Case Report
Management of Soft Tissue Esthetics around Anterior Single Immediate Implant Using TTPHIL® Technique and Implant Supracrestal Extensions in Provisional and Definitive Restorations: Case Report
5823
Views & Citations4823
Likes & Shares
Restoration in anterior maxillary zone poses an esthetic challenge due to demand for immediate prosthetic restoration and subsequent alveolar bone resorption and gingival recession. In order to deliver immediate esthetic results, modified surgical and prosthetic protocols are gaining popularity that reduces the number of operating sessions. In this clinical report missing anterior tooth was restored with immediate dental implant using TTPHIL® technique and optimum esthetic gingival contour was created using immediate provisional and definitive restorations along with submerged extensions. This technique allows for maintenance and enhancement of hard and soft tissue topography that provide predictable and reproducible esthetic outcome without any augmentation procedures.
Keywords: Immediate implantation; TTPHIL® technique; transitional prosthesis; Implant supracrestal tissues; Zirconia abutment
Abbreviation: TTPHIL®: Tall Tilted Pin Hole Placement Immediate Loading technique
INTRODUCTION
Replacing missing teeth in anterior maxilla poses utmost challenge to clinician due to associated high esthetic value and technique sensitive tissue manipulation [1]. Maintenance of alveolar crestal bone height in interproximal areas and height and thickness of facial bone wall are two important features that enhance esthetics by maintaining soft tissue contour [2]. TTPHIL® (Tall, Tilted, PinHole, Immediate Loading) technique have shown considerable success with immediate implantations and restorations [3]. The major advantage of this technique is that it provides soft tissue stability by creating a biologic seal around implant-abutment junction through flapless, subcrestal implant placement and use of microgrooved abutments. It preserves alveolar bone height and reduces marginal bone loss that occurs during socket healing [4]. Furthermore, selection of abutment material is considered very important for per implant soft tissue health as abutments on bone level implants come into contact with soft tissue. Also, immediate provisionalization of implant demonstrates positive effect on peri-implant soft tissue contour enhancing patient comfort and satisfaction [5].
This clinical report presents soft tissue management using TTPHIL® and customized temporary abutment and definitive zirconia abutment with the goal of delivering minimally invasive and esthetically pleasing outcome.
CASE REPORT
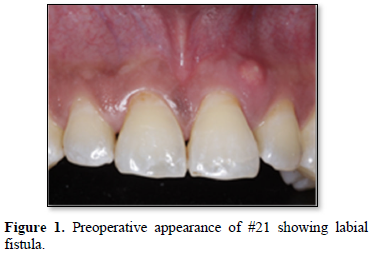
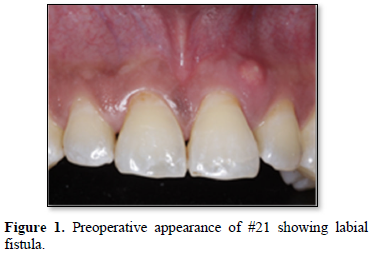
42-year-old male patient presented with chief complaint of pain and mobility in upper front tooth. He did not have any significant medical and habit history. He gave history of fall about 1 week back. On examination, #21
was found to be tender on palpation and mobile, pus draining sinus opening on labial gingival (Figure 1). The remaining teeth were sound. He was subjected to panoramic radiography (Genoray Papaya) and cone-beam computerized tomography scan (Care stream) that demonstrated root fracture (Figure 2). Considering the age of patient, it was prudent to provide fixed treatment with immediate function. Therefore, long cortical implant using TTPHIL® technique engaging nasal cortical bone to attain objectives of primary stability and ossification that form primary requisite for immediate function was planned. After obtaining signed consent for proposed treatment plan, oral prophylaxis was done. One hour prior to surgery, Amoxicillin 1g was given orally and was followed up with 500mg for 3times/daily for next 5 days. Atraumatic extraction was done with forceps. As per the socket classification by Tarnow et al, the residual socket was classified as class I socket [6]. Implant (Bioline I, BiolineDental GmbH&Co.KG) was placed freehand using TTPHIL® technique which is elucidated in following paragraph.
