Research Article
Is Advance Age a Factor for Increased Musculoskeletal Hazards Among Nurses?
657
Views & Citations10
Likes & Shares
Background: Nurses are the backbone and integral component of the healthcare industry. Many workplace stressors that can cause injuries and illnesses are present in the nursing work environment, which makes the job of nurses challenging. These stressors or hazards can impair the health of nurses acutely or long term. As per the Bureau of Labor Statistics (BLS, 2012) Nurses sustain occupational injuries and disorders almost twice the national rate of the general population due to their work. Most of the studies in occupational health have focused mainly on worker’s compensation, insurance, absenteeism, and economic consequences towards the organization. Very little focus is on the impact on the life of the workers affected due to workplace injuries and illnesses. The repercussions of these workplace injuries reach the victim’s workplace, home, hospitals, courts, and the local community.
Physical Hazards are one of the most common risks among nurses as their work involves a large amount of weight-bearing task, awkward postures, space limitations, excessive force, and repetitive tasks. However, the study revealed that age is not the precipitating factor towards these injuries.
Objectives: The main goal of the study was to determine musculoskeletal hazards and their relationship with age among nurses in one of the government hospitals in U.A.E.
Methodology: The study was carried out in one of the government hospitals in Dubai, United Arab Emirates between the period of October 2017 till April 2018. A convenience sample was recruited for this study. The sample of this study consisted of 588 participants who worked as direct patient care providers. Data were analyzed using Statistical Package for the Social Sciences (SPSS) Version 21.
Results: SPSS version 21 was used for analysis. Inferential statistical and descriptive statistics evaluation methods were used to analyze the collected data. Chi-square was used for testing the hypotheses. Nurses do face physical hazards in common but are underreported. Data from the sample revealed that the relationship between Age and low back pain was significant.
Conclusion and Recommendation: Physical hazards are commonly observed among young nurses with less experience and need further studies to determine the factors leading to these injuries. As concluded from the current study training and education is a widely adopted strategy for the prevention of musculoskeletal injuries. To include safe patient handling as a part of mandatory competency and to encourage reporting behavior among the staff to analyze the severity of the problem.
Keywords: Physical hazards, Back injuries, Musculoskeletal injuries, Low back pain, Occupational hazards
INTRODUCTION
According to the U. S Bureau of Labor Statistics, health care workers are more prone to muscular-skeletal disorders when compared with other jobs, which are physically more demanding like in construction, mining, and manufacturing [1]. The main reason for musculoskeletal injuries in health care workers is due to positioning, transportation, and assisting patients [2]. Approximately 20% of nursing jobs include patient handling and mobilization; that is the reason adequate training on safe patient handling and mobilization is essential [3]. Activities that involve lifting, bending and awkward postures are considered as work-related risk factors leading to Muscular skeletal disorders [4]. The patient’s weight is a determinant factor, which affects the health of staff, the heavier the patient, the greater, is the physical stress and exertion, which is required to assist the patient during transfer [5]. Both BMI and age are contributing factors towards musculoskeletal strain and pain [6]. The American Nurses Association Health and Safety Survey 2011, published 62% of nurses had reported disabling musculoskeletal injury and it was a major concern and 56% had experienced musculoskeletal pain, which was worsened due to their job nature [7]. Work-related health impairments can cause great human suffering and can incur high costs. Workplace characteristics ranging from policies and safety practices in place [8], work design layout with basic ergonomics [9] can have a major impact on workers. The type and severity of the illnesses or injuries matter a lot to define its consequences and effects e.g. an employee with a severe disabling back injury will face more consequences than an employee with a minor sprain will. Besides the injury and the suffering, depression has a larger impact on the ability to work and the social functioning of the employee [10].
METHODOLOGY
Quantitative descriptive cross-sectional method was used for the study by using demographic variables.
Sources of Data
The focus of the study was based on the primary data obtained from the survey. 60% of staffs from each unit completed the survey to obtain accuracy of results.
Study Setting
The locale of the study was in one of the government hospitals in Dubai, which is a 600 bedded multispecialty hospital, catering the needs of both nationals and multi-nationals. In all there are 1162 nurses working in the hospital.
