Case Report
Effects of Maxillary Arch Expansion: A Systematic Review of Systematic Reviews
6213
Views & Citations5213
Likes & Shares
Purpose: The aim of this overview was to summarize the available systematic reviews (SRs) and meta-analyses (MAs) reporting the effects of maxillary expansion (ME).
Material and Methods: 5 databases were electronically searched up to May 2019. The outcomes of interest were the craniofacial effect of ME; the effect of ME on the transverse dimension of the maxillary and the mandibular arches, the mid-palatal suture, the facial soft tissue, the anteroposterior and vertical jaws relationship and the adjacent sutures, the retention period after ME, the root resorption and periodontal problems associated with ME. The quality of the included reviews was assessed using AMSTAR, LRD tool and according to a pre-determined level of evidence.
Results: The initial search yielded 4390 studies and 25 SRs/MAs were included finally. The quality of evidence was high in 4 reviews, while the rest of the reviews ranged from low to moderate.
Conclusions: High quality evidence supported the dento-alveolar effects of slow and rapid ME in growing patients, whereas the amount of skeletal expansion gained was debatable. There was also spontaneous mild increase in the mandibular arch width and the negligible soft tissue changes due to ME. Moderate quality evidence reported negligible vertical changes occurring following RME.
Keywords: Maxillary expansion, Slow maxillary expansion, Rapid maxillary expansion, Implant-supported maxillary expansion, Bone-supported maxillary expansion, Overview, Systematic review
Abbreviations: SR: Systematic Reviews; MA: Meta-Analyses; ME: Maxillary Expansion; RME: Rapid Maxillary Expansion; SME: Slow Maxillary Expansion; SRME: Semi Rapid Maxillary Expansion; MPS: Mid-Palatal Suture; LRD: Level of Research Design Scoring; LQE: Low Quality Evidence; MQE: Moderate Quality Evidence; HQE: High Quality Evidence; RCT: Randomized Controlled Trials; CBCT: Cone Beam Computed Tomography; QDH: Quad Helix; EP: Expansion Plates
INTRODUCTION
Transverse maxillary deficiency or posterior crossbite is clinically identified when the lower teeth occlude in a buccal position relative to the upper teeth [1]. Posterior crossbites could be of skeletal or dental origins [2]. Be it of any type, posterior crossbite is not self-corrected and should be treated once diagnosed to allow optimum coordination of the maxillary and mandibular dental arches, prevent functional shifts and wear of the permanent teeth, prevent dentofacial asymmetry and temporomandibular joint disorder [3,4]. Consequently, maxillary expansion (ME) has gained much popularity in the orthodontic community and became an integral part of many orthodontic treatments [5].
However, upon reviewing the orthodontic literature, one can find various proposed maxillary expanders and expansion protocols [6], yet there is no consensus regarding which appliance design or activation rate benefits our patients the most. ME rate can be rapid, so-called rapid maxillary expansion (RME), with an expansion rate of 0.5 mm per day, or slow, so-called slow maxillary expansion (SME), with an expansion rate of 0.25-0.5 mm per week [7]. A clear outcome and thereby specific indications for each expansion rate could not be established, where both RME & SME are reported to increase the skeletal transversal width, but delineated to be lower than the dento-alveolar expansion attained [8].
Additionally, the ideal age for ME is still debatable. Although it is recommended to treat transverse deficiencies relatively early up to the skeletal growth spurt [9], the mid-palatal suture (MPS) fusion is poorly correlated with patient age and gender [10], rendering clear cut indications for surgically assisted ME indefinite.
ME effects surpassed the maxilla to include most adjacent structures [11,12]. The maxillo-mandibular intimate articulation empowered ME not only to increase the transverse palatal dimension, but also to influence the sagittal and vertical facial proportions [13], the mandible with its temporomandibular articulatory system [14], the airway spaces [15] and more. Moreover, the advent of bone anchored ME [16] and the recent modalities detecting MPS maturation [10], have expanded the patients age range that can be treated successfully using the basic ME protocols.
