2529
Views & Citations1529
Likes & Shares
Keywords: Lymphatic filariasis, MDA, Andhra Pradesh, Need of vaccination
This disfiguring disease is due to the bite of blood-sucking mosquitoes (Aedes aegypti, Culex quinquifasciatus and Mansonia africana) in the tropical region of the world. There are three nematode worms belonging to the family Filariodidea. They are Wuchereria bancrofti, Brugia malayi and Brugia timori [3,4]. These nematode parasites once mature reside in the lymph vessels and block lymph flow rendering a situation called lymphedema. World Health Organization through a resolution (WHA50.29) advocated to the Member States to eliminate lymphatic filariasis as a public health issue and consequently launched a Global Programme to Eliminate Lymphatic Filariasis (GOELF) in the year 2000 which set the NTD (Neglected Tropical Diseases) roadmap extended up to the year 2030 [5]. MDA (albendazole (400 mg), ivermectin (200 mcg/kg) and diethylcarbamazine (400 mg) is implemented in all endemic countries among both the risk individuals and also lymphedema patients living in the endemic zone with the help of health workers annually [6,7]. The progress of NTD roadmap as observed from South India and particularly in the state of Andhra Pradesh (India) is evaluated in the present article through the regression analysis so as to forecast the better living.
METHODS
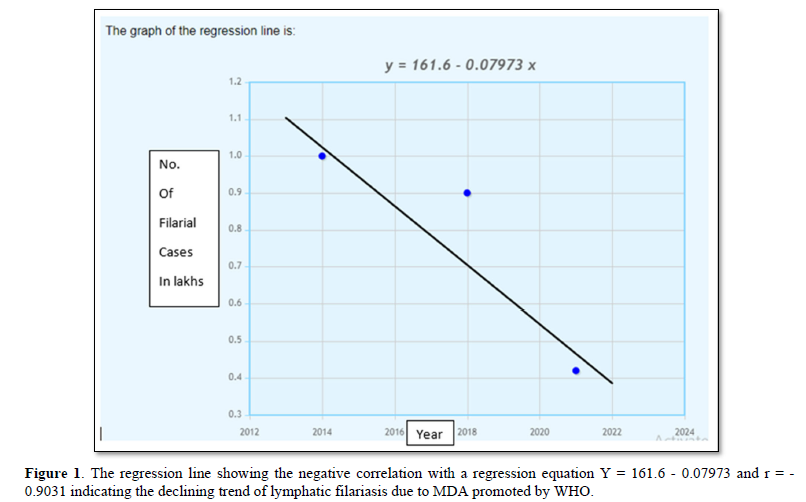
The data on the prevalence of lymphatic filariasis in patients from four states of South India were retrieved from indiastat.com and National Health Mission (India) [8]. The obtained data is shown in Table 1. The regression analysis was performed using online tool viz., https://www.mathportal.org/calculators/statistics-calculator/correlation-and-regression-calculator.php [9]. The resulted regression line and equation are shown in the Figure 1.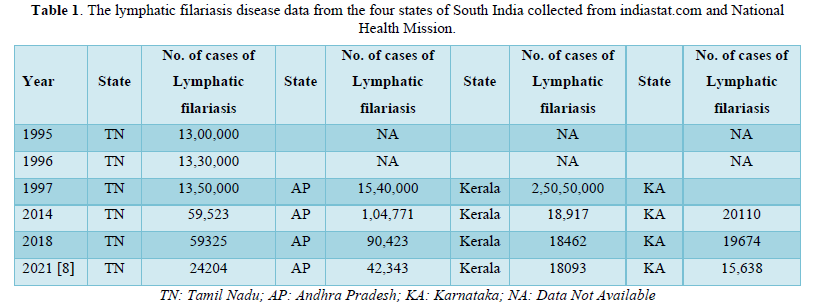
RESULTS AND DISCUSSION
The tropical region of the world, particularly the southern hemisphere, is rich in flora and fauna due to its climatic conditions. Further, the insect-vectors are flourishing well in this well-populated zone of plants and animals. Hence, there is an enormous scope for zoonotic infections to transmit and spread across the mammalian species and humans. One such is the elephantiasis, a serious disfiguring disease due to the defined mosquitoes indicated in the introduction section. The mosquitoes are the intermediate host for filarial worms. While sucking the blood from the infected subjects, the microfilaria goes into the gut of the insect and settles in the salivary glands up to L3 stage (third instar). This stage of microfilariae is the infective stage which is carried to the naïve uninfected man once bitten by the microfilariae carrying mosquito. These transmitted microfilariae are of the size of RBC and keeps staying in the blood stream for a long period (yet to be defined in the literature) till they become adults, then they move to the lymphatic circulation where they reside and produce numerous eggs to continue its life-cycle. During this time the infected individuals face illness due to lymphedema. The MDA (drugs shown in the introduction section) recommended by WHO is being given in all the filarial endemic zones since the year 2000.