Sampling and Sample size
The target population for the study were the direct patient care providers and judgmental sampling technique was used, n=588, sample size considered for the study and surveys with missing data were excluded from the study.
Tools used for data collection
Researcher developed and modified the tool, which was adapted from OHS Vulnerability Measure tool, developed at the Institute for Work and Health based in Toronto, Canada, published in the year Jan 2016, as per the need of the study. The reliability and validity of the modified tool was done based on the pilot study and the experts of the same field validated content of the tool.
Statistical discussion
SPSS version 21 was used for analysis. Inferential statistical and descriptive statistics evaluation methods used to analyze the collected data. Chi-square was used for testing the hypotheses.
ETHICAL APPROVAL
The study was reviewed by Dubai Scientific Research Committee (DSRC). Institutional Review Board (IRB) approval was obtained in order to start data collection. The questionnaire and consent form were given to the participants who meet the inclusion criteria. An information sheet was attached with the questionnaire explaining to them the purpose of the study. Participants were assured that the confidentiality and privacy of the answers will be maintained. No names, phone numbers, and identification were required as a part of data.
RESULTS
Data analysis is the important part of the research and represents the relationship between the variables.
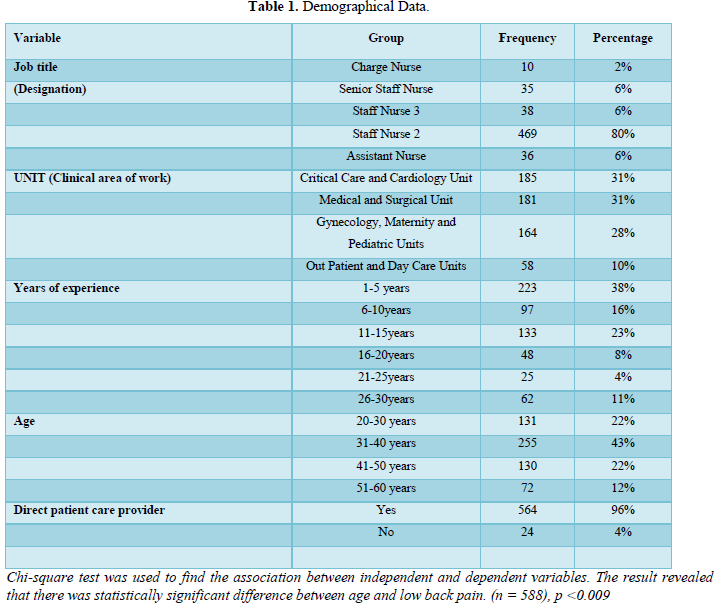
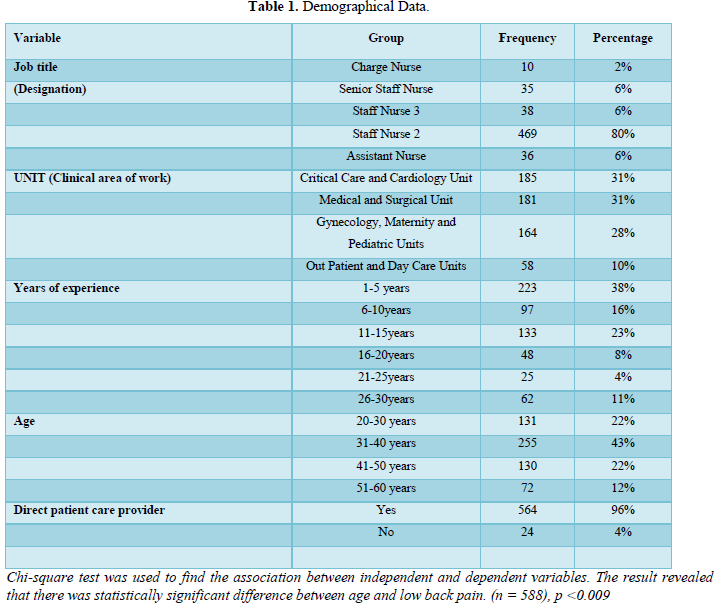
Table 1 presents the participants demographical data, (N= 588 respondents), 2% of the respondents are Charge Nurses working as unit in charge, 6% Senior Staff Nurse, 6% Staff Nurse 3 (direct patient care providers), 80% Staff Nurse 2 (direct patient care providers), 6% Assistant Nurse. The Unit in the sample profile represents the specialties or department of the respondents. Among the respondents, 31% nurses worked in Critical Care and Cardiology Units, 31% in Medical and Surgical Units, 28% from Gynecology, Maternity and Pediatrics Units, 10% from Outpatient and Day-case Unit. Experience profile reflects that respondents with experience of 5 years are 38%, respondents with experience of 6-10 years are 16%, respondents with 11-15 years’ experience are 23%, respondents with 16-20 years’ experience are 8%, experience of 21-25 years are 4% and lastly respondents with 26-30 years are 11%. The age profile of the respondents in the study reveals that 43% participants are between 31-40 years; followed by 22% respondents between 20-30 years, 22% between 41-50 years and 12% between 51-60 years. Job nature of the respondents reflects 96% are direct patient care providers and 4% are unit managers.
