265
Views & Citations10
Likes & Shares
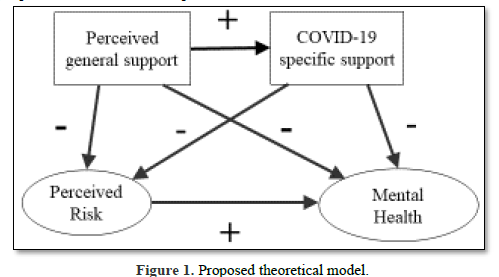
Figure 1 shows the proposed theoretical model derived from the stress process model and previous research findings. The proposed model includes perceived risk of contracting COVID-19 as a mediator between social support and mental health. In this study, social support effects were examined in terms of two indicators: perceived general support and COVID-19-specific support.
METHOD
Study Design and Participants
This study employed a cross-sectional descriptive correlational design. Convenience sampling was used to recruit nursing students from a Japanese public university located in a suburban portion of the Tokyo metropolitan area. During the transitional period from the second to the third wave of the COVID-19 pandemic in October 2020 [21] the researchers used a nursing student listserv to send all nursing students (N=307) study information and an invitation to complete the online study survey. Each participant completed the survey anonymously using Google Forms. The survey’s first section contained an informed consent form that participants had to complete before they could proceed. This study was approved by the university’s Institutional Review Board. Under the inclusion criteria, participants had to be (1) undergraduate nursing students who had completed at least 1 year of study or graduate nursing students currently enrolled in the university and (2) willing to volunteer to participate in the study. First-year undergraduate nursing students were excluded because COVID-19 policy required that they study exclusively online, and thus they were not present on campus during the study period. Of the 307 nursing students invited to participate, 110 completed the survey, for a response rate of 35.8%.
Measures
Survey items were drawn from a previous survey conducted during the 2009 influenza A (H1N1) pandemic in Hong Kong [20,22]. The English-language version of this self-administered survey, which was created by a Taiwanese research team [20,23] was translated into Japanese and back-translated into English for validation purposes. During the translation process, the survey items’ language underwent cultural adaptation for application in Japan. Finally, 25 items of the translated survey were selected for use in this study. Specifically, the three domains of the Japanese survey contained items chosen to examine relationships among social support (perceived general support and COVID-19-specific support), perceived risk of contracting COVID-19 (absolute susceptibility and relative susceptibility), and mental health problems (anxiety and mental distress).
Demographic characteristics
The survey collected information on participants’ demographic characteristics, including their age, educational level (bachelor’s/master’s/PhD program), gender, and place of residence (campus dormitory/apartment near campus/living with family).
Social support
Social support was measured in terms of two indicators: perceived general support and COVID-19-specific support. Perceived general support was assessed using three items that asked participants to indicate their overall satisfaction with support from family, friends, and faculty during the previous 7 days using a 5-point Likert response scale ranging from 0 (extremely dissatisfied) to 4 (extremely satisfied). Total scores ranged from 0 to 12, with higher scores indicating greater perceived general support. The Cronbach’s alpha for the three items was 0.81 in a previous study [20] and 0.62 in this study. In contrast to perceived general support, COVID-19-specific support refers to received support needed specifically during the COVID-19 pandemic. COVID-19-specific support was assessed using five items and a 3-point Likert scale. Respondents were asked whether they possessed a sufficient amount of five COVID-19-specific items: personal protective equipment (PPE), information on infection prevention, living expenses, medical expenses, and psychological support. The response scale ranged from 1 (insufficient) to 3 (sufficient), with total scores ranging from 5 to 15. Higher total scores indicated possession of greater amounts of COVID-19-specific support. The Cronbach’s alpha for the five items was 0.75 in a previous study [20] and 0.70 in this study.
