Research Article
Gestational Age as a Predictor of Successful Vaginal Birth at Term: A Matched Cohort Study
4853
Views & Citations3853
Likes & Shares
Background: Safe Motherhood programmed recommended by World Health Organization (WHO) has been implemented for maternal health care in low-and- middle income countries. The vaginal birth has excellent maternal and newborn outcomes in institutional delivery. This study aimed to determine the gestational age ≤ 40 weeks as one of the predictors of successful vaginal birth.
Methods: A prospective cohort study was conducted at the department of Obstetrics and Gynecology in Chitwan Medical College Teaching Hospital. We admitted low risk mothers in the labor ward were subjected to clinical management of labor and delivery in accordance to the protocol defined by World Health Organization for the induction of labor cohort and matched spontaneous labor cohort, between June 2019 and May 2020 were included in the study. Data were analyzed using the statistical software package SPSS 20.0 version.
Results: Successful vaginal delivery between inductions vs. spontaneous cohorts observed (38.4% vs. 54.5 %.) respectively. Out of 208 vaginal modes of delivery, 71.63% of vaginal delivery occurred at ≤ 40 weeks of gestational age. Gravida was the only significant predictor of successful vaginal delivery, with the odds [aOR: 0.30, 95% CI: 0.153 – 0.615). The gestational age group ≤ 40 weeks odds of successful vaginal delivery [aOR: 1.02, 95% CI: 1.02 (0.583 – 1.795)]. Maternal age and birth weight were not associated with successful vaginal delivery.
Conclusions: Gravida and maternal age were significant predictors of successful vaginal birth. Birth weight was not associated with successful vaginal birth. Gestational age ≤ 40 weeks increases the rate of successful vaginal birth.
Keywords: Induction of labor, Predictors of vaginal birth, Spontaneous labor
INTRODUCTION
Safe Motherhood programmed recommended by World Health Organization (WHO) has been implemented for the reduction of maternal mortality by increasing research evidence, providing evidence-based clinical and programmatic guidance in low-and- middle income countries such as Nepal. Maternal mortality in low-and-middle income countries contributes 94% of the global maternal mortality rate [1]. The rate of primary caesarean delivery is increasing worldwide but its met needs are still inadequate in low-and-middle income countries like ours [2-5]. As the met need of caesarean delivery increasing, mortality due to surgical site wound infection/sepsis as well as a surgical complication is also increasing [6-9]. The successful vaginal birth has excellent maternal and newborn outcomes in institutional delivery with midwifes [10]. The promotion of successful vaginal birth is essence in modern obstetrics management which is the safest mode of delivery in maternal and neonatal health. There are various maternal characteristics of predicting factors for vaginal delivery were identified in retrospective studies such as maternal age, body mass index, Gestational age, Bishop Scores and fetal weight [11,12]. The gestational age at term is one of the most important factors for the successful maternal and new-born outcomes. In clinical obstetrics practice for the management purpose, the term gestational age is divided into main three categories, early (37 0/7 weeks of gestation through-38 6/7 weeks), full term (39 0/7- weeks of gestation through 40 6/7 weeks) and late term (41 0/7- weeks of gestation through 41 6/7 weeks) [13]. Elective induction of labor at term is associated with decreased odds of caesarean delivery when compared with expectant management [14-16]. However, elective induction of labor is only performed before expected date of delivery (40 weeks) when there is clear evidence of high-risk medical indication for it [17]. Clinical obstetrics practice is still prevailed towards expectant management because of a fear of preterm birth. In modern obstetrics, conformation of gestational age becomes easy due to the advance technology in Ultrasound. There are strong evidences that higher the gestational age after 40 weeks gestation, more the risk of surgical intervention or caesarean delivery and also more the risk of adverse perinatal outcome in postdate delivery [18]. Article published in 2015 described that shifting of gestational age of the planed birth towards early gestation 39-40 weeks due to changing in pattern of the clinical practice [19]. There are no evidences of increased risk if elective management or expectant management of labor instituted to pregnancy with low or no risk till its full term [20-23]. Planed delivery within expected date of delivery may increase successful vaginal birth and lower the caesarean rate. It may also promote institutional delivery. So, the objective of this prospective study was to identify the predominant predictors associated with successful vaginal birth in induction and spontaneous labor cohorts. The study question is “Does low-risk pregnancy exposed to labor (either induction or spontaneous) at ≤ 40 weeks of term gestation predicts successful vaginal birth?
