Review Article
Fragment Reattachment in Traumatized Permanent Teeth: A Mini-Review
5860
Views & Citations4860
Likes & Shares
Fragment reattachment is a viable alternative, to composite restoration, for restoration of a traumatized permanent tooth when the fragment is available. The development of various techniques for maintaining pulp vitality and advanced adhesive systems ensure a successful outcome. However, the success of this procedure depends on the accurate diagnosis and clinical decision-making of the dentist. This mini review provides an overview of the various factors that influence the outcome of fragment reattachment and will assist, the dentist, in the decision-making process.
Keywords: Fragment reattachment, Core outcome set, Rehydration, Traumatic injuries
ABBREVIATIONS
TDI: Traumatic Dental Injuries; IADT: International Association of Dental Traumatology; COS: Core Outcome Set; CBCT: Cone-Beam Computed Tomography; Ca (OH)2: Calcium Hydroxide
Traumatic dental injuries (TDI) may lead to fractures and/or displacement of the involved teeth. This can often lead to secondary periapical infections, lesions etc. and can also be detrimental to the complete development of immature teeth. The teeth most frequently involved in a traumatic injury to the maxillofacial region are the permanent maxillary central incisors owing to their location in the arch. This often has a highly unaesthetic appearance and can have a long-term negative psychological effect for the individual [1]. Thus, the onus is on the dentist to not only restore the form, optimum function of the involved tooth/ teeth but also the aesthetic appearance of the tooth, in particular, and face, in general.
Fragment reattachment was first described by Chosack and Eidelman [2] back in 1964 and has since been favored by dental practitioners due to its advantages over other immediate restorative and aesthetic procedures. The introduction of major advances to aesthetic and restorative dentistry, and the materials used for the same, have improved the outcomes of the technique since its conception. One of the important milestones has been the introduction of acid etching to the technique by Tennery [3] which significantly increased the longevity when used with a compatible adhesive restorative system and the occasional use of preparation when indicated [4,5].
Fragment reattachment has tremendous advantages over other procedures such as it is quick, aesthetic and the patient suffer minimal psychological and social trauma, also it is highly economical. Although more advantageous, the limited literature on fragment reattachment has suggested that it may not be an effective permanent restoration since a good amount of data suggests that the teeth have refractured post attachment [5].
IMPORTANCE OF CASE HISTORY & ACCURATE DIAGNOSIS
Fragment reattachment cannot be evaluated as a separate entity without determining when, where and how of the underlying traumatic injury [1]. The extent of the injury, tissues involved, time elapsed since the injury are the factors that determine the choice of management techniques and the treatment outcome. Thus, a detailed case history and an accurate diagnosis of the underlying injury are of utmost importance [6].
A detailed case history outlying the time elapsed since the injury, place where the trauma occurred, adverse events in the immediate post-injury time period and how the injury was managed before seeking medical and/or dental attention should be elicited from the patient and documented. These factors are suggestive of the extent of the trauma and prognosis. A thorough extra- and intra-oral examination to ascertain the extent of injury, tissues involved, presence of dentoalveolar fractures should follow the case history [1,6,7]. Wang et al reported that the degree of trauma (presence or absence of luxation and luxation type) and the stage of root development are key risk factors in the development of pulp necrosis in teeth with uncomplicated crown fractures. In crown-fractured teeth with luxation, most pulp necrosis occurred within 12 months of initial trauma [8]. Hence, type of dental trauma, presence of luxation injury was some of the factors associated with adverse outcomes in permanent teeth after dental trauma [8,9]. These findings are important points to consider while formulating the strategy for treating and monitoring pulp health after dental trauma and overall outcome of therapy [1,8].
In cases where the fragment is not reported by the patient the examination of the oral wounds may be helpful in locating the missing fragment and, in very rare cases, radiographs of the soft tissue may also be indicated to rule out any fragments or foreign debris in the soft tissue wounds [1].
The tooth involved should be evaluated for tenderness on percussion or any signs of mobility [1]. Pulp sensibility testing is to be done for the part of the tooth remaining in the oral cavity irrespective of apparent pulpal involvement, however, the response may be erroneous and is not the true representative for pulp vitality. It should be repeated at the follow-up visits and all the results must be recorded for a comparison since the pulp tends to experience a transient loss of sensitivity due to a shock following the trauma. Hence any decisions regarding endodontic treatment, based on the sensibility testing, are ill-advised, in the first visit, and should be deferred till the next appointment. If the vitality of the tooth involved is in question pulse oximetry, laser and ultrasound Doppler flowmetry tests have been shown to produce accurate results for the same [1,7].