Perceived risk of contracting COVID-19
Perceived risk of contracting COVID-19 was measured using two indicators: absolute susceptibility and relative susceptibility [23]. Absolute susceptibility was assessed as an individual’s perceived risk of infection with COVID-19 within the next month, while relative susceptibility was assessed as an individual’s perceived risk of infection with COVID-19 compared to anyone else except family members. The two items employed a 7-point Likert response scale ranging from 0 (none) to 6 (certainty). Higher scores indicated a greater perceived risk of contracting COVID-19. The Cronbach’s alpha for the two items was 0.80 in a previous study [23] and 0.67 in this study.
Mental health
Mental health was assessed in terms of two indicators: anxiety and mental distress. Anxiety was measured using a Japanese translation of the State-Trait Anxiety Inventory (STAI) A-State [24]. This study employed 10 STAI A-State items and a 4-point Likert scale ranging from 1 (not at all) to 4 (very much). Scores of positive state items were reversed. Higher mean scores indicated more intense states of anxiety. The Cronbach’s alpha for the 10 items was 0.85 in this study. Mental distress was measured using one item and a scale ranging from 0 (never) to 4 (extremely severe). Higher scores indicated more severe mental distress.
Data Analysis
Structural equation modeling (SEM) was performed to test the hypothesized model (Figure 1) illustrating relationships among three domains: social support, perceived risk, and mental health. Descriptive statistics, student’s t-test, analysis of variance (ANOVA) and Pearson correlations were performed to explore interpretation of the SEM results. Bentler and Chou [25] stated that the minimum sample size for the application of SEM should be 10 participants per free parameter. As the model used in this study included eight free parameters, the study’s sample size of 110 participants was sufficient to perform SEM. The maximum likelihood estimation method was applied for the SEM model. Goodness of fit was determined using χ2/df (p>.05) and the comparative fit index (CFI > .95), normed fit index (NFI > .95), and root mean square error of approximation (RMSEA < .05). Data analyses were performed using two programs: SPSS version 28 for descriptive statistics and bivariate correlations, and AMOS version 28 for SEM (Armonk, NY: IBM Corp).
RESULTS
Descriptive Statistics
Descriptive statistics for demographic characteristics, social support, perceived risk, and mental health are presented in Table 1.
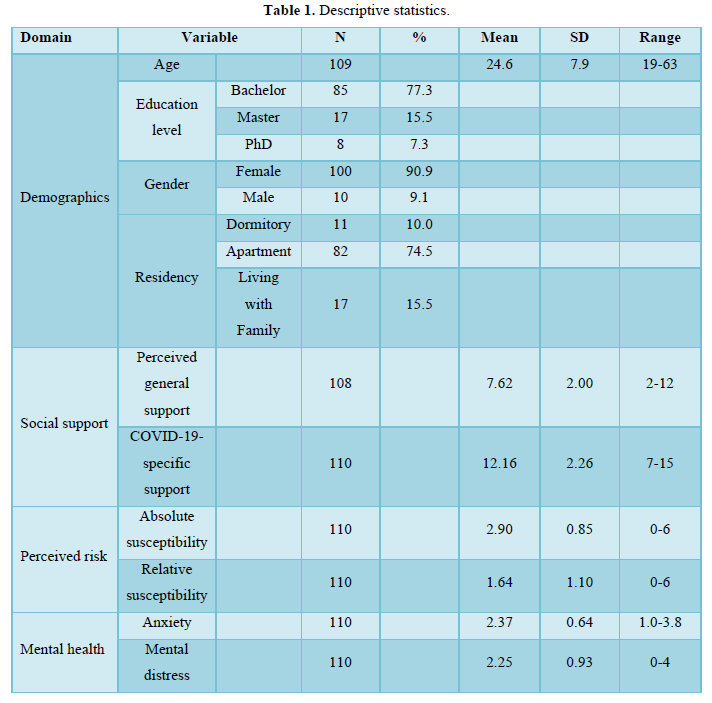
Most participants were undergraduates (77.3%), were females (90.9%), and lived in school dormitories or apartments separately from their families (84.5%). Regarding social support, among the three sources of perceived general support, the mean score for family support (2.81) was higher than the scores for friend support (2.46) and faculty support (2.34). Among the five sources of COVID-19-specific support, the mean score for PPE (2.75) was the highest, followed by the scores for information on infection prevention (2.58), living expenses (2.27), medical expenses (2.33), and psychological support (2.23). Additionally, the percentage of participants who responded that they had sufficient PPE was 77.3%, information on infection prevention was 63.6%, money for living expenses was 47.3 %, money for medical expenses was 47.3%, and psychological support was 41.8%.