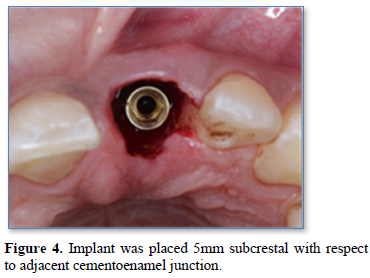
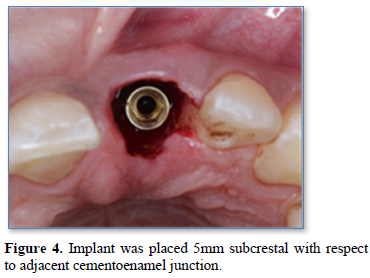
Lignocaine hydrochloride with adrenaline 1:200000 (Lignox 2%) was used. A 1.4mm diameter single drill was used to drill at low speed of 400-600rpm for proprioception of nasal cortex engagement in a flapless manner. Cone-beam computerized tomography scan (Carestream) was taking to confirm direction from buccal to palatal aspect (Figure 3). 3.5x18mm long implant with sharp tapered apex mounted on implant driver was driven into drilled course engaging nasal cortex and 5mm subcrestal placement measured from adjacent cementoenamel junction was achieved (Figure 4). 40Ncm torque and reverse torquing forces were obtained.
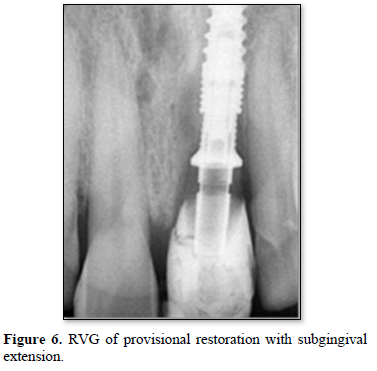
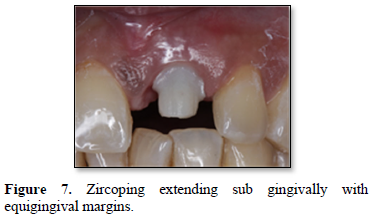
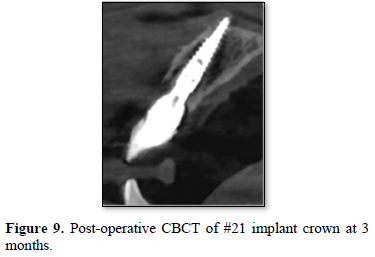
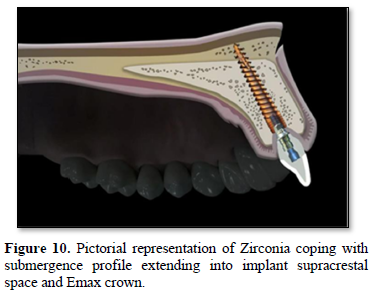
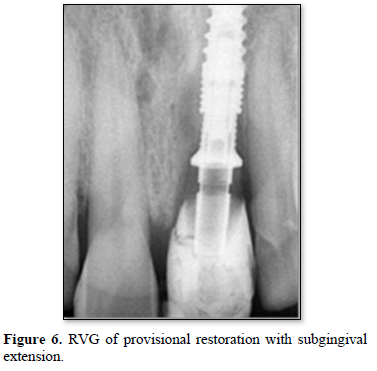
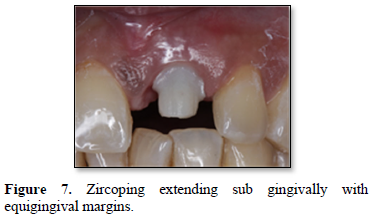
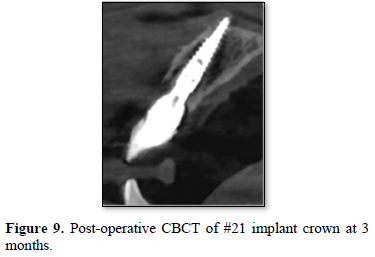
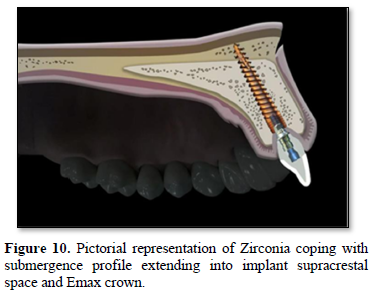
Implant level single stage putty and light body impression (GC Flexseed, GC Dental) was made using closed tray transfer copings. Implant analogue was fitted on transfer coping in completed impression and cast was poured using type-III dental stone (Microstone, Whip Mix Corp.) and sent to lab for zircoping fabrication on definitive abutments. For emergence profile, customized healing abutment was fabricated using composite material and screwed onto implant to prevent soft tissue collapse and maintain emergence profile (Figure 5). Transitional crown was made directly on screwed abutment using composite restorative material (Figure 6). The zircoping was fixed to microgrooved abutment on the cast using resin cement (Panavia F2.0, Kuraray) to avoid subgingival cement remnants and the complex was screwed in patient’s mouth on second day. Following fixation, margin on zircoping was modified to make it equigingival (Figure 7). An abutment level impression was made using putty and light body (GC Flexseed, GC Dental) for Emax crown fabrication. A second transitional crown was fabricated intraorally using composite material. The next day, glazed Emax crown was cemented onto zircoping to bring about required esthetic outcome (Figure 8). Definitive prosthesis that supports supracrestal tissues in its place was delivered in two days. A follow up of three months showed optimum soft tissue esthetics and maintenance of marginal bone levels (Figure 9). The entire implant-zircoping abutment-crown assembly has catered to the esthetic need of the patient (Figure 10).








DISCUSSION
Ideally, implant placement should be based on prosthetic-driven treatment plan to counter problem of marginal bone loss and subsequent soft tissue recession associated with immediately loaded implants [7]. In this case, benefits of immediate implantation using TTPHIL® technique and provisionalization concepts have been harnessed in optimizing esthetic success by preserving existing osseous and gingival architecture. The positioning is such that fixture engages adequate amount of native bone. Using tall implants through the length of available bone contributes to primary stability through