In attempt to summarize the massive amount of evolving data, systematic reviews (SRs) and meta-analyses (MAs) are acknowledged [17]. Not surprisingly, the number of SRs exploring the effects of ME has rapidly escalated. However, their validity is influenced by the methodology [18]. Aiming to recapitulate and critically appraise the best available evidence for both clinicians and researchers, we performed a SR of the published SRs/MAs to provide an overview of all reported ME craniofacial effects [19].
OBJECTIVES
The aims of the current overview were to: (i) Summarize the reported outcomes of ME dentoalveolar and craniofacial treatment effects, (ii) Evaluate the methodological quality of the SRs/MAs, and (iii) Provide a clinical guideline for orthodontists regarding ME protocols, expansion appliances and the suitable age range for ME treatment based on the best available evidence.
METHODS
Protocol registration
This overview followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [20]. The review protocol was registered at PROSPERO (International prospective register of systematic reviews) with registration number: CRD42018103702.
Eligibility criteria
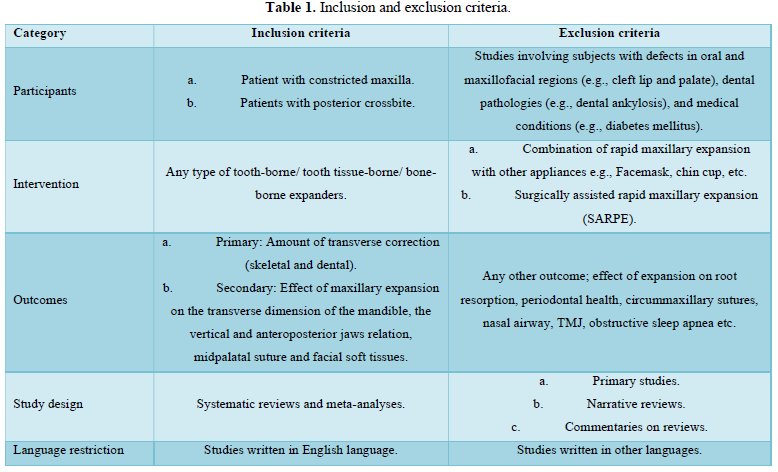
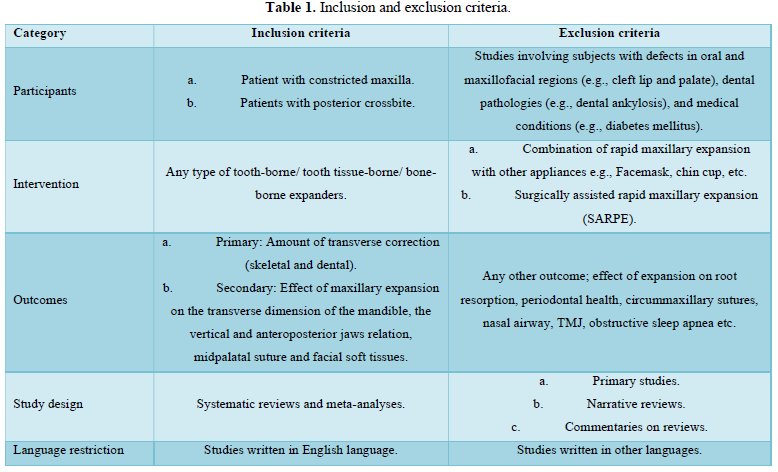
The inclusion and exclusion criteria of the reviews are mentioned in (Table 1).
Search strategy, Study selection and Data collection
Five databases (PubMed, Cochrane library central, LILACS, ScienceDirect and Web of Science) were electronically searched up to May 2019 using the search strategy “(Maxillary transverse discrepancy OR upper dental arch constriction OR unilateral posterior crossbite OR bilateral posterior crossbite OR maxillary constriction OR narrow maxilla OR orthodontic patients OR retroclined molars OR cross-bite) And (Rapid maxillary expansion OR rapid palatal expansion OR maxillary disjunction OR palatal disjunction OR Palatal Expansion OR RME OR SME OR RPE OR Hyrax OR quad helix OR Haas expander Or jack Screw OR surgically assisted palatal expansion OR surgically facilitated palatal expansion OR SARPE OR surgically assisted rapid palatal expansion OR surgically assisted maxillary expansion OR corticotomy)”.
