Letter to Editor
Mother and Child Health in COVID Times!
4549
Views & Citations3549
Likes & Shares
This letter-to-the-editor gives a brief insight of Pakistan’s fractured health system during COVID times.
Pakistan being a low-middle-income country with a fractured healthcare system still struggles with poor maternal and child health outcomes and economic fragilities in the pandemic. Therefore, the entire nation is going through a difficult situation to cater maternal child health problems with limited resources at hand. Doctors being observant of their oath are trying their best to save mothers and save lives, but their redeployment to isolation centers has become a challenge itself to cater the situation. Although, the health structure is overwhelmed due to the pandemic, but the collectivistic culture of Pakistani people has proved to be a silver lining in hard times. However, Pakistani government shall take strict actions for public health policy reinforcement and measures to tackle the situation with the allocation of sufficient funds and mitigation strategies for the provision of maternal services for pregnant females, to study irregular health trends emerged in the pandemic.
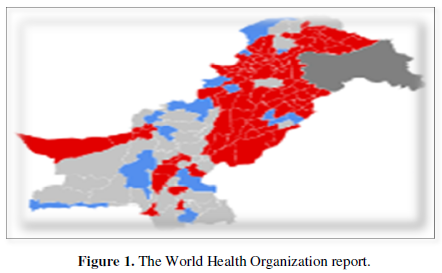
The year 2021 started with a grim reality of spiking 173,331,478 coronavirus cases with an approximate 3,735,571 deaths globally, as the World Health Organization reports (Figure 1) [1].
Pakistan is among the six countries accounting for 50% of global maternal deaths [2]. Therefore, Pakistan being a low-middle-income country with a fractured healthcare system still struggles with poor maternal and child health outcomes and economic fragilities in the pandemic. Globally, Mother, Newborn, and Child Health indices showed an additional 30% maternal and newborn deaths due to reduced access to essential services during the COVID-19 outbreak [3]. Following Pakistan’s National Institute of Population Studies, higher maternal mortality in rural areas was observed due to scarcity of basic maternal units and resources at hand. Also, evidence of the fact that 63.33% Pakistani population resides in rural areas, estimated 178 deaths per 100,000 live births [4]. Further, the higher incidence of hemorrhage was also observed in the post-partum period that accounted for maternal mortality, who were previously dealt by untrained dais/midwives and birth attendants in rural areas referring to domiciliary midwifery services. Also, the risk of thrombosis in pregnancy rose, due to which many doctors suggested the use of anticoagulant prophylaxis in patients with COVID-19 [5]. Therefore, being a health professional at Medicare Hospital, Rawalpindi in collaboration with the London School of Hygiene and Tropical Medicine, the risk of PPH in pregnant females was assessed. However, a remarkable suspension of MCH services, delayed routine follow-up visits, and scheduled labor and C-sections due to national lock-down were observed. It became more challenging for us as a nation due to the redeployment of physicians and staff at isolation centers and consistent lockdowns to cater to maternal and child health problems. The daily grind of limited personal protective equipment and dealing with a large flock of maternal complications spurred fear and confusion among the doctors. Adding to this, a case of an infected pregnant female managed to hide her infection, which later on became a reason for transmission to the physicians and paramedic staff in the provision of perinatal services to her.
Although the Pakistani health care structure was overwhelmed due to the current emergency, no any rational planning was devised by the health authorities regarding MCH services, which in return escalated maternal and child mortality. The deterioration in maternal condition requiring immediate hospitalization was due to onset of COVID-19 related symptoms that occurred more often before the child delivery [6]. Moreover, a positive outlook of the situation was the introduction of telemedicine and video conferencing by some doctors in different areas across Pakistan via mobile units for postpartum consultations - alternate to major lock-down practices. Also, people among different communities tried to banish cultural barriers and differences to help pregnant females in dire need to forge the gap between crisis and limited health care accessibility. Pregnant females were provided with vitamins and folic acid supplementation, which were already in shortage in the market. Health professionals being observant to their oath, require the Pakistani government to take strict actions for public health policy reinforcement and measures to tackle the situation with the allocation of sufficient funds and mitigation strategies for the provision of maternal services for pregnant females, to study irregular health trends emerged in the pandemic, so to devise evidence-based health policy decisions. Also, cooperation from all the stakeholders is expected to establish community-based education regarding limited duplication and resource wastage in the provision of MNCH services amidst the COVID pandemic. Hopefully, we will get through this!
- WHO (2021) WHO Coronavirus dashboard Retrieved on 8th Available online at: https://covid19.who.int
- The Express Tribune (2020) Keeping Mothers safe While Battling Covid-19. Available online at: https://tribune.com.pk/story/2180499/6- keeping-mothers-safe-battling-covid-19
- Stein D, Ward K, Cantelmo C (2020) Estimating the potential impact of COVID-19 on mothers and newborns in low-and middle-income countries. Heal Policy Plus. Available online at: https://medium.com
- Jafarey SN (2002) Maternal mortality in Pakistan-compilation of available data. J Pak Med 52 (12): 539-544.
- Benhamou D, Keita H, Ducloy BA, CARO Working Group (2020) Coagulation Changes and Thromboembolic Risk in COVID-19 Obstetric Patients. Anaesth Crit Care Pain Med 39(3): 351-353.
- Toro DF, Gjoka M, Lorenzo DG, Seta DF, Maso G, et al. (2020) Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect 27(1): 36-46.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Advances in Nanomedicine and Nanotechnology Research (ISSN: 2688-5476)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)
- Food and Nutrition-Current Research (ISSN:2638-1095)
- Proteomics and Bioinformatics (ISSN:2641-7561)