ossification in nasal cortical bone which is a primary requisite for immediate functional loading [8]. It also minimizes micromovement and improves bone implant contact area for succeeding osseointegration [9]. The coronal portion of implant body maintained 2mm distance from buccal wall of socket, since coronal area of socket is the one mostly affected by remodeling changes that occur during healing period [10]. Subcrestal implant positioning also takes into account initial remodeling and crestal bone changes that occur in first year [1]. Degidi [11] found that no gaps or fibrous connective tissue were present at the interface of the subcrestal implants. Additionally, placing narrow implant helps to maintain papillary gingival height and reduce rate of vertical bone resorption on buccal plate [8,12]. Lastly, flapless technique preserves periosteum and supra-periostal plexus that aids in maintenance of alveolar bone [13]. At the abutment level, platform switching establishes space for maintaining peri-implant biologic width and minimizes chances of bacterial infiltration and consequent peri-implantitis [14]. Thus, possibility of crestal bone loss and subsequent gingival recession are reduced.
The transitional restoration comprises an anatomically shaped submergence profile, which applies lateral pressure to soft tissue, forcing gingival fibers to align in a circular orientation. This lateral pressure helps buccal tissue to maintain its vertical location. The alignment of fibers is in accordance with the study by Schierano [14] whose investigation around 9 retrieved abutments revealed horizontal and circular alignment of collagen fibers around abutments. As healing process progresses and inflammation diminishes, coronal soft tissue remains purposefully supported, supra-crestally, by transitional prosthesis in early stage and Zirconia abutment in the later stage to form a supra-crestal scaffold in healing socket [10]. Provisionalization also helps to maintain height of interproximal papilla [5]. Additionally, Zirconia abutment was recommended for anterior regions because of their greater esthetic properties [15]. Clinical data suggests that adhesion of fibroblasts to Zirconia abutment surface by increasing cellular growth rate reduce bacterial adherence leading to favorable soft tissue and marginal bone levels [15,16]. Using zirconia abutment, prosthesis margin was shifted to equigingival level that helps in easy access for removal of cement reducing the incidence of periimplantitis. These features explain the effectiveness of supra-crestal zirconia abutment extension in delivering emergence profile and maintaining soft tissue integrity.
CONCLUSION
The well-planned immediate implant placement using TTPHIL® technique and immediate provisionalization allowed for viable and predictable functional and esthetic outcomes. Placing customized abutment followed by zirconia abutment with submerged extensions aid in maintaining integrity of implant supra-crestal tissues that form key elements in delivery of long-term purposeful outcome. Nevertheless, use of this technique in all types of extraction sockets and long-term evaluation of soft and hard tissue integrity need to be assessed.
