Research Article
The Role of an Early Maintenance Treatment in Bipolar Disorder: The Experience at San Raffaele Hospital Mood Disorder Center in Milan
4882
Views & Citations3882
Likes & Shares
Background: We previously reported that beginning lithium therapy within the first ten years of illness predicts better preventive outcomes than beginning it later in a mixed sample of patients affected by Major Depressive Disorder and Bipolar Disorder (BD). In this study, we aimed at replicating these results in BD, and evaluating clinical markers that may be associated with the response to stabilization therapy.
Methods: Two hundred fourteen BD subjects receiving stabilization therapy (lithium, anticonvulsants, or antipsychotics) were studied. Clinical data were collected using NIMH Life Chart method. We divided the sample into three groups, according to the initiation time of maintenance treatment. The outcome of preventive therapy was evaluated calculating the gradient between the recurrence index before and after starting the treatment. Data were analyzed using multiple logistic regression analyses.
Results: Seventy-seven percent of the patients were responders, with 4.5 years as average time of maintenance treatment. Variables significantly associated with the outcome of preventive therapy were use of lithium as first-line treatment (p=0.02), starting preventive therapy within 5 years from the illness onset (p<0.0001), and high recurrence index before treatment (p<0.0001). The presence of psychotic manifestations turned out to be the only factor that negatively influenced the response to preventive therapy (p=0.03).
Conclusion: We confirmed the importance of an early intervention in BD: starting lithium therapy within five years from illness onset is more effective than treatments delivered later. Our data suggest that the onset time of lithium therapy can be considered as a new prognostic factor; indeed, an early onset could improve patient’s long-term prognosis, while a late onset is associated with the progression of BD. Referring to recently proposed staging models, we suggest using the time of initiation of maintenance therapy as a new parameter to stage BD patients and, therefore, to provide appropriate interventions.
Keywords: Bipolar Disorder, Early intervention, Stabilization therapy, Lithium
INTRODUCTION
Bipolar Disorder (BD) is a common, burdensome, and lifelong psychiatric disorder, causing impairment of psychosocial functioning. The World Health Organization's Global Burden of Disease Study reports BD as the sixth leading cause of years lost due to disability [1]. As new mood recurrences are experienced by the patients, the frequency and severity of episodes in the course of the disorder increases [2], while the duration of euthymic periods decreases with the increase in the number of episodes [3,4]. However, when evaluating the complexity of BD it is necessary to consider the affective dimension together with other concomitant conditions, including comorbid anxiety [5], substance abuse [6], personality disorders [7], and suicidal thoughts or behaviors [8]. With the co-occurrence of comorbidities, the patients might show a worsened clinical outcome with a chronic course of the disorder; in turn, this progression increases the risk of developing resistance to pharmacological treatments [9]. There is evidence that the chronic course of the disease can determine permanent alterations in the neuronal activity, making the patient more prone to experience recurrences, regardless of external circumstances. Indeed, according to the Kindling Hypothesis [10], the cyclic pattern of episodes appears to acquire an intrinsic autonomous rhythm with a lower impact of stressful experiences in triggering new episodes [11]. Therefore, an effective maintenance treatment is necessary to interrupt this vicious cycle and reduce the burden associated with the disorder.
The mood stabilizer lithium has been the standard pharmacological treatment for BD over the last 60 years [12]. The goal of maintenance treatment is the prevention of future mood episodes, both manic/hypomanic and depressive, or at least the decrease in the number or the intensity of episodes [13]. However, there are still disagreements in the timing of initiation of this treatment: some studies show that lithium may be more effective when administered in the early phases of BD [14,15], even though this indication is not unanimously shared [16,17].
Our previous results [14] suggested that the early beginning of lithium treatment has a good preventive effect for future relapses. We aimed at confirming those results in a BD sample, and evaluating clinical markers that may be eventually associated with the effectiveness of the maintenance therapy, improving the patient’s long-term prognosis.