METHODS
This was prospective cohort study conducted at the department of Obstetrics and Gynecology in a tertiary care center at Chitwan Medical College Teaching Hospital between June 2019 and May 2020. The period of the study was one year. CMC-IRC reviewed and approved the study documents and provided ethical clearance for the research (Ref; CMC-IRC/075/076-165). Safe Motherhood Programmed as recommended by World Health Organization (WHO) has been implemented in this tertiary care center. We admitted low risk mothers in the labor ward was subjected to clinical management of labor and delivery in accordance to the protocol defined by World Health Organization for the induction of labor cohort and matched spontaneous labor cohort [24]. We included normal or low risk pregnant mother admitted for the induction of labor via routine protocol with Misoprostol as an “induction cohort” and mother admitted for the management of spontaneous labor included as “spontaneous cohort”. The gestational age included in both groups was between 37-42 weeks, singleton, and cephalic presentation. Pregnant mothers in spontaneous labor cohort were “matched cohort” of induction group as inclusion of similar age category and same parity admitted consecutively for the management of labor. We excluded those mothers who has got previous CS, severe hypertensive disorder, gestational diabetes, multiples pregnancies, abnormal lie and severe oligohydramnios cases from the study. The main instruments to record the data was admission sheet, maternity register and operation theatre register of the hospital. We recorded the demographic data such as age, parity, gestational age; labor-related information such as indications for inductions, duration of labor, mode of delivery and Birth weight.
Sample size was calculated using the formula,
n = Z2 x p x (1-p) / e2
= (1.96)2 x (0.1) x (1-0.1) / (0.05)2
=124.467
=125 (in each cohort)
Were,
n=required sample size
Z=1.96 at 95% confidence interval
p=prevalence 10% (induction rate in tertiary hospital of Nepal)
q=1-p
e=margin of error, 5%
Since we used consecutive sampling method, we have included more than required sample size of low-risk mother who attended for induction in one year study period. Data were analyzed using the statistical software package SPSS 20.0 version. Proportion, mean, standard deviation, chi-square p value, odds ratio was calculated. A multivariate logistic regression analysis was done with vaginal birth as the outcome, which was dichotomized into no/cesarean delivery and yes/vaginal. The gestational age also dichotomized into yes/≤ 40 weeks no / >40 weeks. The p-value
RESULTS
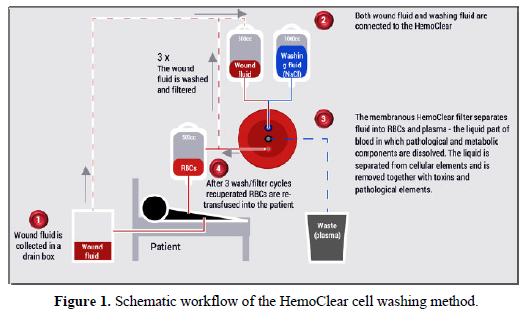
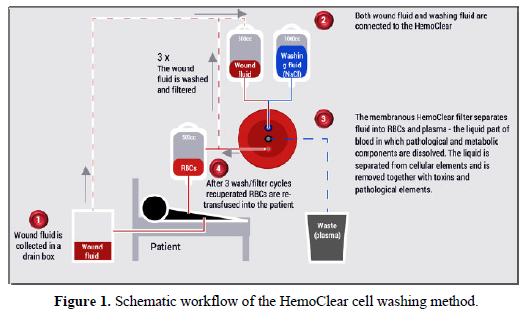
Out of 448 pregnant mothers under study, there were 224 mothers in the “induction cohort” and the same number in matched “spontaneous cohort”. Demography result regarding age shows the mean age of the mother was 24.2 ± 4.1 vs. 24.3 ± 4.2 in the induction and spontaneous cohort respectively. The difference between the two means of age p-value =.828 shows no significant differences in the age group between two cohorts. High rate of vaginal delivery was observed among maternal age group 20-24 and 24-28 years in primigravida and multigravida respectively (Figure 1).