Bivariate Correlations
Table 2 shows bivariate correlations among social support, perceived risk, and mental health variables. Regarding social support, lower perceived general support was associated with higher absolute susceptibility (r=-.22, p<.05) under perceived risk and with greater mental distress (r=-.24, p<.05) under mental health. Lower COVID-19-specific support was associated with higher perceived risk (absolute susceptibility: r=-.24, p<.05; relative susceptibility: r=-.19, p<.05) and with greater mental health symptoms (anxiety: r=-.24, p<.05; mental distress: r=-.36, p<.01).
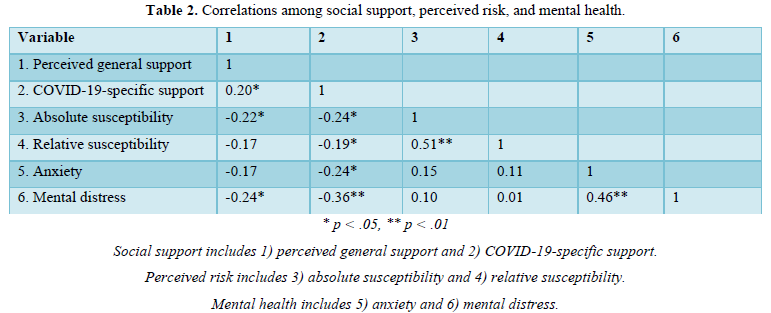
Correlations were also examined between the individual variables of social support and mental health. With respect to perceived general social support, lower family support was associated with higher anxiety (r = -.21, p<.05) and greater mental distress (r = -.19, p<.05), while lower faculty support was significantly associated only with greater mental distress (r = -.26, p<.01). For individual COVID-19-specific support variables, both insufficient living expenses and insufficient medical expenses were significantly associated with higher anxiety (r = -.21, p<.05; r = -.22, p<.05) and with greater mental distress (r = -.21, p<.05; r = -.21, p<.05). Moreover, lower psychological support was significantly associated with higher anxiety (r = -.30, p<.01) and greater mental distress (r = -.50, p<.01). In addition, correlations were examined between individual variables of social support and perceived risk. Among perceived general support variables, lower family support was significantly associated with higher absolute susceptibility (r = -.20, p<.05) under perceived risk. For individual COVID-19-specific support variables, insufficient living expenses were significantly associated with higher absolute susceptibility (r = -.26, p<.01) and higher relative susceptibility (r = -.25, p<.01) under perceived risk, while insufficient medical expenses were significantly associated only with higher absolute susceptibility (r = -.22, p<.05) under perceived risk.