- Par-Olov O, Chu S, Drago C, Saito H, Myron N (2020) Clinical Outcomes of Maxillary Anterior Postextraction Socket Implants with Immediate Provisional Restorations Using a Novel Macro- Hybrid Implant Design: An 18- to 24-Month Single-Cohort Prospective Study. Int J Periodont Rest 40: 355-363.
- Henningsen A, Smeets R, Koppen K, Sehner S (2017) Immediate loading of subcrestally placed dental implants in anterior and premolar sites. J Craniomaxillofac Surg 45(11): 1898-1905.
- Nag PVR, Sarika P, Khan R, Bhagwatkar T (2018) Immediate implantation and loading in just two days with TTPHIL technique using CAD/CAM Prosthesis. Int J Appl Dent Sci pp: 209-213.
- Nag PVR, Sarika P, Khan R, Bhagwatkar T (2019) TTPHIL-ALL TILT™ - An effective technique for loading of dental implants: A comparative study of stress distribution in maxilla using finite element analysis. J Dent Implant 9: 4-11.
- Chul KO, Jeongwon P, Kim JH (2019) Esthetic Rehabilitation of Maxillary Anterior Teeth, Including an Immediate Provisionalization with an Implant-Supported Fixed Dental Prosthesis. J Clin Med 8: 428.
- Tarnow DP, Chu SJ (2020) The Single Tooth Implant a Minimally invasive Approach for Anterior and posterior sockets. Quintessence Publishing: Batavia; pp: 13-14.
- Funato A, Salama MA, Ishikawa T, Garber DA, Salama H (2007) Timing, positioning, and sequential staging in esthetic implant therapy: A four-dimensional perspective. Int J Periodont Rest 27: 313e23.
- Degidi M, Piattelli A, Scarano A, Shibli J, Iezzi G (2012) Peri-Implant Collagen Fibers Around Human Cone Morse Connection Implants Under Polarized Light: A Report of Three Cases. Int J Periodont Rest 32: 323-328.
- Han CH, Mangano F, Mortellaro C, Park KB (2016) Immediate Loading of Tapered Implants Placed in Postextraction Sockets and Healed Sites. J Craniofac Surg 27(5): 1220-1227.
- Valavanis KD, Vergoullis I, Papastamos M, Salama H (2020) Immediate Implant Placement and Provisionalization in the Esthetic Zone Revisited: The Marginal Migration Concept (MMC). Appl Sci 10: 8944.
- Degidi M, Scarano A, Iezzi G, Piattelli A (2005) Histologic Analysis of an Immediately Loaded Implant Retrieved After 2 Months. J Oral Implantol 31(5): 247-254.
- Garzón N, Velasco-Ortega E, Lopez LJ (2019) Bone Loss in Implants Placed at Subcrestal and Crestal Level: A Systematic Review and Meta-Analysis. Materials 12: 154.
- Martınez CP, Vlahovic Z, Scepanovic M, Videnovic G, Barone A, et al. (2015) Submerged flapless technique vs. Conventional flap approach for implant placement: Experimental domestic pig study with 12-month follow-up. Clin Oral Impl Res pp: 1-5.
- Valles C, Rodriguez-Ciurana X, Clementini M, Baglivo M, Paniagua B, et al. (2018) Influence of subcrestal implant placement compared with equicrestal position on the peri-implant hard and soft tissues around platform-switched implants: A systematic review and meta-analysis. Clin Oral Investig 22(2): 555-570.
- Medeiros R, Filho AJV, Pellizzer EP, Mazaro JVQ, Santos DM, et al. (2013) Analysis of the Peri-implant Soft Tissues in Contact with Zirconia Abutments: An Evidence-based Literature Review. J Contemp Dent Prac 14: 567-572.
- Raffaelli L, Iommetti PR, Piccioni E, Toesca A, Serini S, et al. (2008) Growth, viability, adhesion potential, and fibronectin expression in fibroblasts cultured on zirconia or felspathic ceramics in vitro. J Biomed Mater Res 86(4): 959-968.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Chemotherapy Research Journal (ISSN:2642-0236)