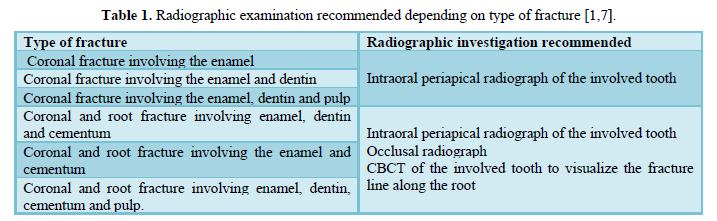
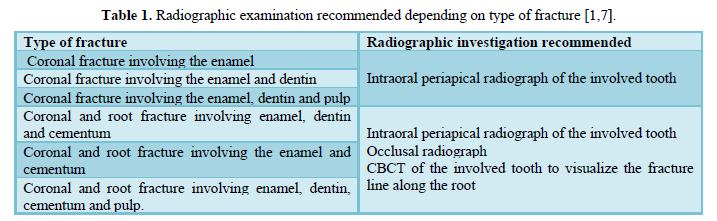
The radiographic evaluation of the traumatic injury depends on the type of fracture as shown in Table 1. In case of a fractured tooth where an intraoral periapical radiograph is indicated it is advised that if the fracture line is not clearly visualized in the radiograph involving the fractured tooth different angulations can be tried and the adjacent teeth should also be involved to rule out any trauma or injury that may have occurred to them. In all types of injury, it is also advisable to shoot a radiograph of the teeth in contact with the involved tooth/ teeth in the opposing arch to rule out any injury to the opposing tooth. An occlusal radiograph of the entire arch is recommended to rule out any dento-alveolar fractures. It should be kept in mind that these are recommendations only and the requirement and type of radiographs may vary from patient to patient as per need [1,7].
PROGNOSIS
Olsburgh and associates reported that the dentist plays a vital role in the prognosis of the traumatized tooth. The prognosis depends on his accurate diagnosis and treatment procedures at two different levels: the pulp level and the restoration level. They reviewed several techniques of fragment reattachment in complicated and uncomplicated traumatic injuries and found that the prognosis, at restoration level, depends on the dentin-bonding agents. At the pulpal level, the dentin-sealing prior to dentin-bonding affects the pulp vitality and, thereby, the overall prognosis of treatment [10].