SEM Results
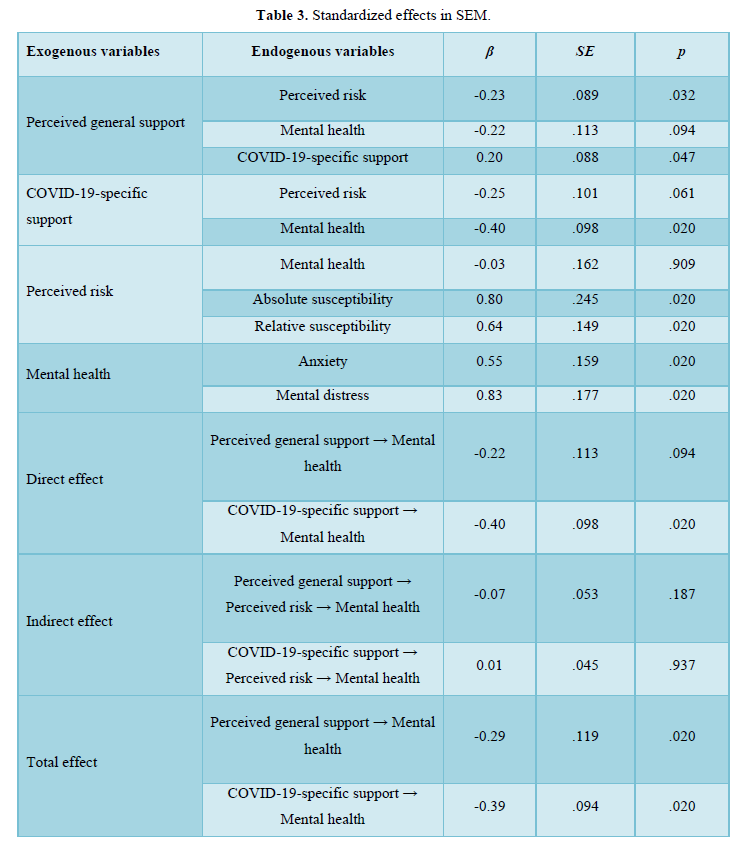
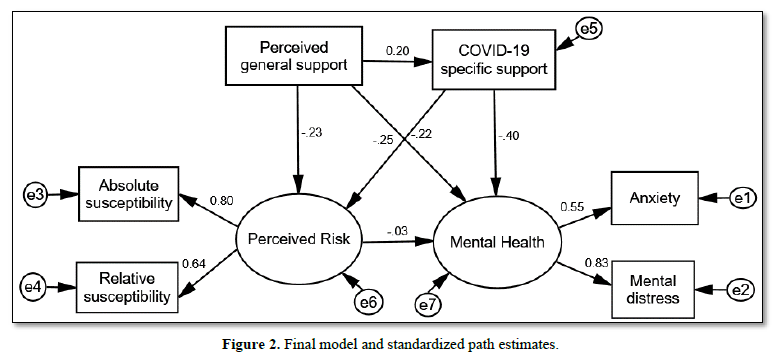
Figure 2 and Table 3 show the SEM results. The model, which consisted of perceived general support, COVID-19-specific support, perceived risk (absolute and relative susceptibility), and mental health (anxiety and mental distress), showed acceptable model fit indices: χ2/df = 0.45, CFI = 1.00, NFI = 0.98, and RMSEA = 0.00. All variables in the model satisfied the normality assumption required for SEM. The model included three paths from perceived general support to perceived risk (β = -.225, p = .032), mental health (β = -.221, p = .094), and COVID-19-specific support (β = .201, p = .047), whereas it included two paths from COVID-19-specific support to perceived risk (β = -.253, p = .061) and mental health (β = -.395, p = .020). Thus, the alleviating effect of social support (as perceived general support) on perceived risk was supported, and the alleviating effect of social support (as COVID-19-specific support) on mental health symptoms was verified in this study sample. However, the model showed that the path from perceived risk to mental health was non-significant (β = -.027, p = .909). Furthermore, we observed non-significant indirect effects of perceived general support (β = -.072, p = .187) and COVID-19-specific support (β = .007, p = .937) on mental health through perceived risk, even though both perceived general support (β = -.293, p = .020) and COVID-19-specific support (β = -.389, p = .020) showed significant total effects on mental health. Therefore, SEM results did not support an indirect effect of social support (both perceived general support and COVID-19-specific support) on mental health through perceived risk.