Hand-search of the European Journal of Orthodontics, American Journal of Orthodontics and Dentofacial Orthopedics, Orthodontics and Craniofacial Research and The Angle Orthodontist was also performed. Electronic search of the grey literature at ProQuest and PROSPERO was performed, in addition to searching the conference abstracts of scientific congresses (European Orthodontic Society and International Association of Dental Research).
Following exclusion of the internal and external duplicates, all resulting titles then abstracts were scanned, and the reviews that seemed to fulfil the eligibility criteria were read in full-text. SRs/MAs which satisfied all the eligibility criteria were included. The reference lists of the included SRs/ MAs were also investigated. The search and study selection were independently accomplished by two reviewers (A.A. and M.A.). In case of any disagreements, the third reviewer (Y.M.) was consulted for a conclusive decision.
Data items and collection
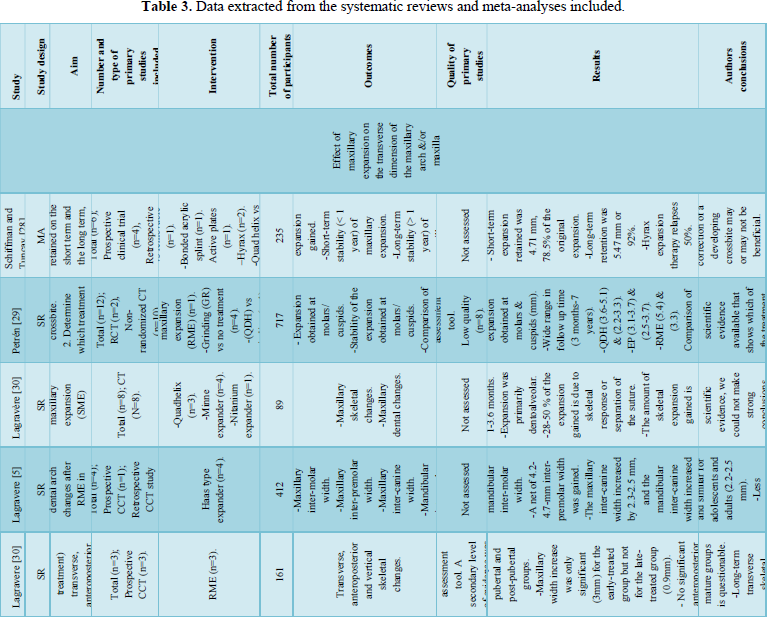
Data about Authors, Year of publication, Study design, Intervention, Total number of subjects, Outcome, Quality of the primary studies, Results, and Author’s conclusions were extracted from the included SRs/MAs.
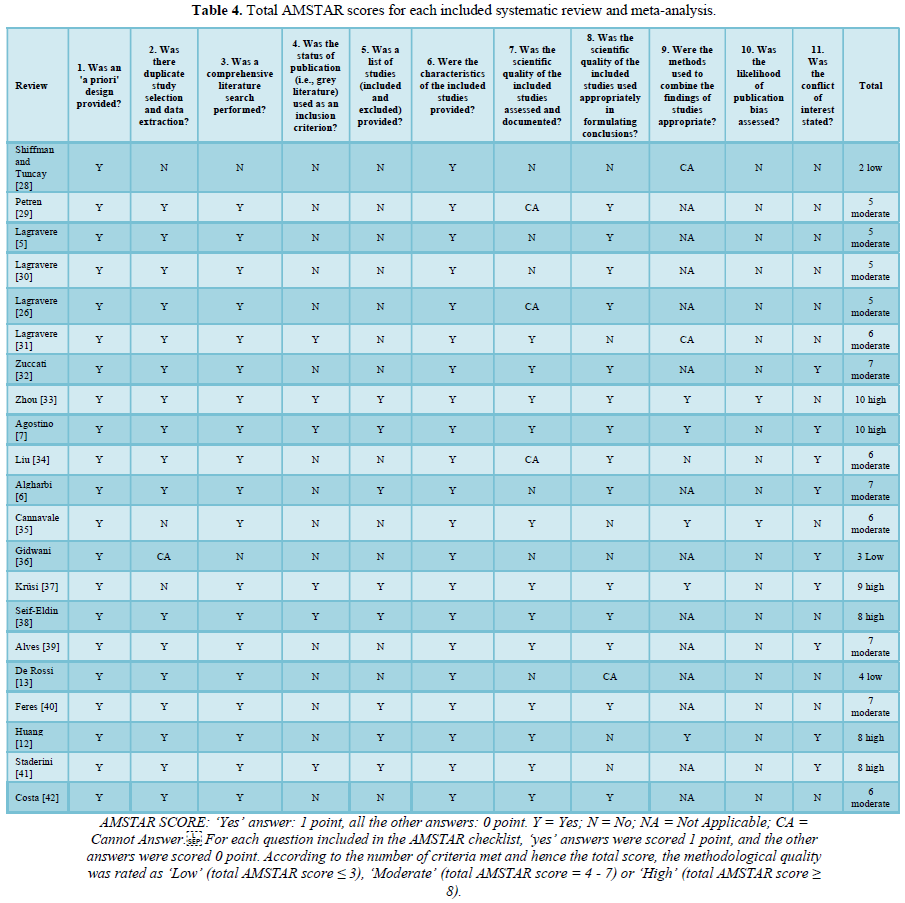
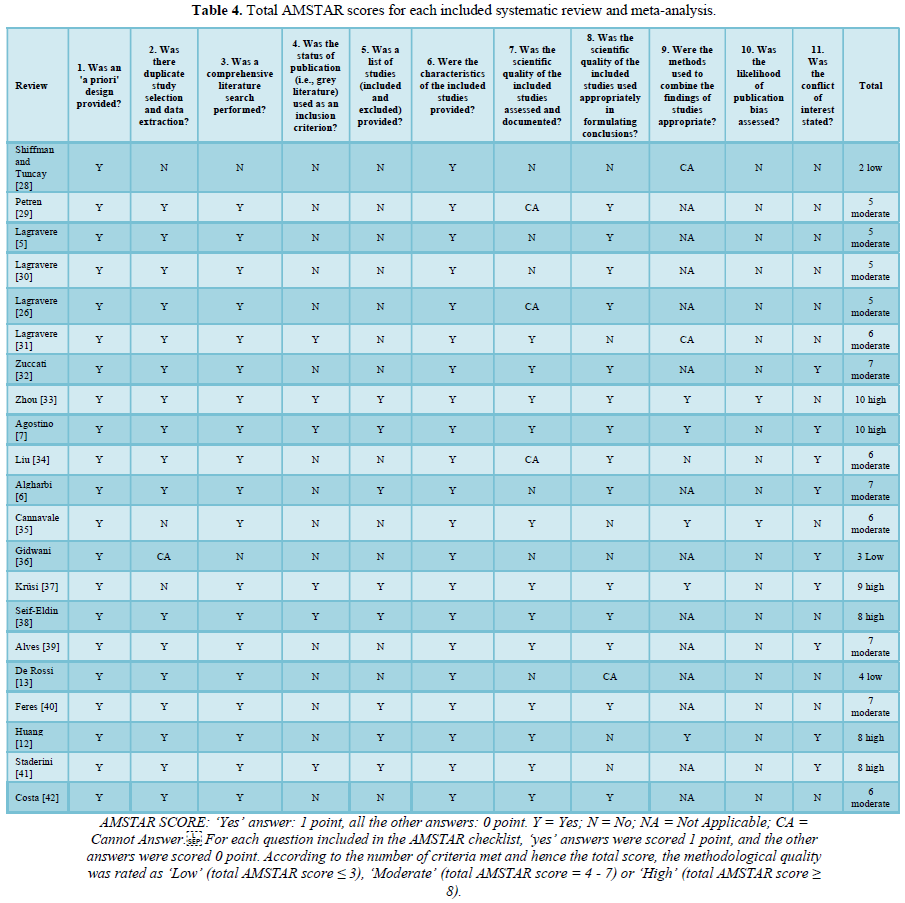
Methodological quality assessment of the included SRs and MAs
The methodological quality was assessed using ‘A Measurement Tool to Assess Systematic Reviews’ (AMSTAR) [18]. For each question included in the AMSTAR checklist, ‘yes’ answers were scored 1 point, and the other answers were scored 0 point. According to the number of criteria met and hence the total score, the methodological quality was rated as ‘Low’ (total AMSTAR score ≤ 3), ‘Moderate’ (total AMSTAR score = 4 - 7) or ‘High’ (total AMSTAR score ≥ 8). The inter-examiner reliability for the AMSTAR scores was calculated by means of Cohen’s k coefficient.