TREATMENT APPROACHES
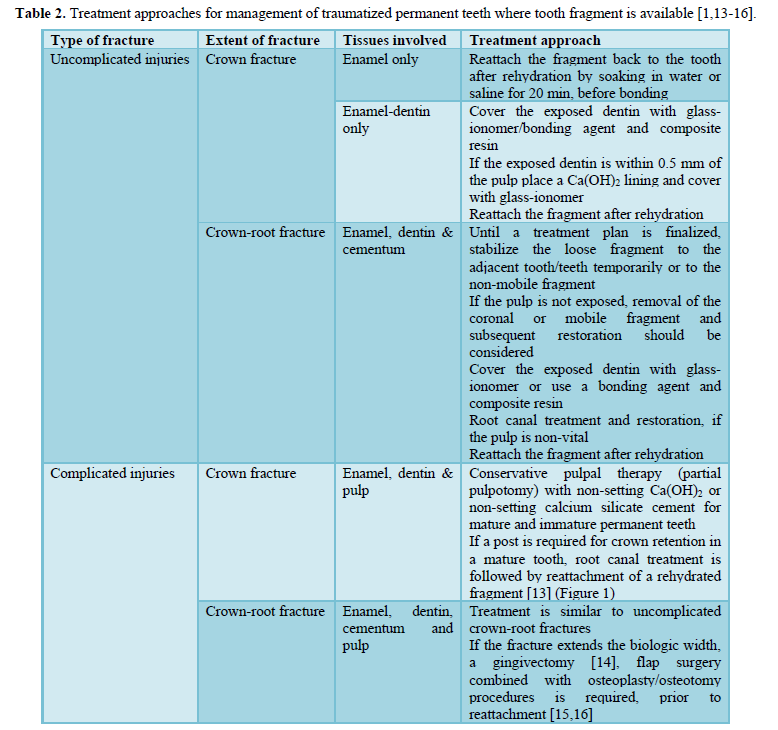
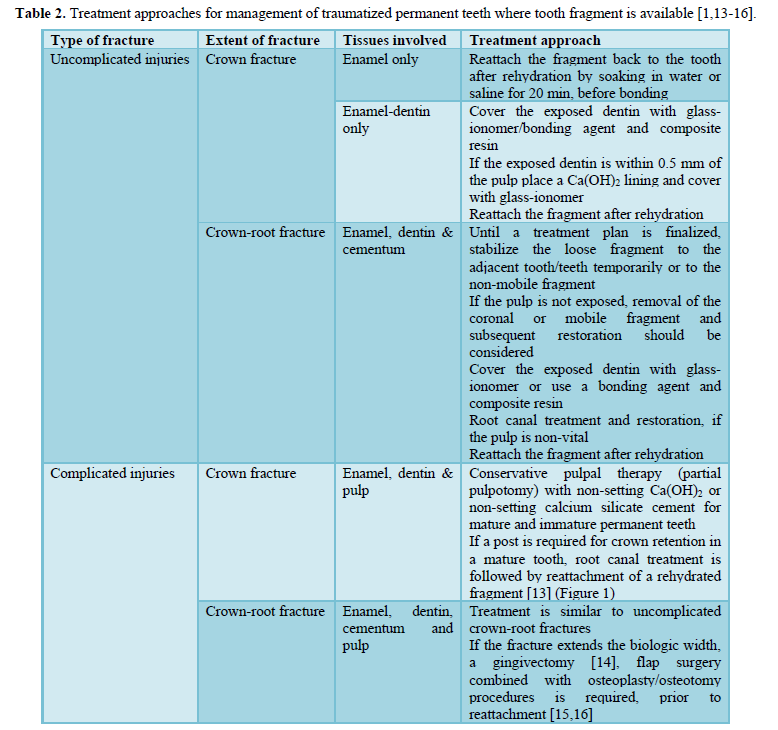
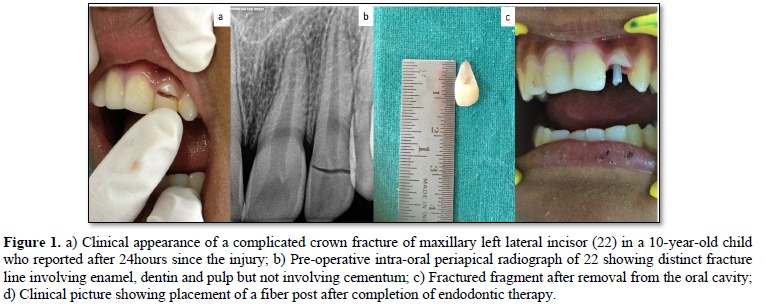
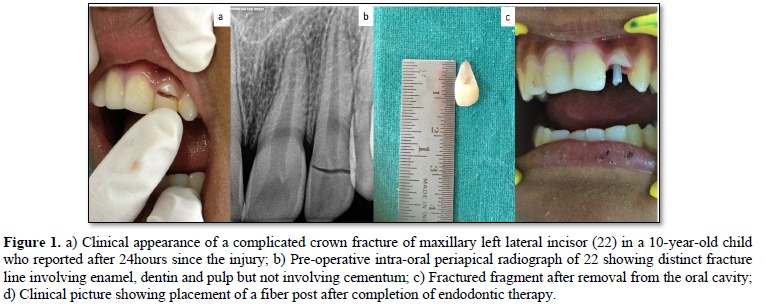
Several treatment options have been suggested depending on the type of injury sustained. In a questionnaire survey of restorative dentistry specialists, de Santos et al found that the interviewees struggled with treatment planning for crown- and crown-root fractures. Complicated and uncomplicated crown-root fractures posed greater difficulties due to the multi-disciplinary approach necessary for their management [11]. Hence, an evidence-based, uniform intervention strategy is necessary [12]. Thus, the International Association of Dental Traumatology (IADT), in 2020, suggested updated guidelines for improved management of injured teeth and to minimize complications resulting from trauma. These guidelines have been summarized in Table 2. Furthermore, current evidence shows that short-term, passive, and flexible splints for splinting luxated, avulsed, and root-fractured teeth is recommended. However, the duration of the said splinting depends on the type of injury (Figure 1) [1].