DISCUSSION
Our study investigated relationships among social support (perceived general support and COVID-19-specific support), perceived risk of COVID-19 infection, and mental health in Japanese nursing students during the transitional period from the second to the third wave of the COVID-19 pandemic in October 2020. Our SEM model showed that perceived general support exerted a direct effect that reduced students’ perceived risk of COVID-19 infection, while COVID-19-specific support had an alleviating direct effect on students’ mental health problems. These findings are consistent with previous study results indicating that in nursing students, perceived support was useful in alleviating fear of infection [12,17,26] whereas under COVID-19-specific support, having sufficient PPE [12,13,27] sufficient infection prevention information [14,28] and fewer financial problems were helpful in reducing anxiety and stress. Consequently, perceived general support may be effective in lessening perceived risk among nursing students, whereas COVID-19-specific support, provided in sufficient amounts, may be beneficial in alleviating their mental health problems. With respect to correlations between the types of social support and perceived risk, we showed that family support under perceived general support and having money for living expenses and medical expenses under COVID-19-specific support were significantly associated with lower absolute susceptibility under perceived risk. This contrasts with a study among nursing students in the United States that reported perceived general support from friends significantly reduced perceived risk, while perceived general support from both family and educators did not [16]. The difference between Graves et al.’s findings and our own is likely due to cultural differences between the United States and Japan. Suzuki [29] reported that Japanese college students were more emotionally and financially dependent on their families than American college students. During the pandemic, most of the Japanese participants in this study lived physically apart from family due to the university’s infection prevention policies, and this separation increased their living expenses. At the same time, most nursing students lost part-time jobs and were prohibited from working, even in healthcare facilities, due to government infection prevention advisories [30]. Given the financial hardships experienced by many students and their exacerbation of students’ perceived risk, we conclude that universities should provide nursing students with additional financial support such as scholarships during a pandemic to reduce their perceived risk. This is especially important for students who have difficulties obtaining financial support from their families who may also be experiencing financial problems during a pandemic. Regarding the effects of social support on mental health during the COVID-19 pandemic, previous studies have shown associations between adequate social support and reduced mental health symptoms in nursing students [4,12,20,26,31,32]. In our study, bivariate correlations showed that family support and faculty support under perceived general support and living expenses, medical expenses, and psychological support under COVID-19-specific support were significantly associated with fewer symptoms of mental health problems. Thus, not only perceiving sufficient support from family and faculty, but also receiving sufficient financial and psychological support appears to be critical to mitigating mental health problems among nursing students during a pandemic. In addition, the potential value of pandemic-specific social support for alleviating mental health problems in nursing students warrants future investigation. Notably, the absence of a significant association between perceived risk and mental health in the SEM model is inconsistent with previous studies [15,16]. Studies conducted during the first wave of COVID-19 (April and May 2020) demonstrated that students with a lack of PPE [12,13,26] and insufficient virus information [14] experienced greater mental health problems. In contrast, we collected data during the transitional period from the second to the third wave of the pandemic in Japan (October 2020). Although both periods lacked established infection prevention and vaccination measures, most of our study participants possessed sufficient PPE and information on infection prevention during the transitional period from the second to the third wave, which was likely not the case during the first wave. It is likely that sufficient PPE and infection prevention information reduced the negative effects of the COVID-19 experience on their mental health, especially in the initial phase of the pandemic. Additionally, as the pandemic progressed over time, nursing students may have strengthened their self-concepts, reducing the mental health impact of any perceived risk of infection. Previous studies have shown that self-concepts such as coping [15,27,33-35] perceived control [36] and resilience [17] were significantly associated with better mental health among nursing students during COVID-19. Thus, the relationship between perceived risk and mental health may change by reinforced self-concepts under pandemic. Furthermore, although both perceived general support and COVID-19-specific support had significant beneficial total effects on mental health, we found that the indirect effects of social support on mental health through perceived risk were non-significant. As a possible explanation for the absence of indirect effects, the model showed another mediating factor, COVID-19-specific support, between perceived general support and mental health. In this light, Melrose [37] demonstrated that the relationships between received support and both perceived (general) support and mental health strengthened when support was actually needed. Thus, the mediating effect of COVID-19-specific support (received support) on the relationship between perceived general support and mental health may have been stronger if our data had been collected during the initial stage of the pandemic, the critical period when students most needed pandemic-specific support. Consequently, when the opportunity arises in the future, the mediating effect of received support between perceived support and mental health should be explored in the early pandemic period.