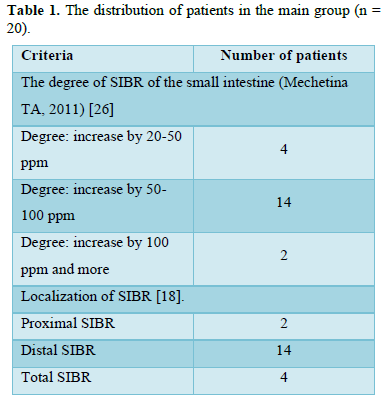
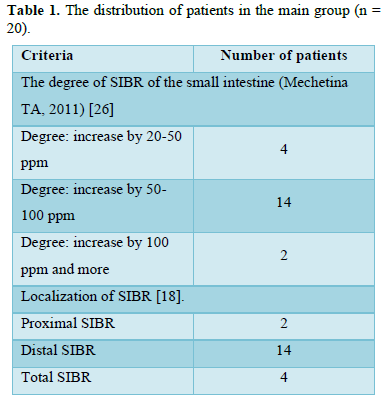
The gravidity and parity related proportions were Primigravida (58%) and multigravida (42%) in each cohort (Table 1). No significant difference (p-value 1.00) was observed in Gravidity and Parity.
The two cohorts were comparable based on maternal age and gravida. The induction cohort had significantly higher gestational age at delivery compared to spontaneous labor cohort (that relates to the existing protocol for induction i.e., induction commonly done after 40 weeks). However, there were 46.4% women, who were induced at ≤ 40 weeks of gestation for the medical indication of previous pregnancy loss and mild group of hypertensive disorders. The birth weight was also significantly higher for induction cohort compared to spontaneous cohort. Induction cohort was strongly associated with higher C-section rate (61.6%) (Table 2)


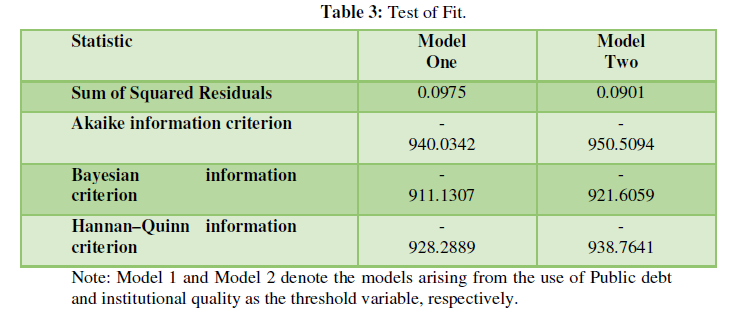
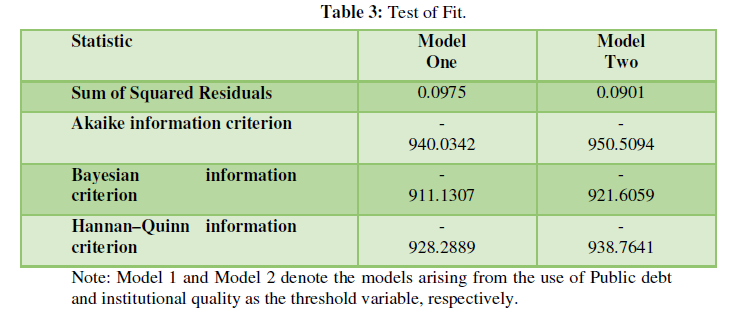
Overall, considering both the cohort, there were 208 (46.4%) successful vaginal deliveries. The remaining 53.6% (n = 240) underwent C-section, hence were categorized as “unsuccessful” vaginal birth (Table 3).
In multivariate logistic regression analysis, for induction cohort, Gravida was the only significant predictor of successful vaginal delivery, with the odds of successful vaginal delivery in primigravid women being 70% less than multigravida women [aOR: 0.30, 95% CI: 0.153 - 0.615). The gestational age group ≤ 40 weeks had slightly increased, but statistically insignificant odds of successful vaginal delivery [aOR: 1.02, 95% CI: (0.583 - 1.795)]. Maternal age and birth weight were not associated with successful vaginal delivery.