DISCUSSION
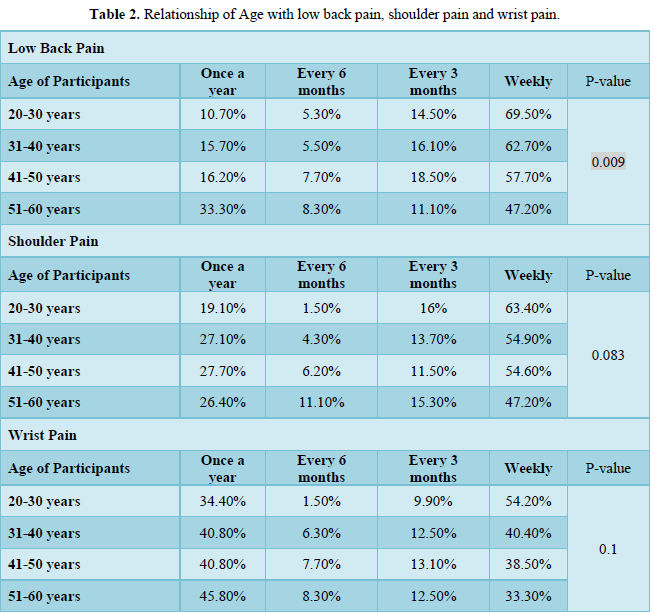
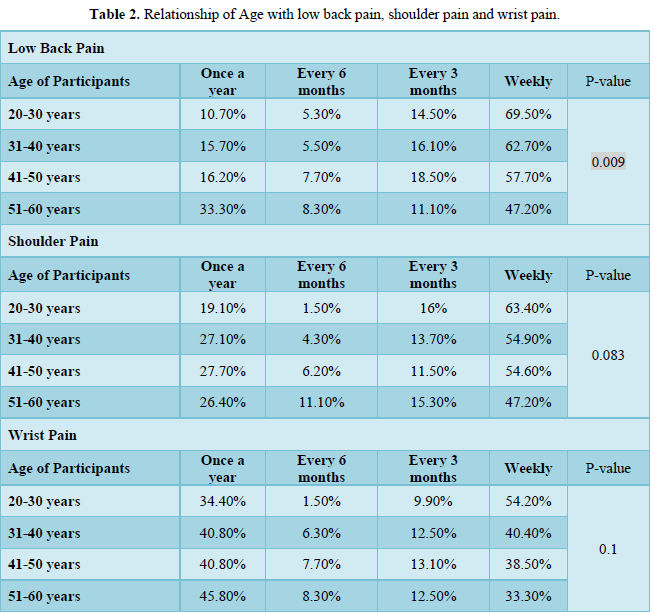
The main goal of the study was to assess the relationship of age with musculoskeletal injuries (MSI) among the nurses. To the best of our knowledge, this was the first study conducted in this hospital. The result of the study suggested that MSI was more common in young nurses. Musculoskeletal injuries are the most common work-related hazard among direct patient care providers. Patient handling and moving is the main cause of musculoskeletal injuries [11]. As per the U.S Department of Labor, low back injury was most frequent among health care providers and was one of the leading causes of absenteeism. Several factors influence work-related injuries like age, type of employment, the status of employment, length of shift, body mass index, and health and wellness activity [12]. From Table 2, it is evident that the age group, which was frequently affected by musculoskeletal pain, was between 20-30 years, and staffs between 51-60 years had the least complaint. Similar findings were noted in a study, the prevalence of low back pain was more in very young nurses, mainly working in intensive care units [13]. In one of the published studies, 73% of work-related injury was noted in workers aged between 25-54 years, 16% of respondents were less than 25 years, and 8% older than 54 years [12]. Musculoskeletal pain is often associated with psychosocial factors and physical workload [14]. The risk of musculoskeletal injuries is noted in occupations, which involves repetitive motion of body parts, forceful efforts, awkward postures, and lifting heavy objects [15]. There are various factors, which increase musculoskeletal injuries among workers like age, gender, hours of work per week, and organization [16]. Despite so much focus on safe patient handling and mobility, nurses still sustain frequent musculoskeletal injuries, and these injuries are underreported [17-18]. Nurses are prone to musculoskeletal injuries throughout their nursing careers [19]. 20% of the nursing work time involves patient handling, which involves strain on the hands and wrists, so adequate training is required to carry these tasks [6]. Safe patient handling is a technique, which requires adequate skill to lift, transfer, and mobilize patients [20]. With the advancement of age, this task becomes more challenging and nurses always consider the patient’s safety first [21]. Many pieces of literature have stated that there is increased risk for injury due to age-related changes, but there is also consent that with age there is a decline in injury rates due to experience, maturity, and the critical decision of older workers [22].
CONCLUSION