Implications for Nursing Education
Our results indicated the importance of financial and psychological support under COVID-19-specific support to alleviate nursing students’ mental health symptoms, as nursing students with insufficient living and medical expenses and poor psychological support had higher anxiety and mental distress. Nursing educational institutions should prepare sufficient financial and psychological support systems for future public crises, such as emergent scholarships, special tuition waivers, and accessible free counseling services. Additionally, our findings highlighted the importance of faculty support for nursing students’ mental health during a pandemic, because students with less perceived general support from faculty experienced more mental distress. This finding was consistent with a previous study showing that nursing students who perceived faculty support as good or excellent had fewer anxiety symptoms [32]. Given students’ need for faculty support during times of crisis, nursing educators should proactively establish innovative educational programs including instruction for building strong self-care practices and resilience. Van der Riet [38] showed in their systematic review before the COVID-19 pandemic that teaching nursing students self-care theories and skills, such as mindfulness meditation was effective to alleviate their mental stress in both academic and clinical settings. Zhang [17] demonstrated that both lower resilience and fear of COVID-19 mediated alleviating effects of perceived support on PTSD among campus-quarantined nursing students. In preparation for future public crises like this pandemic, schools of nursing should also ensure that faculty have the needed resources for their own self-care and resilience to optimize their own well-being and serve as role models. Incorporating self-care content into the nursing curriculum is increasingly important as rising pre-pandemic rates of burnout and mental health problems among nurses were magnified by the pandemic [39]. Wellness programs need to be integrated across the continuum of education from the nursing school curriculum through professional development programs in healthcare organizations. Having effective academic-practice partnerships is a key mechanism to support the educational preparation and well-being of nurses, and advance nursing practice.
Study Limitations
We used a cross-sectional study design, which did not allow us to determine causal relationships. If it had been possible to perform a longitudinal study, the path directions could have been based on the time axis, which would have been useful for validating the model. In addition, because our recruitment was restricted to one university operating under an infection quarantine policy during the pandemic and the sample size was relatively small, the findings may have limited generalizability, and the observed reliability of some measures was low. To obtain more generalizable and reliable findings, it would be useful to establish a research cooperative in which multiple Japanese research institutions collect nursing student data in a consistent manner during a public health crisis. Finally, the relationships examined in our study may be time-sensitive according to the stages of the pandemic. In the past, the stressful environments resulting from unpredicted and prolonged disasters have led to severe mental health struggles [40]. Longitudinal research involving data collection at various time points during a public health crisis would be needed to verify the reported relationships among social support, perceived risk, and mental health.
CONCLUSION
Our study showed that under social support, perceived general support had an alleviating effect on nursing students’ perceived risk of COVID-19 infection, while COVID-19-specific support had an alleviating effect on their mental health problems. As aspects of COVID-19-specific support, both financial and psychological support lessened perceived risk and mental health symptoms in nursing students. Although longitudinal research is necessary to further explore relationships among social support, perceived risk, and mental health in nursing students at various points during a pandemic, nursing educators can use our findings as evidence in developing innovative strategies for enhancing social support for nursing students now and in preparation for a future public health crisis.
- Mulyadi M, Tonapa SI, Luneto S, Lin W-T, Lee B-O (2021) Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurse Educ Pract 57: 103228.
- Thomas LMB (2022) Stress and depression in undergraduate students during the COVID-19 pandemic: Nursing students compared to undergraduate students in non-nursing majors. J Prof Nurs 38: 89-96.