DISCUSSION
Induction cohort strongly associated with a higher incidence of caesarean delivery 61.6% vs.45.5% than spontaneous cohort. A study done by by Kjerulff KH et al observed only 24.8% vs. 18.9% in induction and spontaneous cohort respectively [25]. Davey et al. observed in single cephalic primigravida pregnancy population based cross sectional study and [26]. Higher the gestational age after 40 weeks high the caesarean delivery was observed in our study. Gravida was the only significant predictor of successful vaginal delivery in both cohorts, with the odds of successful vaginal delivery in primigravid women being 70% less than multigravida women [aOR: 0.30, 95% CI: 0.153 – 0.615). Gravida was a significant predictor observed in our study. There were significant differences (p value <0.001) observed in mean birth weight of neonates 3122.201±404. vs 2981.75±508.061 grams respectively. The induction cohort had higher birth weight then spontaneous. Birth weight was insignificant predictors of vaginal delivery in our study. The multinomial logistic regression analysis shows that the maternal age: aOR 0.924 (0.873 - 0.978), gravid: aOR 0.415 (0.258 - 0.667) and induction group aOR 0.561 (0.368 - 0.857) were the significant predictors of successful vaginal birth. Higher rate of vaginal delivery was observed among maternal age group 20-24 and 24-28 years. Our findings showed that lower the age higher the prediction of vaginal birth. Successful vaginal birth was seen in multigravida. There is 70% more chance of successful vaginal birth in multigravida mother than primigravida. Induction group had a lesser chance of successful vaginal birth than spontaneous group. In our study, slightly higher rate of successful vaginal delivery was observed in exposure to both cohort in gestational age ≤40 than >40 weeks. Sinkey RG et al reported similar finding on the comparative effectiveness analysis of elective induction of labor at 39 weeks among nulliparous women with non-anomalous singleton, vertex as compared to expectant management [27]. The gestational age group ≤40 weeks and >40 weeks, birth weight was unable to demonstrate the significance predictors. However, lower the gestational age higher the successful vaginal birth was observed in both group in our study. Gestational age may be one of the useful predictors of successful vaginal delivery. Because of small sample population, there is wide range of confidence interval of odds: aOR 1.161 (0.737 - 1.830) showed up to 1.8 time’s higher chance of vaginal delivery when exposed to delivery ≤40 weeks of gestation. Similar finding reported in the retrospective study done by Alleviated et al in the derivation and validation of a model predicting the likelihood of vaginal birth following labor induction [28]. Among the identified predictors, Maternal age, Gravida, Induction cohort were the most common in our study. Other studies found maternal age, BMI, cervical bishop score [29] and parity [28]. The study population were differing with our study we took the matched cohort of similar age group and same parity. We did not consider the factor of Bishop Score because of its high observer differences and poor predictive ability for the success of induction [30]. Balchin I reported that White women and South Asian women differed significantly in their patterns of gestation specific ante partum stillbirth from term onwards, this is a consistent finding with our study [31]. The Several arguments, biases and evidences were issued in the commentary article by Menticoglou SM about “Routine induction of labor at 41 weeks gestation: nonsense consensus” on 2002 AD which might be relevant in the past especially in low resource and obstetrics overloaded settings [32]. Several studies and trials have lacked of evidence of recommendation of induction 39-42 weeks of gestation [33]. In contrary to this opinion, our study finding showed that 86.6% of delivery occurred at ≤40 weeks of gestation in the spontaneous labor group. So, the elective delivery within expected date of delivery (40 weeks) increases the successful vaginal delivery. The opinion about “Induction of labor” given by WHO based on the Cochrane systematic review of 9 trials from 15 countries, the WHO mentioned that there was moderate-certainty evidence suggesting that induction before 41 weeks makes little or no difference to the caesarean section rate whereas there is also moderate-certainty evidence suggesting reduced caesarean section rates in cases where labor induction was done at or after 41 weeks [24]. In Asian countries like ours, the institutional delivery is very low. Elective delivery within 40 weeks may increase the rate of institutional delivery as well as vaginal delivery and improve the fetomaternal outcomes in low and- middle income countries. Some evidences which do favor for the induction of labor before EDD in elective or planed delivery. Majority of pregnant mother on their extreme age are more prone to develop pregnancy associated hypertension, gestational diabetes and other pregnancy relate co morbidities. Higher the gestational age more these co morbidities appear in pregnancy. So that plan delivery at mid of the term is helpful to prevent and reduce from these co-morbidities than expected delivery [34]. A study by Turowski G found that the maturation disorder in the placenta was seen in prolonged pregnancy [35]. In summary, Gravida was the only significant predictor of successful vaginal delivery, with the odds of successful vaginal delivery in primigravid women being 70% less than multigravida women in multivariate logistic regression analysis for the induction cohort, The gestational age group ≤ 40 weeks had slightly increased, but statistically insignificant odds of successful vaginal delivery. Maternal age and birth weight were not associated with successful vaginal delivery.