Significant relationship of age was observed with low back pain but no relationship of age with shoulder and wrist pain. The age group who mainly reported musculoskeletal pain or injury were the younger nurses aged between 20-30 years. The incidence and prevalence of musculoskeletal pain and injury was among younger nurses aged between 20 to 30 years was noted in this study and this can be mainly due to lack of skill, knowledge and experience of safe patient handling mechanism and needs further study.
RECOMMENDATIONS
Musculoskeletal injuries lead to sickness and absence from work for a longer period of time, which has an economic impact on the organization. Training and education are the widely adopted strategy for prevention of musculoskeletal injuries along with technological developments such as lifting and hoists machine but still, the problem is not resolved as the handling of patients is different from the handling of inanimate objects as each patient’s cognitive status may be different due to a disease condition or drugs.
Measures that can be incorporated are
- To conduct educational programs aimed at the prevention of musculoskeletal injuries including information on proper lifting techniques.
- To include safe patient handling devices as a mandatory competency and assessment for each staff mainly on lifting techniques.
- To encourage reporting behavior among staff to analyze the severity of the problem as musculoskeletal pain or injuries are under-reported.
- Proper record of all injuries and pain to be maintained in the unit and case scenarios to be discussed in the meeting to analyze factors contributing to the incident.
- Encourage the participation of all staff in risk assessment and determination of controls.
- To initiate the return-to-work program by identifying a return-to-work coordinator who can be an occupational physician, ergonomists, nurses, health and safety consultants who can address individual cases, including concerns about their fitness to work and any special work requirements.
FUTURE RESEARCH DIRECTIONS
Staffs compliance on safe patient handling mechanism can be determined.
ACKNOWLEDGEMENT
The author will like to thank Dr. Namrata Arora Charpe her guide for all her guidance, supervision and support during the entire research.
ETHICAL CONSIDERATION
Ethical committee approval was taken from Dubai Research and Scientific Committee. Each respondent duly signed consent form prior to data collection and the respondents were assured that their response would be confidential.
DISCLOSURE STATEMENT
The authors declare that they do not have conflict of interest. All the authors, read and approved the submitted version. All authors confirm that the manuscript is our own original work.