- Bartlett ML, Taylor H, Nelson JD (2016) Comparison of mental health characteristics and stress between baccalaureate nursing students and non-nursing students. J Nurs Educ 55(2): 87-90.
- Sveinsdóttir H, Flygenring BG, Svavarsdóttir MH, Thorsteinsson HS, Kristófersson GK, et al. (2021) Predictors of university nursing students’ burnout at the time of the COVID-19 pandemic: A cross-sectional study. Nurse Educ Today 106: 105070.
- Bai W, Xi H, Zhu Q, Wang Z, Han L, et al. (2021) Changes in nursing students' career choices following the COVID-19 pandemic in China. Front Psychiatry 12: 657021.
- Lopez V, Anderson J, West S, Cleary, M (2022) Does the COVID-19 pandemic further impact nursing shortages? Issues Ment Health Nurs 43(3): 293-295.
- Ma Z, Wang D, Zhao J, Zhu Y, Zhang Y, et al. (2022) Longitudinal associations between multiple mental health problems and suicidal ideation among university students during the COVID-19 pandemic. J Affect Disord 311: 425-431.
- Ministry of Health, Labor and Welfare (2010) Situation Update. Available online at: https://www.mhlw.go.jp/english/topics/influenza_a/situation_update/index.html
- World Health Organization (2020) WHO Director-General’s opening remarks at the media briefing on COVID-19. Accessed on: March 11, 2020. Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19
- Tanji F, Kodama Y (2021) Prevalence of psychological distress and associated factors in nursing students during the COVID-19 pandemic: A cross-sectional study. Int J Environ Res Public Health 18(19): 10358.
- Takaoka H, Ishido T, Yabushita Y (2021) Thoughts of students before nursing practice during the Covid-19 pandemic. JFH 15: 55-68.
- Casafont C, Fabrellas N, Rivera P, Olivé-Ferrer MC, Querol E, et al. (2021) Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: A phenomenological research study. Nurse Educ Today 97: 104711.
- Rodríguez AJ, Hernández MA, Romero BC, Martínez AA, Prado LMC, et al. (2021) Experiences and perceptions of nursing students during the COVID-19 crisis in Spain. Int J Environ Res Public Health 18(19): 10459.
- Türkleş S, Boğahan M, Altundal H, Yaman Z, Yilmaz M (2021) Diaries of nursing students during the COVID-19 pandemic: A qualitative descriptive study Int J Environ Res Public Health 18(16): 8556.
- Alsolais A, Alquwez N, Alotaibi KA, Alqarni AS, Almalki M, et al. (2021) Risk perceptions, fear, depression, anxiety, stress and coping among Saudi nursing students during the COVID-19 pandemic. J Ment Health 30(2): 194-201.
- Graves RJ, Harrell M, Barinas JL, Taylor SE, Fruh SM, et al. (2022) Effects of the perceived risk of contracting COVID-19 on nursing students' well-being. J Nurs Educ 61(11): 641-645.
- Zhang D, Qin L, Huang A, Wang C, Yuan T, et al. (2023) Mediating effect of resilience and fear of COVID-19 on the relationship between social support and post-traumatic stress disorder among campus-quarantined nursing students: A cross-sectional study. BMC Nurs 22(1): 164.
- Sugimoto K, Fukuzawa RK, Togoobaatar G, Park CG, Vonderheid SC (2023) Factors associated with mental health among undergraduate nursing students early in the COVID-19 pandemic: An integrative review. Int J Nurs Educ Scholarsh 20(1).
- Li DJ, Ko NY, Chen YL, Wang PW, Chang YP, et al. (2020) COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: A Facebook survey. Int J Environ Res Public Health 17(12): 4479.
- Pearlin LI (1999) Stress and mental health: A conceptual overview. In A. V. Horwitz & T. L. Scheid (Eds.), A handbook for the study of mental health: Social contexts, theories, and systems. Cambridge University Press. pp: 161-175.