MATERIALS AND METHODS
Patients’ characteristics
The sample included 214 subjects (84 males, 130 females) affected by BD (135 type I, 79 type II). Patients were recruited from the Outpatient Center of the Mood Disorder Unit at San Raffaele Hospital in Milan, from September 2018 to July 2019.
Inclusion criteria were diagnosis of Bipolar Disorder type I or type II according to DSM-5 criteria, being in a euthymic state for at least 9 months (defined as having a 24-item Hamilton Depression Rating Scale
Among the patients recruited, 32 (15%) were excluded from the analysis due to lack of recollected information, poor adherence, or inadequate tolerability to maintenance therapy.
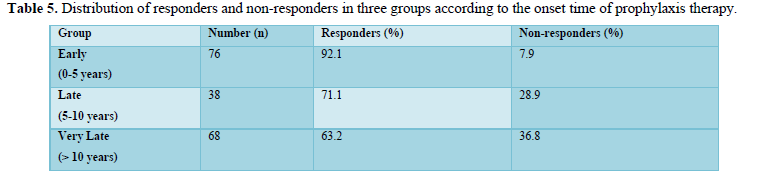
We divided the remaining 182 (85%) subjects into three groups, according to the time point of administration of the mood stabilizer:
-“Early group”, including patients who initiated the preventive therapy within five years from the onset of illness (n=76);
-“Late group”, including patients who initiated the preventive therapy between five and ten years after the onset of illness (n=38);
-“Very Late group”, including patients who initiated the preventive therapy after ten years from the onset of illness (n=68).
Recurrence rate assessment
The recurrence rate of the disease was measured using the recurrence index (RI), defined as the ratio between the number of episodes and the months of duration of the illness. We calculated two distinct RIs, respectively before and after starting to take the maintenance therapy: pre-treatment RI =number of episodes/months of duration of the illness before treatment X 100; on-treatment RI =number of recurrent episodes/months of duration of the treatment X 100.
The efficacy of the prophylactic treatment was evaluated using the difference between pre-treatment RI and on-treatment RI (RI gradient). RI gradient was used to define treatment outcome: we considered the response to maintenance therapy effective when RI gradient > 0. RIs and their derivatives were calculated for any kind of recurrence, and individually for depressive and manic episodes, with and without psychotic features.
Statistical analyses
Data analysis was performed using the software STATISTICA 7.0. A p-value lower than 0.05 was considered to indicate a statistically significant difference. Clinical and demographic variables were obtained through descriptive analysis.
Response to therapy, measured as the RI gradient, was processed as a dependent variable against other variables. We carried out two different multiple logistic regression analyses: first, we considered as variables of interest current age, age of onset, polarity at onset, pre-treatment RI, occurrence of psychotic features, family history of mood disorders, hospitalizations, stressful events, comorbidities, type of Bipolar Disorder (type I or type II); the second analysis includedas variables onset time of prophylaxis (“early”, “late” and “very late” group), age at therapy initiation, duration, and type of therapy.