FOLLOW-UP
Any traumatized tooth/teeth should be followed up as per the IADT 2020 guidelines at 1 week, 6-8 weeks, 3 months, 6 months, 1 year and yearly for 5 years according to the type of injury. Follow up of the patient, whenever possible, should always be accompanied with radiographs annually for the first two years and then biennially until the 5 year follow up is completed. Photographic documentation should be maintained at each of the follow-ups for aesthetic re-evaluation [1].
TREATMENT OUTCOMES
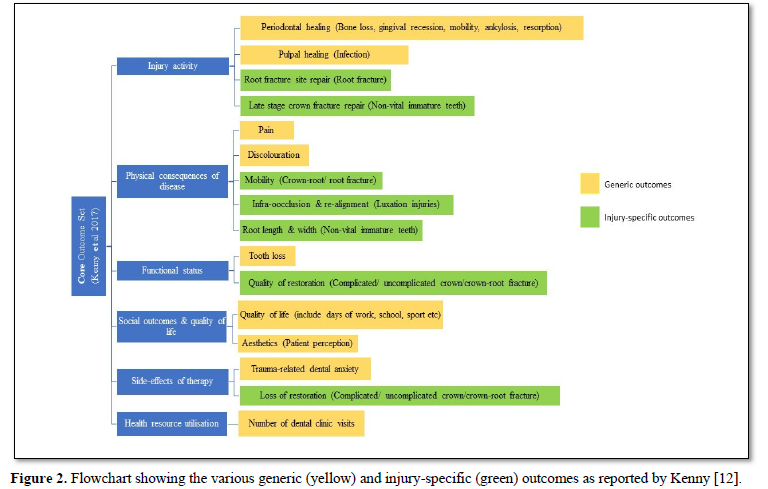
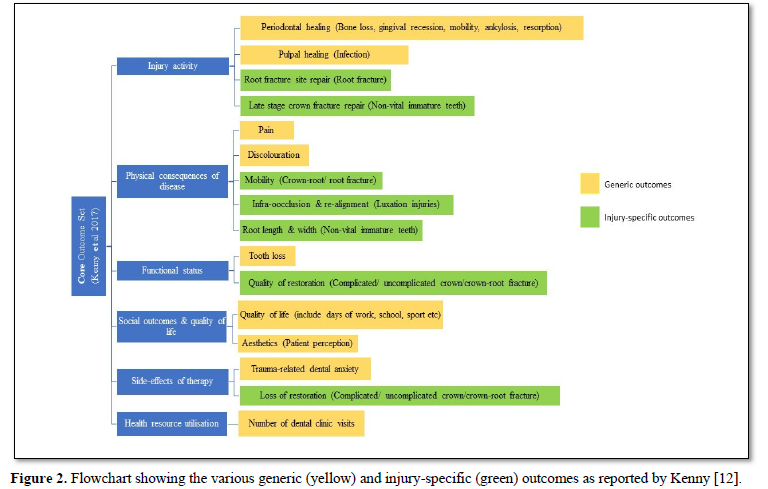
An outcome is a clinical measure used to adjudge the efficacy of treatment. Thus, outcomes need to be relevant to patients, clinicians and policymakers to provide best clinical treatment and conduct evidence-based research [12]. Almost
half of the patients evaluated in a 15-year questionnaire follow-up were dissatisfied with the color and/or anatomic form of their restored teeth [17]. Sharif and colleagues reported that clinical trials for treatment interventions in traumatic dental injuries poorly represented patient-related outcomes, with no outcomes reported for quality of life or family outcomes [18]. Thus, a Core Outcome Set (COS) for traumatic injuries was developed by Kenny et al by Delphi methodology. This COS outlines the outcomes as “generic” and/or injury-specific under several domains as given in Figure 2 [12].