- World Health Organization (2023) Japan: WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/region/wpro/country/jp
- Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R (2014) Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infect Dis 14: 169.
- Pramukti I, Strong C, Sitthimongkol Y, Setiawan A, Pandin M, et al. (2020) Anxiety and suicidal thoughts during the COVID-19 pandemic: Cross-country comparative study among Indonesian, Taiwanese, and Thai university students. J Med Internet Res 22(12): e24487.
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA (1983) Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press.
- Bentler, P. M., & Chou, C. P. (1987) Practical issues in structural modeling. Sociol Method Res 16(1): 78-117.
- Li D, Zou L, Zhang Z, Zhang P, Zhang J, Fu W, et al. (2021) The psychological effect of COVID-19 on home-quarantined nursing students in China. Front Psychiatry 12: 652296.
- Savitsky B, Findling Y, Ereli A, Hendel T (2020) Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurs Educ Pract 46: 102809.
- Gallego G, Campillo CM, Carrión MA, Balanza S, Rodríguez GM, et al. (2020) The COVID-19 pandemic and its impact on homebound nursing students. Int J Environ Res Public Health 17(20): 7383.
- Suzuki O (1999) A comparative study of late adolescents in Japan and the U. S.: The degree of post-parental independence and adjustment. Seishin Stud 92: 376-358.
- Japan Association of Nursing Programs in Universities Quality Improvement Committee for Nursing Education. (2021).
- De Gagne JC, Cho E, Park HK, Nam JD, Jung D (2021) A qualitative analysis of nursing students' tweets during the COVID-19 pandemic. Nurs Health Sci 23(1): 273-278.
- Fitzgerald A, Konrad S (2021) Transition in learning during COVID-19: Student nurse anxiety, stress, and resource support. Nurs Forum 56(2): 298-304.
- Cheng L, Guo X, Liu H, Chen Q, Cui R (2021) Hope, death anxiety and simplified coping style scores of nursing students during the outbreak of COVID-19: A cross-sectional study. Medicine (Baltimore) 100(34): e27016.
- Savitsky B, Findling Y, Ereli A, Hendel T (2021) Nursing students in crisis mode: Fluctuations in anxiety during the COVID-19-related lockdown. Nurs Educ 46(3): E33-E38.
- Zhu Y, Wang H, Wang A (2021) An evaluation of mental health and emotion regulation experienced by undergraduate nursing students in China during the COVID-19 pandemic: A cross-sectional study. Int J Ment Health Nurs 30(5): 1160-1169.
- Kondo A, Abuliezi R, Niitsu K, Naruse K, Oki T, et al. (2023) Factors related to mental health effect among nursing students in Japan and the United States during the coronavirus pandemic: A cross-sectional study. Int J Ment Health Nurs 32(1): 186-198.
- Melrose KL, Brown GDA, Wood AM (2015) When is received social support related to perceived support and well-being? When it is needed. Pers Individ Dif 77: 97-105.
- Van der Riet P, Levett JT, Aquino RC (2018) The effectiveness of mindfulness meditation for nurses and nursing students: An integrated literature review. Nurs Educ Today 65: 201-211.
- Melnyk BM, Hsieh AP, Tan A, Teall AM, Weberg D, et al. (2022) Associations Among Nurses' Mental/Physical Health, Lifestyle Behaviors, Shift Length, and Workplace Wellness Support During COVID-19: Important Implications for Health Care Systems. Nurs Adm Q 46(1): 5-18.
- Terayama T, Shigemura J, Kobayashi Y, Kurosawa M, Nagamine M, et al. (2021) Mental health consequences for survivors of the 2011 Fukushima nuclear disaster: A systematic review. Part 2: Emotional and behavioral consequences. CNS Spectrums 26(1): 30-42.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Rheumatology Research (ISSN:2641-6999)