RESULTS
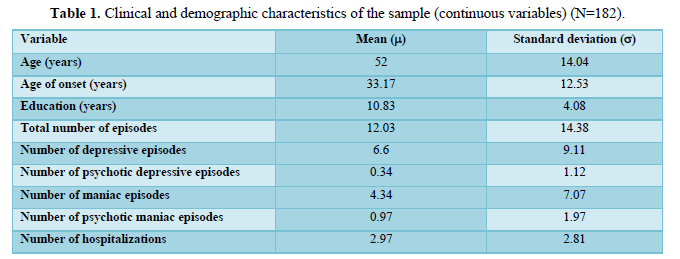
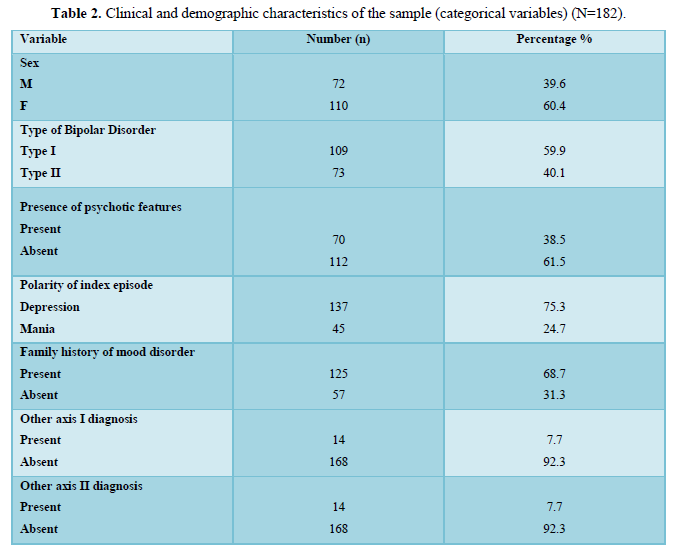
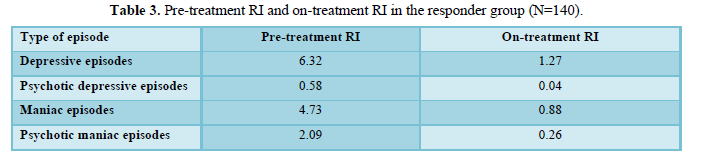
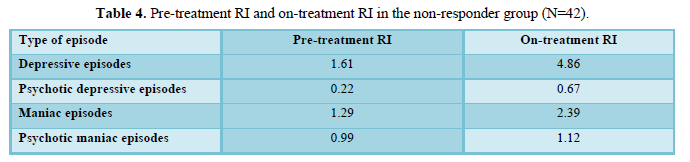
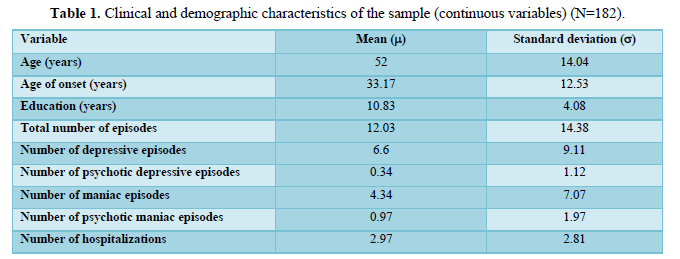
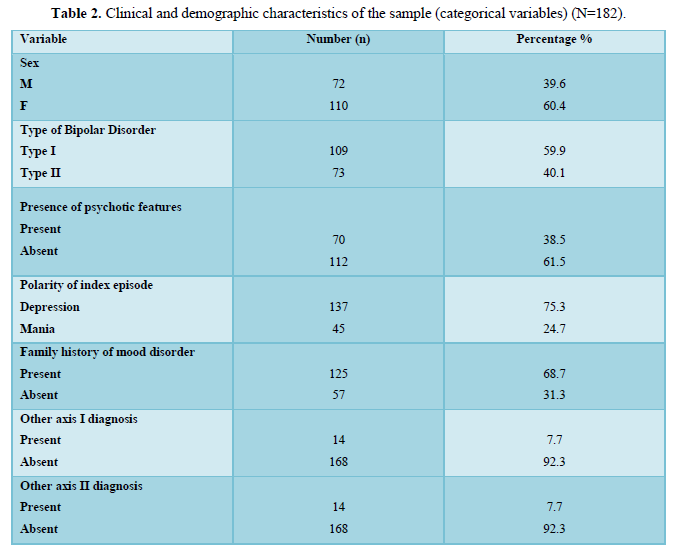
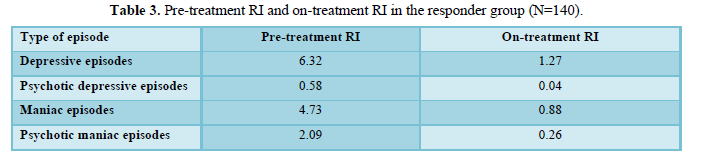
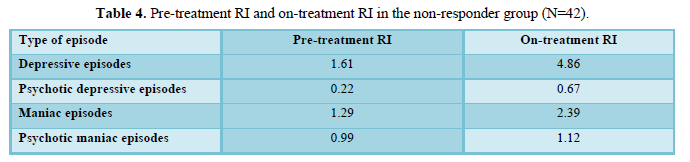
Table 1 and Table 2 summarize the clinical and demographic characteristics of the sample. The average time of maintenance therapy was 54 months. Seventy-seven percent (N=140) of patients were considered responsive to preventive therapy, according to a positive RI gradient, while the remaining 23% (N=42) were considered non-responders. Table 3 and Table 4 show individual RI gradients for manic and depressive episodes, with and without psychotic features, respectively in the responder and the non-responder group.