LIMITATION
A term gestation ≤ 40 weeks variable was unable to demonstrate significant predictors of successful vaginal delivery probably due to small sample population and single center study. The bias was prevailed in induction group whom was done in the majority only after 41 weeks of gestation according to the WHO protocol. The protocol was not changed during the study. The significance of the planed exposure to induction at 39 weeks (just before EDD) would be beneficial to promote vaginal birth. This action decline 30% of the CS rate which would optimize the neonatal outcome and also decrease the maternal morbidity and mortality. But, careful selections and conformation of the gestational age optimize the outcome.
CONCLUSION
The planned exposure to labor within ≤40 weeks would be beneficial in low-risk mothers to optimize vaginal birth. The other predictor like maternal age and fetal weight fails to demonstrate a significant association for successful vaginal birth.
- Trends in maternal mortality (2000 to 2017) estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019. Available online at: https://apps.who.int/iris/handle/10665/327596
- Samdal LJ, Steinsvik KR, Pun P, Danp P, Roald B, et al. (2016) Indications for Cesarean Sections in Rural Nepal. J Obstet Gynaecol India 66(Suppl 1): 284-288.
- Rai SD, Regmi PR, Teijlingen EV, Wood J, Ganesh DG, et al. (2018) Rising Rates of Caesarean Section in Urban Nepal. J Nepal Heal Res Counc 16(41): 479-480.
- Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, et al. (2016) The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990-2014. PLoS One 11(2): e0148343.
- Luz G, José MB, Jeremy AL, Ana PB, Mario M, et al. (2010) The Global Numbers and Costs of Additionally Needed and Unnecessary Caesarean Sections Performed per Year: Overuse as a Barrier to Universal Coverage. Available online at: https://www.who.int/healthsystems/topics/financing/healthreport/30C-sectioncosts.pdf
- Kawakita T, Landy HJ (2017) Surgical site infections after cesarean delivery: epidemiology, prevention and treatment. Mat Heal Neo Per 3: 12.
- Holmer H, Kamara MM, Bolkan HA, Alex VD, Fatu F, et al. (2019) The rate and perioperative mortality of caesarean section in Sierra Leone. BMJ Global Health 24: e001605.
- Raagab AE, Mesbah YH, Brakat RI, Zayed AA, Alsaammani MA (2014) Re-laparotomy after cesarean section: risk, indications and management options. Med Arch 68(1): 41-43.
- Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, et al. (2014) The Global cause of maternal death; a WHO systematic Analysis. Lancet 2(6): PE323-E333.
- Grünebaum A, McCullough LB, Sapra KJ, Brent RL, Levene MI, et al. (2014) Early and total neonatal mortality in relation to birth setting in the United States, 2006-2009. Am J Obstet Gynecol 211(4): 390-391.
- Alavifard S, Meier K, Shulman Y, Rohan D, George T (2019) Derivation and validation of a model predicting the likelihood of vaginal birth following labor induction. BMC Pregnancy Childbirth 19: 130.
- Eggebø TM, Wilhelm BC, Hassan WA (2015) A model to predict vaginal delivery in nulliparous women based on maternal characteristics and intrapartum ultrasound. Am J Obstet Gynecol 213: 362.
- Spong CY (2013) Defining “Term” Pregnancy: Recommendations from the Defining “Term” Pregnancy Workgroup. JAMA 309(23): 2445-2446.
- Darney BG, Snowden JM, Cheng YW, Jacob L, Nicholson JM, et al. (2013) Elective induction of labor at term compared with expectant management: Maternal and neonatal outcomes. Obstet Gynecol 122(4): 76-769.
- Sinkey RG, Lacevic J, Reljic T, Iztok H, Kelly SG, et al. (2018) Elective induction of labor at 39 weeks among nulliparous women: The impact on maternal and neonatal risk. Plos one 13(4): e0193169.