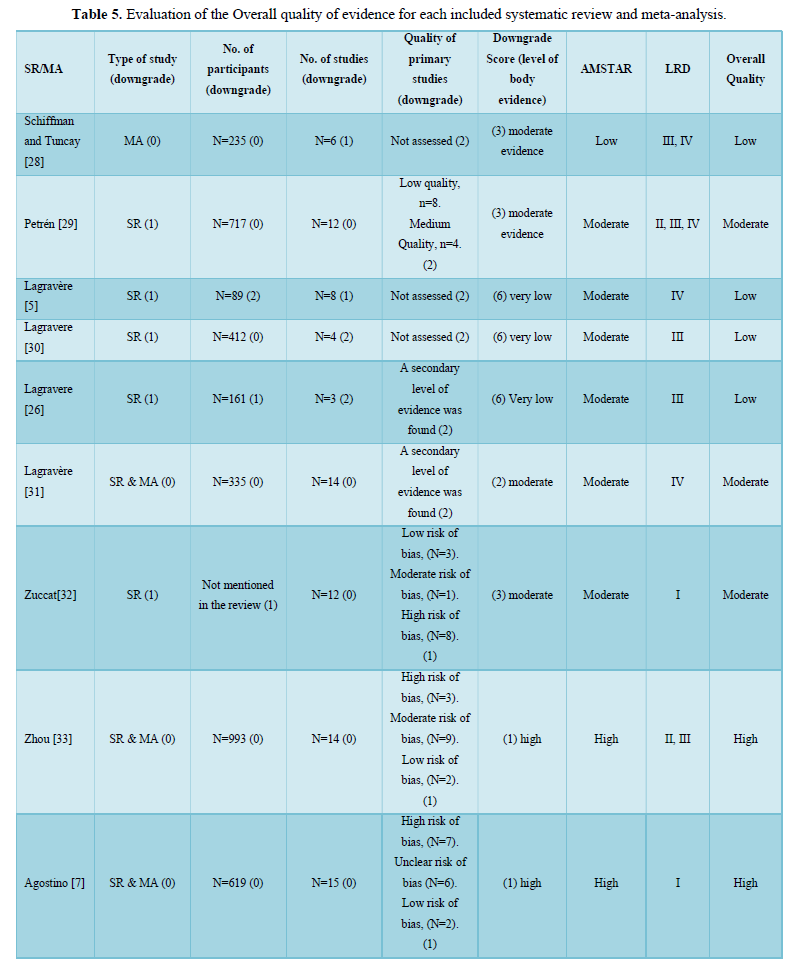
Quality assessment of the body of evidence
The design of the primary studies included in each SR/MA was assessed using the Level of Research Design scoring (LRD) [21-24], a scoring system based on the hierarchy of evidence.
For each SR/MA, the quality of the body of evidence was also appraised according to a pre-determined set of levels of evidence [8]. According to the number of downgrades/scores, the evidence of each review was classified as: very low (>5 downgrades), low (4-5 downgrades), moderate (2-3 downgrades) or high (0-1 downgrade) [8]. Quality of the individual studies was not reassessed, but stated as judged by the authors of the reviews. Finally, the overall quality of the review was assessed by the three reviewers (A.A., M.A., Y.M.) based on the individual AMSTAR [18], LRD [21-24] and body of evidence [8] scores.