One hundred eighteen patients (65%) received lithium salts alone as maintenance therapy, while the remaining 64 patients, received valproate alone (6.1%), lithium in combination with valproate (5.1%), lithium in combination with carbamazepine (3.0%), haloperidol alone (2.5%), lithium in combination with haloperidol (2.0%), or other treatments (16.3%).
Treatment outcome, measured as RI gradient, was analyzed by logistic analyses. In the first logistic analysis on stepwise multivariate logistic regression, the “pre-treatment RI” (t=5.31; P<0.0001) and the “psychotic features during the course of the disease” (t=-2.07; P=0.03) were the only variables significantly associated with the outcome of preventive therapy. Thus, a better treatment outcome (higher gradient values) was related to an initial worse trend of the disease, with a higher recurrence index than non-responders (13.01 vs 4.08). Moreover, the group of responders showed a lower percentage of patients with a clinical history of psychotic symptoms, compared to the group of non-responders (34.3% vs 52.4%).
In the second logistic analysis on stepwise multivariate logistic regression, the “type of therapy” (t=-2.35; P=0.02) and the “onset time of lithium prophylaxis”(“early”, “late” and “very late” group) (t=-4.06; P<0.0001) were the only variables significantly associated to the outcome of preventive therapy. Particularly, responders received more frequently lithium monotherapy (67.8%), lithium in combination with valproate or carbamazepine (9.2%), valproate monotherapy (6.4%), haloperidol monotherapy (3.5%), lithium in combination with haloperidol (2.8%); non-responders, instead, took more frequently lithium monotherapy (57.1%), risperidone monotherapy (7.1%), valproate monotherapy (7.1%), valproate in combination with haloperidol or olanzapine (7%), lithium in combination with valproate (4.7%), gabapentin monotherapy (2.3%). Besides, when considering the ratio between responders and non-responders according to the onset time of lithium prophylaxis, the “early group” showed a significantly higher percentage of responders (92.1%) compared to “late group” (71.1%) and “very late group” (63.2%), as shown in Table 5.
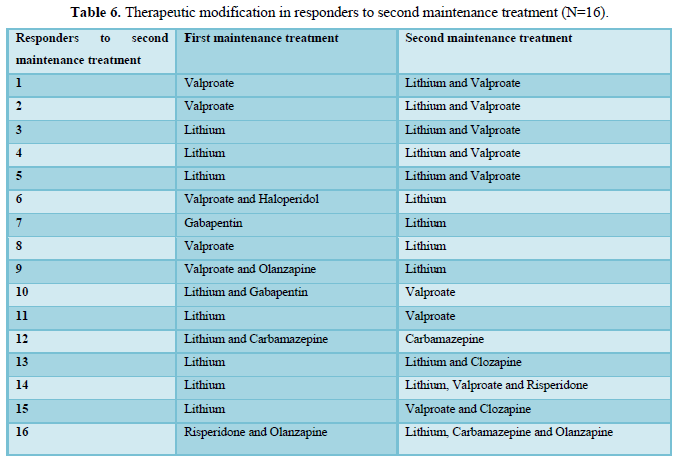
When a patient was considered non-responder to the maintenance treatment, a new mood stabilizer was considered, either alone or in combination. Among the non-responders included in our study (N=42), 54.8% received a new stabilizing treatment for an average period of 41 months. Sixteen patients (69.6%) responded to the new therapy.