- Souter V, Painter I, Sitcov K, Aaron BC (2019) Maternal and newborn outcomes with elective induction of labor at term. Am J Obstet Gynecol 220: 273.
- Cheng YW, Kaimal AJ, Snowden JM, Nicholson JM, Caughey AB (2012) Induction of labor compared to expectant management in low-risk women and associated perinatal outcomes. Am J Obstet Gynecol 207(6): 502.
- Delnord M, Blondel B, Drewniak N, Kari K, Francisco B, et al. (2014) Varying gestational age patterns in cesarean delivery: an international comparison. BMC Pregnancy Childbirth 14: 321.
- Samdal LJ, Steinsvik KR, Pun P, Roald B, Erik B, et al. (2016) Indications for Cesarean Sections in Rural Nepal. J Obstet Gynaecol India 66: 284-288.
- Na ED, Chang SW, Ahn EH, Sang HJ, Young RK, et al. (2019) Pregnancy outcomes of elective induction in low-risk term pregnancies: A propensity-score analysis. Medicine (Baltimore) 98(8): e14284.
- Guerra GV, Cecatti JG, Souza JP, Anibal F, Carroli, et al. (2011) Elective induction versus spontaneous labor in Latin America. Bull World Health Organ 89(9): 657-665.
- Nassar N, Schiff M, Roberts CL. (2013) Trends in the distribution of gestational age and contribution of planned births in New South Wales, Australia. PLoS One 8(2): e56238.
- Metcalfe A., Lisonkova S, Joseph K (2015) The association between temporal changes in the use of obstetrical intervention and small- for-gestational age live births. BMC Pregnancy Childbirth 15: 233.
- WHO recommendations for induction of labor (2011) Geneva: World Health Organization. Available online at: https://www.ncbi.nlm.nih.gov/books/nbk131965/
- Kjerulff KH, Attanasio LB, Edmonds JK, Kozhimannil KB, Repke JT (2017) Labor induction and cesarean delivery: A prospective cohort study of first births in Pennsylvania, USA. Birth 44(3): 252-261.
- Davey M, King J (2016) Caesarean section following induction of labor in uncomplicated first births- a population-based cross-sectional analysis of 42,950 births. BMC Pregnancy Childbirth 16: 92.
- Sinkey RG, Lacevic J, Reljic T, Anthony OO, Charles JL, et al. (2018) Elective induction of labor at 39 weeks among nulliparous women: The impact on maternal and neonatal risk. PLoS One 13(4): e0193169.
- Alavifard S, Meier K, Shulman Y, George T, Rohan D (2019) Derivation and validation of a model predicting the likelihood of vaginal birth following labour induction. BMC Pregnancy Childbirth 19: 130.
- Kolkman DGE, Verhoeven CJM, Brinkhorst SJ, van der Post JAM, Pajkrt E, et al. (2013) The Bishop Score as a Predictor of Labor Induction Success: A Systematic Review. Am J Perinatol 30(8): 625-30.
- Faltin-Traub EF, Boulvain M, Faltin DL, Extermann P, Irion O (2004) Reliability of the Bishop score labor induction at term. Eur J Obstet Gynecol Reprod Biol 112: 178-181.
- Balchin I, Whittaker JC, Patel RR, Lamont RF, Steer PJ (2007) Racial variation in the association between gestational age and perinatal mortality: Prospective study. BMJ 334(7598): 833.
- Menticoglou SM, Savas MM (2003) Routine induction of labor at 41 weeks gestation: Nonsensus consensus: BIJOG 109(5): 485-491.
- Mya KS, Laopaiboon M, Vogel JP, Jose GC, Joao PS, et al. (2017) Management of pregnancy at and beyond 41 completed weeks of gestation in low-risk women: A secondary analysis of two WHO multi-country surveys on maternal and newborn health. Reprod Health 14(1): 141.
- Roberts CL, Algert CS, Morris JM, Ford JB (2015) Increased planned delivery contributes to declining rates of pregnancy hypertension in Australia: A population-based record linkage study. BMJ Open 5(10): e009313.
- Turowski G, Vogel M (2018) Review and view on maturation disorders in the placenta. APMIS 126(7): 602-612.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Pathology and Toxicology Research
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)