The resultant impact of MDA in all the four states of South India is shown in Table 1. Most importantly, as per the guidelines of WHO [1,6,9], the contribution of health workers in the dramatic reduction in the number of lymphatic filariasis patients is noteworthy. Among the four states reported, Andhra Pradesh is showing more number of affected cases. By 2021, as per the data from National Health Mission (NVBDCP) [8], the number of reported affected cases is found high in the state of Andhra Pradesh compared to the rest. The regression analysis of the data reveal that there is a linear decrease trend with a significant negative correlation value (r) = - 0.9031 with a regression equation Y=161.6 - 0.07973X, the regression model of which predicts 23,000 filarial cases in the state of Andhra Pradesh by the year 2024 which is a phenomenal decline of filarial cases from the year 1997 (Table 1) and thus paving the path to improve the public health of the community which would be further accentuated through prophylactic measures such as vaccination.
CONCLUSION
The number of recorded cases of lymphatic filariasis in the year 1997 in the state of Andhra Pradesh (India) is 15,40,000. Whereas by the year 2021 this number reduced to 42,343 as per the report from NVBDCP. This phenomenal decline in the filariasis cases must have been primarily due to the WHO guidelines & directions; and implementation programs by the health workers. In the present study, the regression model predicted 23,000 filarial cases by the year 2024 in the state of Andhra Pradesh. The risk of transmission of microfilariae due to the potential carriers (infected subjects) and insect vectors may further augment the situation, the same would be abated by implementing and planning the prophylactic vaccines (Table 1).
ACKNOWLEDGEMENTS
Authors acknowledge the Centre of Excellence, Department of Biotechnology, VFSTR for providing facilities during the tenure of the work included in the article.
- WHO (2022) Lymphatic filariasis. Available online at: https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis
- Cromwell EA, Schmidt CA, Kwong KT, Pigott DM, Mupfasoni D, et al. (2020). The global distribution of lymphatic filariasis, a geospatial analysis. Lancet Glob Health 8(9): e1186-e1194.
- Babu S, Nutman TB (2014) Immunology of lymphatic filariasis. Parasite Immunol 36(8): 338-346.
- Nutman TB (2001) Blood borne Filarial Infections Wuchereriabancrofti, Brugiamalayi, Brugiatimori, Loa loa Mansonellaperstans and Mansonellaozzardi. Princ Pract Clin Parasitol pp: 433-455.
- Roy N (2018) Elimination of lymphatic filariasis India Updates and way forward. Manipal J Med Sci 3(2): 1-3.
- WHO (2017) Guideline alternative mass drug administration regimens to eliminate lymphatic filariasis. Available online at: https://www.who.int/publications/i/item/9789241550161
- Horton J, Witt C, Ottesen EA, Lazdins JK, Addiss DG, et al. (2000) An analysis of the safety of the single dose, two drug regimens used in programmes to eliminate lymphatic filariasis. Parasitology 121(S1): S147-S160.
- National Health Mission (2022) National Vector Borne Disease Control Programme (NVBDCP). Available online at: https://nhm.gov.in/index4.php?lang=1&level=0&linkid=279&lid=346
- Mukhopadhyay AK, Patnaik SK (2007) Effect of mass drug administration programme on microfilaria carriers in East Godavari district of Andhra Pradesh. J Vector Borne Dis 44(4): 277-280.