Table 6 reports the previous and new maintenance treatment for each new responder.
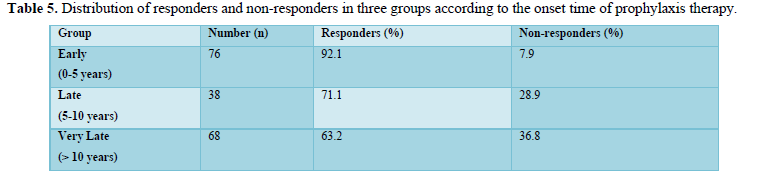
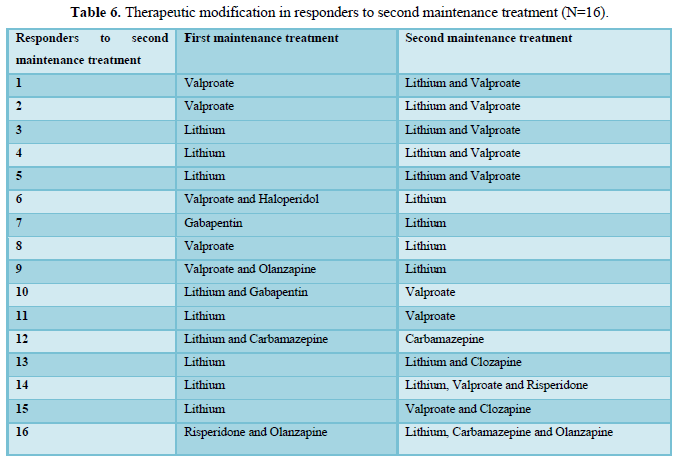
Table 6 reports the previous and new maintenance treatment for each new responder.
DISCUSSION
The need for maintenance therapy in BD is crucial: if depressive and manic episodes usually has a favorable prognosis, thanks to their self-limitedness and wide responsiveness to acute treatments, the risk of relapse or recurrence is very high and progressively increasing in the course of the illness. Given this clinical trend, the use of mood stabilizers is considered the gold standard as a maintenance treatment.
In our study, lithium was confirmed to be used as the first choice in the prevention of new recurrences in BD, considering that it was prescribed to 65% of the sample. Among the analyzed patients (N=182), 77% responded to the therapy, and among those receiving lithium (N=118), 80.5% achieved a favorable outcome, as indicated by a lower RI, in agreement with previous studies [19]. Besides, our results confirm that lithium fits the definition of mood stabilizers, given its ability to prevent episodes of both polarities [20,21].
More interestingly, the type of maintenance treatment significantly correlateswith the response to therapy, suggesting a different stabilizing potential for each preventive strategy. In particular, responders received more frequently lithium inmonotherapy or in combination with an anticonvulsant then non-responders; on the other hand, a significant percentage of non-responders received risperidone in monotherapy or valproate in monotherapy or in combination with an antipsychotic. Our findings are partly in line with other studies [13,22], which have found a differential effect of various stabilizing strategies concerning depressive and manic episodes. Indeed, antipsychotics and valproate showed protection against manic recurrences, but not for depressive.
Considering the timing of maintenance treatment, our main results point toward a clear role of the early initiation of any stabilizers as a predictor of response to therapy through the reduction of future recurrences, as already indicated in other studies [14,23,24]. Indeed, introducing lithium therapy within the first five years of illness is more effective than introducing it later. Referring to the recently proposed staging models for Bipolar Disorder [25,11], we suggest considering the time of initiation of the maintenance therapy as an additional parameter for staging bipolar patients adequately. More specifically, patients who received stabilizing therapy later should be included in more advanced stages, with crucial consequences in the choice of such treatment. According to the staging models, each stage comes with a progressive complexity of treatment strategies: a patient who has been without mood stabilizers for a longer period might benefit from lithium, possibly in combination with other anticonvulsants or antipsychotics [26].