FACTORS AFFECTING OUTCOMES
As stated previously, the overall outcome of fragment reattachment procedure, depends on the accurate management of pulp vitality and restorative success [10]. Any factor that affects one or both these components will have a detrimental effect on the injury specific as well as generic outcomes [12]. These factors are as follows:
- Time elapsed/ Treatment delay: Andreasen et al pooled the results of several studies about treatment delay on pulpal and periodontal healing of various types of TDIs and concluded that the treatment delay could be categorized into: Acute (24 h). In uncomplicated crown- or crown-root fractures, a subacute or delayed treatment is acceptable. However, in complicated fractures, a vital pulp therapy must be initiated within the first 24 h to prevent failure of treatment. The time elapsed is imperative not with respect to repositioning and splinting of the tooth/teeth but with the prevention of soft tissue infection [19]. A retrospective evaluation of uncomplicated crown fractures showed that the rate of pulpal necrosis increased with delayed treatment. Furthermore, the rate of pulpal necrosis is greater when the root formation is complete [8]. This is in sharp contrast to the findings of Rozi et al, who found no significant statistical difference between the time elapsed since dental injury and the initiation of dental treatment, although the difference may be attributed to the small sample size of the study. They further stated that the placement of dentin coverage, during the emergency visit, prevents bacterial invasion of deeper tissues [9] although Andreasen et al contradict this belief since the rate and extent of bacterial invasion are unknown, and the process is usually strain specific [20].
Treatment delay would also lead to longer dry time of the fractured fragment. The final bond strength of the restored tooth is drastically less when the fragment is dehydrated (up to 48 h) as compared to a hydrated fragment. Some of this diminished bond strength is returned when the fragment is rehydrated before reattachment or if the dentin is removed from the fragment before restoration [21].
- Type of injury: The one-year clinical survival rate of teeth restored with fragment reattachment in uncomplicated and complicated fractures were 95.7% and 90.0%, respectively [5]. The chances of future adverse outcomes are reported to be eight times higher in complicated crown fractures as compared to uncomplicated crown fractures [8]. The rate of loss of pulpal vitality increased manifold when the TDI was associated with a concomitant luxation injury, irrespective of stage of root development [8,9,17]. This was especially true in the case of intrusion injuries (90-91.3%) [8]. Crown fractures with associated luxation injuries resulted in adverse outcomes in 64% cases [9]. In 97% of uncomplicated crown fractures without luxation injuries, the pulp survived after 15 years, as against half of that in those with associated luxation injuries [17]. The difference here can be attributed to the loss of blood circulation and nerve supply to the periodontal tissues due to the luxation injuries [9]. However, there was no significant difference in the in vitro fracture resistance of a tooth restored by fragment reattachment based on the type of injury. The fracture resistance of restored tooth was significantly lower (~70%-84%) than non-traumatized tooth [5].
- Rehydration of fragment: Several techniques and time durations of rehydration have been suggested till date. Yilmaz et al studied the in vitro effects of wet and dry storage medium on the bond strengths and fracture resistance of the restored teeth and found that the difference to be insignificant. The fracture resistance forces of tooth fragments and remnants that were kept in a dry environment for 47 hours followed by 30 min in 0.9% saline were not significantly different from those for teeth that had been kept in tap water for 24 hours prior to their reattachment [5]. This is similar to the findings of Capp et al, who stated that strength of a hydrated (placed in distilled water) and rehydrated (fragment immersed in distilled water 30 min before the bonding) bonded fragments, were similar, although greater than dehydrated fragments [21,22]. Recently, rehydration by means of a 15 min humidification process was proven to be more effective than immersion in distilled water [23]. Another alternative is the use of Tooth Mousse, as a short-term storage media, for effective rehydration and improved bonding [24].