RESULTS
Study selection: Search results and study selection are detailed in the PRISMA flow diagram in (Figure 1). A total of 4390 articles were identified through electronic and manual searching. After duplicates removal and screening by title and abstract, 30 studies were considered eligible and full texts were thoroughly inspected. 5 articles [1,8,25-27] were excluded following full-text examination. Harrison and Ashby [1] was excluded as it was updated in a recent review [10] which was included, Bucci [8] was an overview, Pithon [25] studied the combined effect of ME and facemask, Isfeld [26] evaluated technologies and methodologies capable of assessing MPS maturation, Andrade [27] studied the functional changes due to posterior crossbite rather than ME.
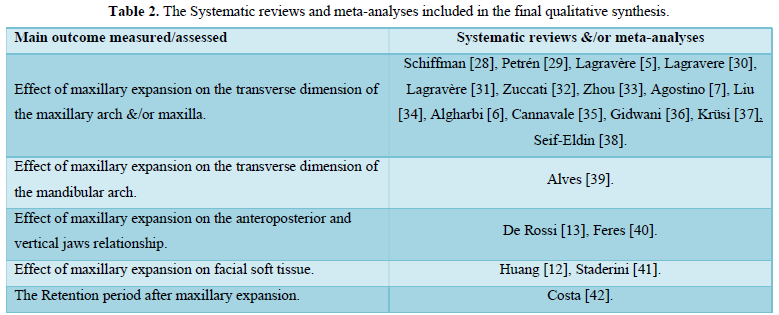
