7122
Views & Citations6122
Likes & Shares
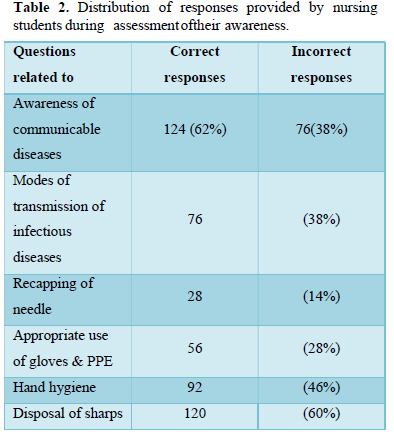
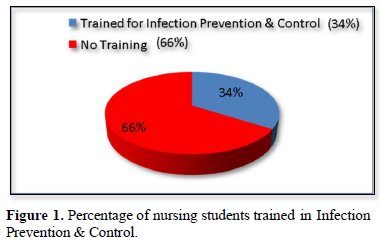
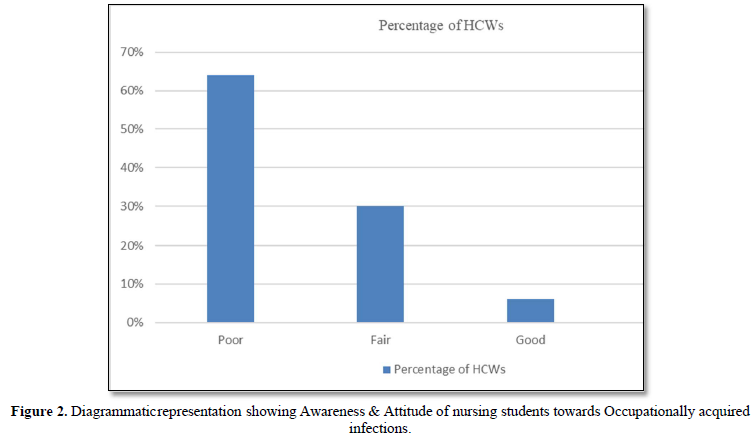
Occupationally acquired infections represent an important health issue and exposure to infectious material poses a serious risk to healthcare workers in health care settings. This study was undertaken to screen nursing students regarding their awareness, attitude & behavior towards infectious diseases and occupational hazards and to give recommendations regarding interventions to prevent occupationally acquired infections. A cross-sectional survey was conducted using self-administered questionnaire to a total of 200 nursing students as study population. We found that their awareness about epidemiological characteristics of Infectious diseases & occupational hazards was insufficient. The recommendations to prevent occupational exposure to such infections by the results of this study are continuous education, training about infection control & safe work practices, implementing Standard precautions, Transmission based precautions, PPE, improved availability of resources and immunization against Hepatitis B and other vaccine- preventable diseases.

- WHO-HWF-Working paper (2021) The impact of COVID-19 on health and care workers; a closer look at deaths. Available online at: https://apps.who.int/iris/handle/10665/345300
- Kermode M, Jolley D, Langkham B, Thomas S, Crofts N (2005) Occupational exposure to blood and risk of bloodborne virus infection among health care Workers in rural north India health care Am J Infect Control 33: 34-41.
- World Health Organization (2002) The World Health Report, Box 4.2002. Geneva, Switzerland, 2002. Available online at: htpp://www.who.int/whr/2002/chapter4/en/index8
- Mullan RJ, Baker EL, Hughes JM, Bell DM, Jaffe HW, et (1989) Centers for disease control and prevention: Guidelines for prevention of transmission of HIV&HBV to health-care and public-safety workers. MMWR Morb Mortal Wkly Rep 38: 1-37.
- Centers for Disease Control and Prevention (1998) Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic MMWR Morb Mortal Wkly Rep 47: 1-39.
- Beltrami EM, Williams IT, Shapiro CN, Chamberland ME (2000) Risk and management of blood-borne infections in health care workers. Clin Microb Rev 13: 385-407.
- Update. (1988) Universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus, and other bloodborne pathogens in health care settings. MMWR 37: 377-382, 387-388.
- Kermode M, Jolley D, Langkham B, Thomas MS, Holmes W, et al. (2005) Compliance with Universal/Standard Precautions amongst care Am J Infect Control 33: 27-33.
- Padmaja GV, Mrudula AS (2019) Screening of Health care personnel for Human Immuno Deficiency virus (HIV), Hepatitis B(HBV) and Hepatitis C(HCV) Infections in Mahatma Gandhi Memorial Hospital, Warangal, Telangana. Caims Org J 17(1): 11-16.
- Moloughney BW (2001) Transmission and postexposure management of blood borne virus infections in the health care setting: Where are we now? CMAJ 165: 445-451.
- Rapiti E, Prüss ÜA, Hutin Y (2005) Sharps Assessing the Burden of Disease from Sharps Injuries to Health-Care Workers at National and Local Levels. World Health Organization: Geneva. (WHO Environmental Burden of Disease Series, No. 11. Available online at: https://apps.who.int/iris/handle/10665/43051
- Wałaszek M, Kołpa M, Wolak Z, Rózanska A, Wójkowska MJ (2017) Poor hand hygiene procedure compliance among polish medical students and physicians the result of an ineffective education basis or the impact of organizational culture? Int J Environ Res Public Health 14:
- Garus PA, Górajski M, Szatko F (2018) Did legal regulations change the reporting frequency of sharp injuries of medical personnel? Study from 36 hospitals in Łód´z Province, Int J Occup Med Environ Health 31: 37-46.
- Kocur E, Sliwa RB, Grosicki S (2016) Analysis of cases of occupational exposure to blood recorded in the city hospital in Zabrze in 2006-2015. Przegl Epidemiol 70: 603-615.
- Szczypta A, Rózanska A, Bulanda M (2014) Analysis of occupational exposure of healthcare workers in the years 1998-2013 for bloodborne pathogens on the example of the hospital of the surgical Med Pracy 65: 723-732.
- Gholami A, Borji A, Lotfabadi P, Asghari A (2013) Risk factors of needlestick and sharps injuries among healthcare Int J Hosp Res 2: 31-38.
- Sharma S, Gupta A, Arora A (2010) Knowledge, attitude and practices on needle- stick and sharps injuries in tertiary care cardiac hospital: A Indian J Med Sci 64: 396-401.
- Richards MJ, Jenkin GA, Johnson PDR (1997) Universal precautions: Attitudes of Australian and New Zealand Med J Aust 166: 138-140.
- Lymer UB, Schütz AA, lsaksson B (1997) A descriptive study of blood exposure incidents among healthcare workers in a university hospital in J Hosp Infect 35: 223-235.
- Panagakos FS, Silverstein J (1997) Incidence of percutaneous injuries at a dental school: A 4-year retrospective Am J Infect Control 25(4): 330-334.
- Sepkowitz KA (1996) Occupationally acquired infections in health care workers. Part Ann Intern Med 125(10): 826-834.
- Henein MN, Lloyd L (1997) HIV, hepatitis B, and hepatitis C in the code one trauma Am Surg 63: 657-659.
- McCarthy GM, MacDonald JK (1997) The infection control practices of general dental Infect Control Hosp Epidemiol 18: 699-703.
- Cleveland JL, Gooch BF, Lockwood SA (1997) Occupational blood exposures in dentistry: A decade in Infect Control Hosp Epidemiol 18: 717-721.
- Aiken LH, Sloane DM, Klocinski JL (1997) Hospital nurses’ occupational exposure to blood: Prospective, retrospective and institutional Am J Public Health 87: 103-107.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Allergy Research (ISSN:2642-326X)