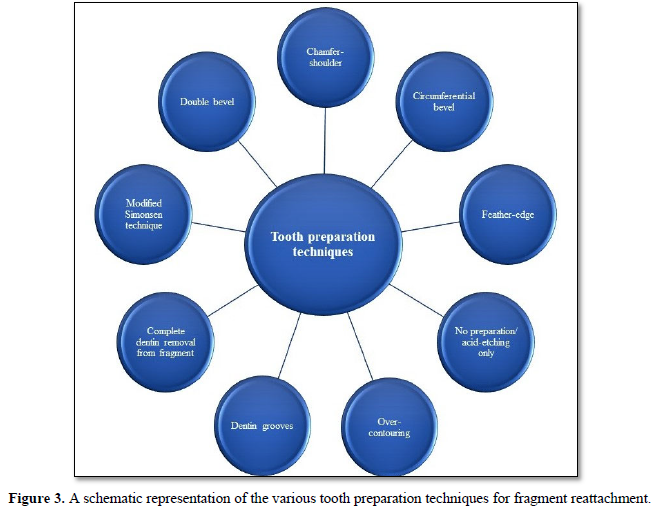
- Tooth preparation: Different approaches of preparing the fragment and the fractured tooth margins have been suggested [2,4,25-29] (Figure 3). Reis et al found that the highest fracture resistance was seen with pre-bonding beveling or dentin grooves and post-bonding over-contouring, which was comparable to non-traumatized tooth [26]. Similar results were noted with post-attachment beveling [27]. A comparison of post-bonding chamfer and pre-attachment complete dentin removal from the fragment showed that the dentin removal presents increased surface area, thus improving the fracture resistance. This is critical for delayed reattachment of a fragment stored in dry environment. However, there is no real consensus on the technique to be followed [28]. The pooled data of several studies showed that the bond strength of reattachment procedure is not dependent only on the technique but also influenced by the hydration of the fragment and the adhesive material used [29]. Thus, it is suggested that, as long as the fragment adapted well with the tooth surface, tooth preparation should be avoided and only adhesive-based reattachment, using an adhesive with good mechanical properties, is warranted although some preparation may be required depending on the type of fracture [28,29].
- Adhesive material: The bond strength of the restored tooth is highest when the type of fracture and technique to be used are considered before choosing the adhesive system to be used. The bond strength was higher when two-step adhesive system was combined with flowable composite resin, when fragment is reattached without preparation, as compared to micro-hybrid composite resin. However, if a post-bonding chamfer is to be prepared, with or without prior dentin removal, an adhesive system and micro-hybrid composite resin are preferred. A nano- or nanohybrid composite resin is the material of choice when bevel preparation or dentin grooves are recommended. Micro-hybrid composite is used when over-contouring or when internal grooves are prepared on the tooth surface [29].
CONCLUSION
The IADT guidelines (2020) state that fragment reattachment is a temporary restorative procedure with a longevity of 2-7years [1,30]. There are several factors that influence the survival of this procedure. However, there is lack of evidence in this regard. Thus, future studies assessing the influence of these factors and long-term follow-up are necessary.
-
Bourguignon C, Cohenca N, Lauridsen E, Flores MT, O'Connell AC, et al. (2020) International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent Traumatol 36: 314-330.
-
Chosack A, Eidelman E (1964) Rehabilitation of a fractured incisor using the patient’s natural crown: Case report. J Dent Child 71: 19-21.
-
Tennery NT (1988) The fractured tooth reunited using the acid bonding technique. Tex Dent J 96: 16-17.
-
Simonsen RJ (1982) Restoration of a fractured central incisor using original tooth fragment. J Am Dent Assoc 105: 646-648.
-
Yilmaz Y, Guler C, Sahin H, Eyuboglu O (2010) Evaluation of tooth-fragment reattachment: A clinical and laboratory study. Dent Traumatol 26(4): 308-314.
-
Andreasen JO, Andreasen FM (1993) Textbook and color atlas of traumatic injuries to the teeth, 3rd ed. Copenhagen: Munksgaard Publishers 1993.
-
Andreasen FM, Kahler B (2015) Diagnosis of acute dental trauma: The importance of standardized documentation: A review. Dental Traumatol 31: 340-349.
-
Wang C, Qin M, Guan Y (2014) Analysis of pulp prognosis in 603 permanent teeth with uncomplicated crown fracture with or without luxation. Dental Traumatol 30: 333-337.
-
Rozi AH, Scott JM, Seminario AL (2017) Trauma in permanent teeth: Factors associated with adverse outcomes in a University Pediatric Dental Clinic. J Dent Child 84(1): 9-15.
-
Olsburgh S, Jacoby T, Krejci I (2002) Crown fractures in the permanent dentition: Pulpal and restorative considerations. Dent Traumatol 18: 103-115.
-
de Castro MAM, Poi WR, de Castro JCM, Panzarini SR, Sonoda CK, et al. (2010) Crown and crown-root fractures: An evaluation of the treatment plans for management proposed by 154 specialists in restorative dentistry. Dental Traumatol 26: 236-242.
