, pyrazinamide, and moxifloxacin met the noninferiority criteria specified in the trial protocol. Based on the available evidence, this regimen is now being considered as a potential alternative to the current standard 6-month regimen [24].
OBJECTIVE
The objective of this study was to assess the effectiveness of Directly Observed Treatment Short course (DOTS) in treatment of Tuberculosis (TB) patients in all Government health care facilities of Bangalore (rural and urban) district.
MATERIALS AND METHODS
Study Design: Retrospective cross-sectional study
Study Site: Bangalore Government Hospitals (BGH) both rural and urban
Study period: February 2022 to March 2023
Government health facilities offer services for the diagnosis and treatment of TB. The diagnostic process includes clinical assessment, CBNAAT (Cartridge-Based Nucleic Acid Amplification Test which is used to detect Tuberculosis (TB) and drug-resistant TB by amplifying and detecting specific DNA sequences of the TB bacteria), CHEST X-RAY, culture, cytopathology, F-line LPA (Line Probe Assay for detection of First Line Drugs Resistance in Tuberculosis by examining specific genetic mutations associated with resistance to first-line TB drugs), gene sequencing and histopathology. Microscopy ZN (Ziehl-Neelsen Staining for Microscopy) which is a laboratory technique used to stain and visualize tuberculosis bacteria (acid-fast bacilli) under a microscope is also used. It helps diagnose TB by identifying the characteristic staining pattern of these bacteria and fluorescence microscopy. Fluorescent microscopy is a technique that uses fluorescent dyes or markers to visualize specific structures or substances within cells or tissues.
TB patients are administered a uniform drug regimen throughout their treatment course, with the duration of treatment varying depending on the type of TB. Despite variations in the duration of treatment, the medication prescribed to all TB patients remains constant.
If it is 6-9 months regimen, DOTS therapy consists of Isoniazid (INH), Rifampicin (Rif), Prazinamide (PZA) and Ethambutol (EMB). If it is a 4month regimen, Rifapentine, Isoniazid, Pyrazinamide, and Moxifloxacin are used.
DATA COLLECTION
Data was collected by research students/staff and medical laboratory workers using a checklist prepared for this purpose based on the contents found in the TB registration book. The study encompassed the collection of patient information such as age, gender, residential address, emergency contact details, type of TB, patient status, HIV diagnosis, co morbidity and treatment. The study involved an extensive analysis of 12,618 TB patient records who received treatment between February 2022 and March 2023.
DATA ANALYSIS
The collected data was subjected to statistical analysis to obtain percentage distributions, and Chi-square test was performed to analyze our results.
RESULTS
Among the 12,618 patients, 7,308 (57.91%) were male, 5,300 (42.03%) were female patients and 10 patients (0.079%) were transgender. The study findings also revealed that 46%, of the patients with TB were aged below 40 years, and the majority (91.5%) were new cases as shown in Table 1.

The major co-morbid conditions considered in the patients were HIV and Diabetes.
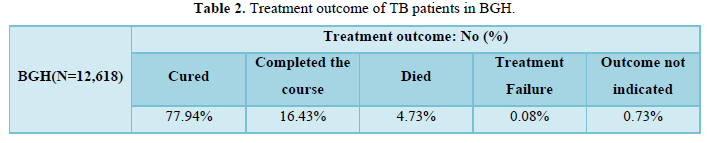
84.65% of the TB patients were not reactive to HIV, while 27.90% were HIV reactive. The treatment success rate for HIV-negative patients was 30.74%, compared to 0.903% for HIV-positive patients. However, the association between HIV status and treatment success rate was not statistically significant (P = 0.342). The study also showed that a higher number of HIV-negative TB patients received treatment at the hospital, and this association was statistically significant (P< 0.001). 71.0% of the patients were diabetic and 14.1% were non-diabetic. The highest number of cured TB patients was observed at BGH (Table 2). Furthermore, it was observed that the treatment success rate for TB patients at all government hospitals in Bangalore was 77.9%, and this association was statistically significant (P=0.0464). Age and gender were not significantly associated with treatment outcomes (P=0.0649).
After analyzing the data of 12,618 patients, we found that 96.8% were responsive to rifampicin and 3.4% showed rifampicin resistance. Only one patient, representing a minuscule 0.008% of the cohort, demonstrated moxifloxacin resistance.
DISCUSSION
This study provides insight into the prevalence of tuberculosis and its treatment outcomes among patients in Bangalore.
The results indicate that males are more affected by tuberculosis than females, and most patients are new cases. Diabetes had high prevalence among TB patients in BGH and there is a need for effective interventions to manage this comorbidity. A considerable number of patients were HIV reactive. The study reveals the low prevalence of rifampicin and moxifloxacin resistance among TB patients in Bangalore.
However, the emergence of drug resistance is a growing concern globally, and continued monitoring of drug resistance is necessary to prevent the same. New drugs with high efficacy against Mycobacterium tuberculosis could improve treatment outcomes for cases with resistance to isoniazid and rifampicin and reduce the duration of existing treatment regimens [25].
As the vision of National Tuberculosis Elimination Programme (NTEP) for India is Total freedom from TB by 2023, effective intervention strategies must be planned to get 100% cure rate.
CONCLUSION
Overall, it can be concluded that DOTS therapy is effective in curing 77.94 % of TB patients in Bangalore. Diabetes was prevalent in majority of the patients as co-morbidity which has to be looked into. The resistance to rifampicin was low and to moxifloxacin, was negligible.