- Collins JW (2010) Safe patient handling & lifting standards for a safer American workforce.
- Schoenfisch AL, Lipscomb HJ, Pompeii LA, Myers DJ, Dement JM (2013) Musculoskeletal injuries among hospital patient care staff before and after implementation of patient lift and transfer equipment. Scand J Work Environ Health 39(1): 27-36.
- Holman GT, Ellison KJ, Maghsoodloo S, Thomas RE (2010) Nurses’ perceptions of how job environment and culture influence patient handling. Int J Trauma Nurs 14(1): 18-29.
- Engels JA, Van Der Gulden JW, Senden TF, Hof BV (1996) Work related risk factors for musculoskeletal complaints in the nursing profession: Results of a questionnaire survey. Occup Environ Med 53:636-641.
- McCoskey KL (2007) Ergonomics and patient handling. AAOHN J 55: 454-462.
- Arvidsson SRN, Bergman S, Arvidsson B, Fridlund B, Tingstrom P (2012) Psychometric properties of the Swedish Rheumatic Disease Empowerment Scale, SWE-RES-23. Musculoskeletal Care 10(2): 101-109.
- Dawson JM (2012) ANA releases 2011 Health and Safety Survey results. Available online at: https://www.myamericannurse.com/ana-releases-2011-health-and-safety-survey-results/
- Patterson JM (1997) Vpp companies’ best practices. Occupational Health & Safety 66: 60-61.
- Hoke GEJ (1997) Ergonomics: One size does not fit all. Telemarketing 16: 28-31.
- Lerner D, Adler D, Hermann RC, Chang H, Ludman EJ, et al. (2012) Impact of a work-focused intervention on the productivity and symptoms of employees with depression. J Occup Med 54(2): 128-135.
- Menzel NN, Brooks SM, Bernard TE, Nelson A (2004) The physical workload of nursing personnel: Association with musculoskeletal discomfort. Int J Nurs Stud 41(8): 859-867.
- Williams A (2013) Collins Academic Skills - Research: B2+. pp: 192. Available online at: https://collins.co.uk/products/9780007507115
- June KJ, Cho S (2011) Low back pain and work-related factors among nurses in intensive care units. J Clin Nurs 20(3-4): 479-487.
- Arvidsson I, Gremark SJ, Dahlqvist C, Axmon A, Karlson B, et al. (2016) Cross-sectional associations between occupational factors and musculoskeletal pain in women teachers, nurses and sonographers. BMC Musculoskeletal Disord 17(1): 35.
- Roquelaure Y, Ha C, Fouquet N, Descatha A, Leclerc A, et al. (2009) Attributable risk of carpal tunnel syndrome in the general population – implications for intervention programs in the workplace. Scand J Work Environ Health 35(5): 342-348.
- Eriksen W (2003). The prevalence of musculoskeletal pain in norwegian nurses’ aides. Int Arch Occup Environ Health 76(8): 625-630.
- Vendittelli D, Penprase B, Pittiglio L (2016) Musculoskeletal injury prevention for new nurses. Workplace Health & Safety 64(12): 573-585.
- Smedley J, Inskip H, Trevelyan F, Buckle P, Cooper C, et al. (2003) Risk factors for incident neck and shoulder pain in hospital nurses. Occup Environ Med 60(11): 864-869.
- Mitchell T, Sullivan OP, Burnett A, Straker L, Rudd C (2008) Low back pain characteristics from undergraduate student to working nurse in Australia: A cross-sectional survey. Int J Nurs Stud 45: 1636-1644.
- Gallagher RN, Susan S (2013) Implementation guide to the safe patient handling and mobility interprofessional national standards. Available online at: https://www.amazon.com/Implementation-Handling-Mobility-Interprofessional-Standards/dp/1558105301
- Daley K (2013) From your ANA president: Safe patient handling and mobility standards lead to healthier nurses and patients. American Nurse Today 8(7): 22.
- Breslin FC, Smith P (2005) Age related differences in work injuries: A multivariate, population based study. Am J Ind Med 48: 50-56.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Alzheimers and Parkinsons Disease
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)