Not only the total number of episodes and their frequency should be considered as prognostic factors in BD, but it is also important to address the presence of peculiar clinical features within the episodes. We observed that the presence of psychotic features during BD is a negative prognostic factor in the response to stabilizing therapy. Previous studies have already reported that more than a half of BD patients exhibit at least one psychotic episode in their lifetime [27]; it is also known that the psychotic features are observed more frequently during manic episodes, approximately in 20-50% of cases [28]. The negative prognostic impact of psychotic features has been long known. Those patients who experienced delusions or hallucinations have a worse long-term social functioning and a lower probability to achieve complete remission from the disease [29,30]. A more recent study has shown that among bipolar patients treated with lithium; those with psychotic episodes have a worse outcome with preventive therapy [31]. Consistent with previous studies, we found that the presence of psychotic features during the disease turns out to be a negative prognostic factor in the response to preventive therapy.
Some limitations should be acknowledged in our study. First, using a retrospective design, data collection of anamnestic information is not always accurate as it is based on the patients’ subjective recollection of the events. We found particularly arduous to collect the previous pharmacological history. Furthermore, the sample itself included subjects with numerous hospitalizations, both in our hospital or other clinics, representing a population with more severe clinical features and multiple pharmacological trials.
CONCLUSION
Our study confirms the importance of early pharmacological interventions in BD: the sooner the patients start stabilizing therapy, the better is for response to treatment. Particularly, initiating lithium within the first five years of illness is more effective than delivering the treatment later in the disorder.
Consequently, according to our analysis, we propose to address the time of initiation of the maintenance therapy as a new potential marker of BD progression, to enrich the staging models already proposed by [25,11]. Specifically, patients with earlier initiation of maintenance treatment should be categorized within the early stages, while patients who initiated it later should be identified in the later stages. A staging model for BD can be widely applied, making it quite useful in determining with acceptable accuracy BD prognosis and in identifying useful and specific preventive treatments for each stage.
- Murray CJ, Lopez AD (1997) Global mortality, disability and the contribution of risk factors: Global burden of disease study. Lancet 349: 1436-1442.
- Kapczinski F, Vieta E, Andreazza AC, Frey BN, Gomes FA, et al. (2008) Allostatic load in bipolar disorder: implications for pathophysiology and treatment. Neurosci Biobehav Rev 32: 675-692.
- Kessing LV, Mortensen PB, Bowling TG (1998) Clinical definition of sensitisation in affective disorder: A case registers study of prevalence and prediction. J Affect Disord 47: 31-39.
- Kessing LV, Hansen MG, Andersen PK & Angst J (2004) The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders - a life-long perspective. Acta Psychiatr Scand 109: 339-344.
- Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, et al. (2004) Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry 65: 1106-1113.
- Tohen M, Greenfield SF, Weiss RD, Zarate CA Jr, Vagge LM, et al. (1998) The effect of comorbid substance use disorders on the course of bipolar disorder: A review. Harv Rev Psychiatry 6: 133-141.
- Mantere O, Melartin TK, Suominen K, Rytsälä HJ, Valtonen HM, et al. (2006) Differences in Axis I and II comorbidity between bipolar I and II disorders and major depressive disorder. J Clin Psychiatry 67: 584-593.
- Gonda X, Pompili M, Serafini G, Montebovi F, Campi S, et al. (2012) Suicidal behavior in bipolar disorder: Epidemiology, characteristics and major risk factors. J Affect Disord 143: 16-26.
- Berk M, Brnabic A, Dodd S, Kelin K, Tohen M, et al. (2011) Does stage of illness impact treatment response in bipolar disorder? Empirical treatment data and their implication for the staging model and early intervention. Bipolar Disord 13: 87-98.
- Post RM (1992) Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 149: 999-1010.
- Kapczinski F, Dias VV, Anna MKS, Frey BN, Oliveira RG, et al. (2009) Clinical implications of a staging model for bipolar disorders. Expert Rev Neurother 9: 957-966.