There is a need for continuous monitoring and effective interventions to achieve 100 % cure rates and zero % resistance as per the vision of NSP.
The National Strategic Plan (NSP) for TB elimination 2017-25 is a bold strategic framework to drive the acceleration of progress toward TB Elimination, and achieving the Sustainable Development Goal (SDG) and End TB targets for India.
-
Terracciano E, Amadori F, Zaratti L, Franco E (2020) Tuberculosis: An ever-present disease but difficult to prevent. Ig Sanita Pubbl 76(1): 59-66.
-
O'Garra A, Redford PS, McNab FW, Bloom CI, Wilkinson RJ, et al. (2013) The immune response in tuberculosis. Annu Rev Immunol 31: 475-527.
-
Imran M, Khan SA, Asdaq SMB, Almehmadi M, Abdulaziz O, et al. (2022) An insight into the discovery, clinical studies, compositions, and patents of macozinone: A drug targeting the DprE1 enzyme of Mycobacterium tuberculosis. J Infect Public Health 15(10): 1097-1107.
-
Sia JK, Rengarajan J (2019) Immunology of Mycobacterium tuberculosis Microbiol Spectr 7(4): 10.
-
O'Garra A, Redford PS, McNab FW, Bloom CI, Wilkinson RJ, et al. (2013) The immune response in tuberculosis. Annu Rev Immunol 31: 475-527.
-
Sathiyamoorthy R, Kalaivani M, Aggarwal P, Gupta SK (2020) Prevalence of pulmonary tuberculosis in India: A systematic review and meta-analysis. Lung India 37(1): 45-52.
-
Nachega JB, Chaisson RE (2003) Tuberculosis drug resistance: A global threat. Clin Infect Dis 36(1): S24-S30.
-
Sia IG, Wieland ML (2011) Current concepts in the management of tuberculosis. Mayo Clin Proc 86(4): 348-361.
-
Rikimaru T (2004) Endobronchial tuberculosis. Expert Rev Anti Infect Ther 2(2): 245-251.
-
Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR (2009) Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis 49(9): 1350-1357.
-
Phypers M, Harris T, Power C (2006) CNS tuberculosis: A longitudinal analysis of epidemiological and clinical features. Int J Tuberc Lung Dis 10(1): 99-103.
-
Baumann MH, Nolan R, Petrini M, Lee YC, Light RW, et al. (2007) Pleural tuberculosis in the United States: Incidence and drug resistance. Chest 131(4): 1125-1132.
-
Sharma SK, Mohan A, Sharma A, Mitra DK (2005) Miliary tuberculosis: New insights into an old disease. Lancet Infect Dis 5(7): 415-430.
-
Hussain SF, Irfan M, Abbasi M, Anwer SS, Davidson S, et al. (2004) Clinical characteristics of 110 miliary tuberculosis patients from a low HIV prevalence country. Int J Tuberc Lung Dis 8(4): 493-499.
-
Khatri GR, Frieden TR. Cont (2002) Controlling tuberculosis in India. N Engl J Med 347(18): 1420-1425.
-
Seung KJ, Keshavjee S, Rich ML (2015) Multidrug-Resistant Tuberculosis and Extensively Drug-Resistant Tuberculosis. Cold Spring Harb Perspect Med 5(9): a017863.
-
Thomas BE, Subbaraman R, Sellappan S, Suresh C, Lavanya J, et al. (2018) Pretreatment loss to follow-up of tuberculosis patients in Chennai, India: A cohort study with implications for health systems strengthening, BMC Infect Dis 18(1): 142.
-
Al-Hrazi RMA, Al-Shamahy HA, Jaadan BM (2019) Determination of rifampicin mono-resistance Mycobacterium tuberculosis in the National tuberculosis control programme in Sana’a city-Yemen: A significant phenomenon in war region with high prevalence tuberculosis. Universal J Pharm Res 4(3): 12-17.
-
Aggarwal AN, Gupta D, Agarwal R, Sethi S, Thakur JS, et al. (2015) Prevalence of pulmonary tuberculosis among adults in a north Indian district. PLoS One 10(2): e0117363.
-
National TB Elimination Program (India). Available online at: https://en.wikipedia.org/wiki/National_TB_Elimination_Program_(India)
-
Revised National Tuberculosis Control Programme, NATIONAL STRATEGIC PLAN FOR TUBERCULOSIS ELIMINATION 2017–2025 March 2017 Central TB Division, Directorate General of Health Services, Ministry of Health with Family Welfare, Nirman Bhavan, New Delhi; pp: 110 108. Available online at: https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf
-
Herchline TE, Amorosa JK (2023) Tuberculosis (TB) Treatment & Management. Drugs & Dis Available online at: https://emedicine.medscape.com/article/230802-treatment
-
Dorman SE, Nahid P, Ekaterina V, Kurbatova, Phillips PPJ (2021) Four-Month Rifapentine Regimens with or without Moxifloxacin for Tuberculosis. N Engl J Med 384(18): 1705-1718.
-
Genet C, Melese A, Worede A (2019) Effectiveness of directly observed treatment short course (DOTS) on treatment of tuberculosis patients in public health facilities of Debre Tabor Town, Ethiopia: Retrospective study. BMC Research Notes 12(1): 1-5.
-
Seung KJ, Keshavjee S, Rich ML (2015) Multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis. Cold Spring Harb Perspect Med 5(9): a017863.