-
Kenny KP, Day PF, Sharif MO, Parashos P, Lauridsen E, et al. (2018) What are the important outcomes in traumatic dental injuries? An international approach to the development of a core outcome set. Dent Traumatol 34(1): 4-11.
-
Choudhary A, Garg R, Bhalla A, Khatri RK (2015) Tooth fragment reattachment: An esthetic, biological restoration. J Nat Sc Biol Med 6: 205-207.
-
Kothare SS, Choubey S, Das AR (2020) Fragment reattachment of an uncomplicated crown-root fracture: A case report. J South Asian Assoc Paediatr Dent 3(1): 30-33.
-
Ertugrul F, Eden E, Ilgenli T (2008) Multidisciplinary treatment of complicated sub gingivally fractured permanent central incisors: Two case reports Dent Traumatol 24: e61-e66.
-
Öz İA, Haytac¸ MC, Toroğlu MS (2006) Multidisciplinary approach to the rehabilitation of a crown-root fracture with original fragment for immediate esthetics: A case report with 4-year follow-up. Dent Traumatol 22: 48-52.
-
Robertson A (1998). A retrospective evaluation of patients with uncomplicated crown fractures and luxation injuries. Endod Dent Traumatol 14: 245-256.
-
Sharif MO, Tejani-Sharif A, Kenny K, Day PF (2015) A systematic review of outcome measures used in clinical trials of treatment interventions following traumatic dental injuries. Dent Traumatol 31: 422-428.
-
Andreasen JO, Andreasen FM, Skeie A, Hjørting-Hansen E, Schwartz O (2002) Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries: A review article. Dent Traumatol 18: 116-128.
-
Andreasen JO, Lauridsen E, Andreasen FM (2010) Contradictions in the treatment of traumatic dental injuries and ways to proceed in dental trauma research. Dent Traumatol 26: 16-22.
-
Capp CI, Roda MI, Tamaki R, Castanho GM, Camargo MA, et al. (2009) Reattachment of rehydrated dental fragment using two techniques. Dent Traumatol 25: 95-99.
-
Lauridsen E, Hermann NV, Gerds TA, Ahrensburg SS, Kreiborg S, et al. (2012) Combination injuries 3: The risk of pulp necrosis in permanent teeth with extrusion or lateral luxation and concomitant crown fractures without pulp exposure. Dent Traumatol 28(5): 379-385.
-
Madhubala A, Tewari N, Mathur VP, Bansal K (2019) Comparative evaluation of fracture resistance using two rehydration protocols for fragment reattachment in uncomplicated crown fractures. Dent Traumatol 35(3): 199-203.
-
Jalannavar P, Tavargeri A (2018) Influence of storage media and duration of fragment in the media on the bond strength of the reattached tooth fragment. Int J Clin Pediatr Dent 11(2): 83-88.
-
Ojeda-Gutierrez F, Martinez-Marquez B, Rosales-Ibanez R, Pozos-Guillen AJ (2011) Reattachment of anterior teeth fragments using a modified Simonsen’s technique after dental trauma: Report of a case. Dent Traumatol 27: 81-85.
-
Reis A, Francci C, Loguercio AD, Carrilho MR, Rodriques Filho LE (2001) Re-attachment of anterior fractured teeth: Fracture strength using different techniques. Oper Dent 26(3): 287-294.
-
Chazine M, Sedda M, Ounsi HF, Paragliola R, Ferrari M, et al. (2011) Evaluation of the fracture resistance of reattached incisal fragments using different materials and techniques. Dental Traumatol 27: 15-18.
-
Garcia FCP, Poubel DLN, Almeida JCF, Toledo IP, Poi WR, et al. (2018) Tooth fragment reattachment techniques: A systematic review. Dent Traumatol 38: 135-143.
-
de Sousa APBR, França K, Rezende LVML, Poubel DLN, Almeida JCF, et al. (2018) In vitro tooth reattachment techniques: A systematic review, Dent Traumatol 34: 297-310.
-
Ajayi DM, Adebayo GE (2018) Survival of reattached tooth: A systematic review. J West Afric Coll Surg 8: 59-84.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Advance Research on Alzheimers and Parkinsons Disease
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)