- Vieira RM, Manji HK, Zarate Jr CA (2009) The role of lithium in the treatment of bipolar disorder: convergent evidence for neurotrophic effects as a unifying hypothesis. Bipolar Disord 11 Suppl 2: 92-109.
- Gitlin M, Frye MA (2012) Maintenance therapies in bipolar disorders. Bipolar Disord 14 Suppl 2: 51-65.
- Franchini L, Zanardi R, Smeraldi E, Gasperini M (1999) Early onset of lithium prophylaxis as a predictor of good long-term outcome. Eur Arch Psychiatry Clin Neurosci 249: 227-230.
- Ketter TA, Houston JP, Adams DH, Risser RC, Meyers AL, et al. (2006) Differential efficacy of olanzapine and lithium in preventing manic or mixed recurrence in patients with bipolar I disorder based on number of previous manic or mixed episodes. J Clin Psychiatry 67: 95-101.
- Baethge C, Smolka MN, Gruschka P, Berghöfer A, Schlattmann P, et al. (2003) Does prophylaxis-delay in bipolar disorder influence outcome? Results from a long-term study of 147 patients. Acta Psychiatr Scand 107: 260-267.
- Baldessarini RJ, Tondo L, Hennen J (2003) Treatment-latency and previous episodes: Relationships to pretreatment morbidity and response to maintenance treatment in bipolar I and II disorders. Bipolar Disord 5: 169-179.
- Denicoff KD, Leverich GS, Nolen WA, Rush AJ, McElroy SL, et al. (2000) Validation of the Prospective NIMH-Life-Chart Method (NIMH-LCM-p) for Longitudinal Assessment of Bipolar Illness. Psychol Med 30: 1391-1397.
- Garnham J, Munro A, Slaney C, Macdougall M, Passmore M, et al. (2007) Prophylactic treatment response in bipolar disorder: Results of a naturalistic observation study. J Affect Disord 104: 185-190.
- Bauer MS, Mitchner L (2004) What is a mood stabilizer? An evidence-based response. Am J Psychiatry. 161: 3-18.
- Ketter TA, Calabrese JR (2002) Stabilization of mood from below versus above baseline in bipolar disorder: A new nomenclature. J Clin Psychiatry 63: 146-151.
- Calabrese JR, Shelton MD, Rapport DJ, Youngstrom EA, Jackson K, et al. (2005) A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry 162: 2152-2161.
- Post RM, Leverich GS, Altshuler LL, Frye MA, Suppes TM, et al. (2003) An overview of recent findings of the stanley foundation bipolar network (Part I). Bipolar Disord 5: 310-319.
- Rohayem J, Baylé JF, Richa S (2008) Predictors of prophylactic response to lithium. Encephale 34: 394-399.
- Berk M, Hallam KT, McGorry PD (2007) The potential utility of a staging model as a course specifier: A bipolar disorder perspective. J Affect Disord 100: 279-281.
- Lin D, Mok H, Yatham LN (2006) Polytherapy in bipolar disorder. CNS Drugs 20: 29-42.
- Keck Jr PE, McElroy SL, Havens JR, Altshuler LL, Nolen WA, et al. (2003) Psychosis in bipolar disorder: Phenomenology and impact on morbidity and course of illness. Compr Psychiatry 44: 263-269.
- Pope Jr H, Lipinski Jr J (1978) Diagnosis in schizophrenia and manic-depressive illness: A reassessment of the specificity of “schizophrenic“ symptoms in the light of current research. Arch Gen Psychiatry 35: 811-828.
- Rosen LN, Rosenthal NE, Dunner DL (1983) Social outcome compared in psychotic and nonpsychotic bipolar I patients. J Nerv Ment Dis 171: 272-275.
- Ozyildirim I, Cakir S, Yazici O (2010) Impact of psychotic features on morbidity and course of illness in patients with bipolar disorder. Eur Psychiatry 25: 47-51.
- Rohayem J, Baylé JF, Richa S (2008) Predictors of prophylactic response to lithium. Encephale 34: 394-399.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)