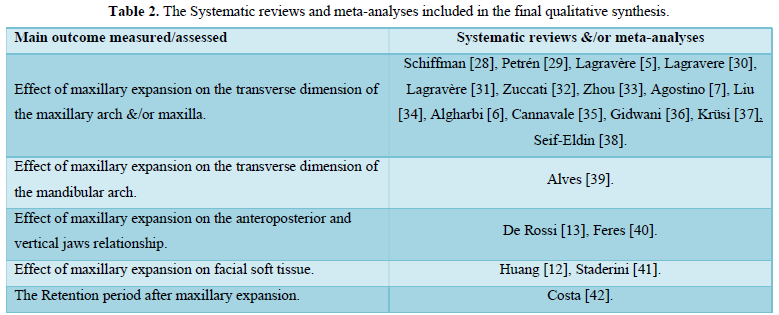
Finally, 25 SRs/MAs were included in the qualitative synthesis, and were classified according to their main outcome into 8 groups as shown in (Table 2).
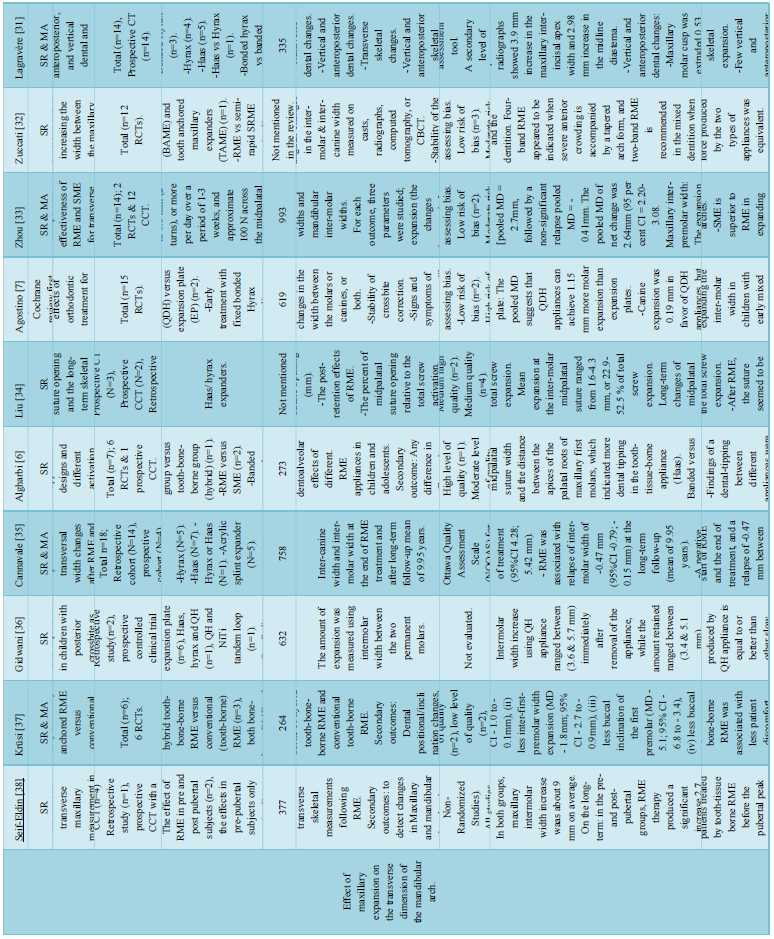
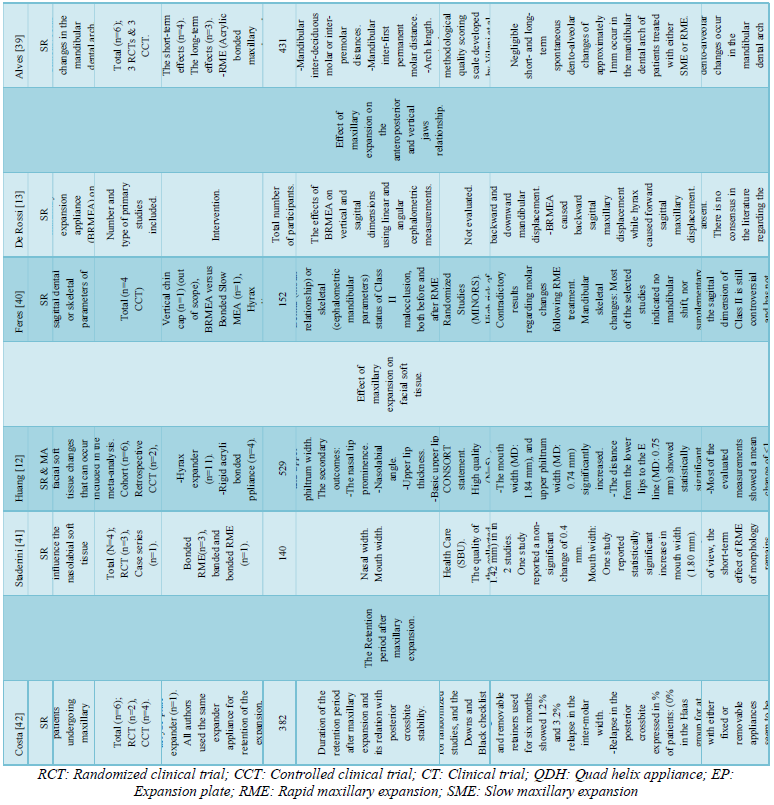
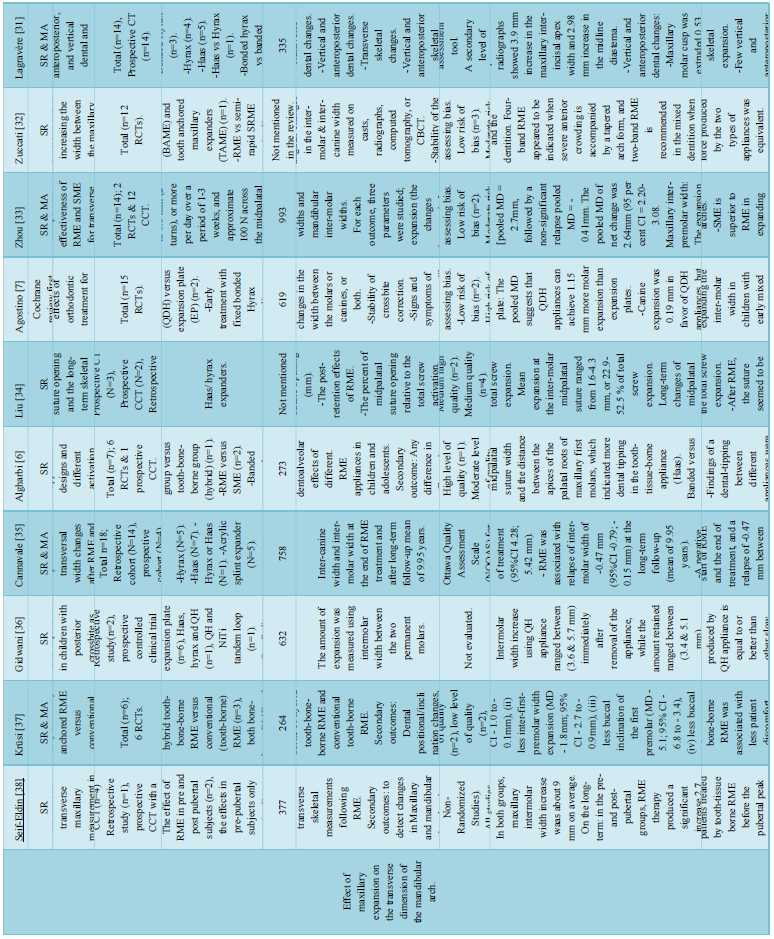
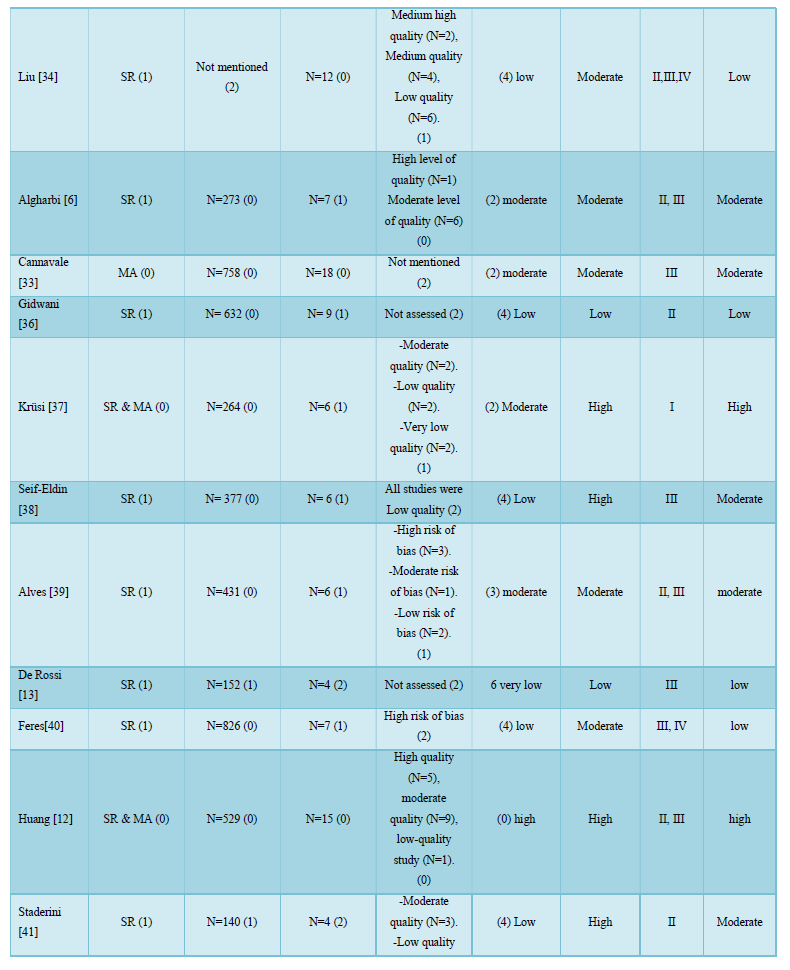
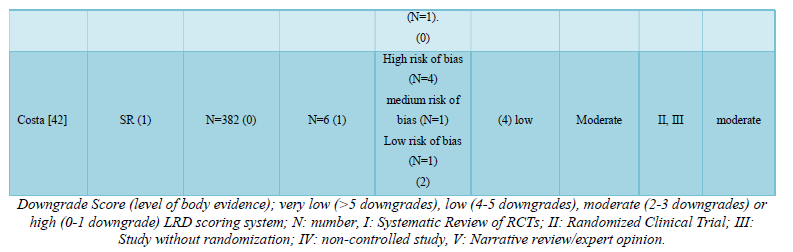
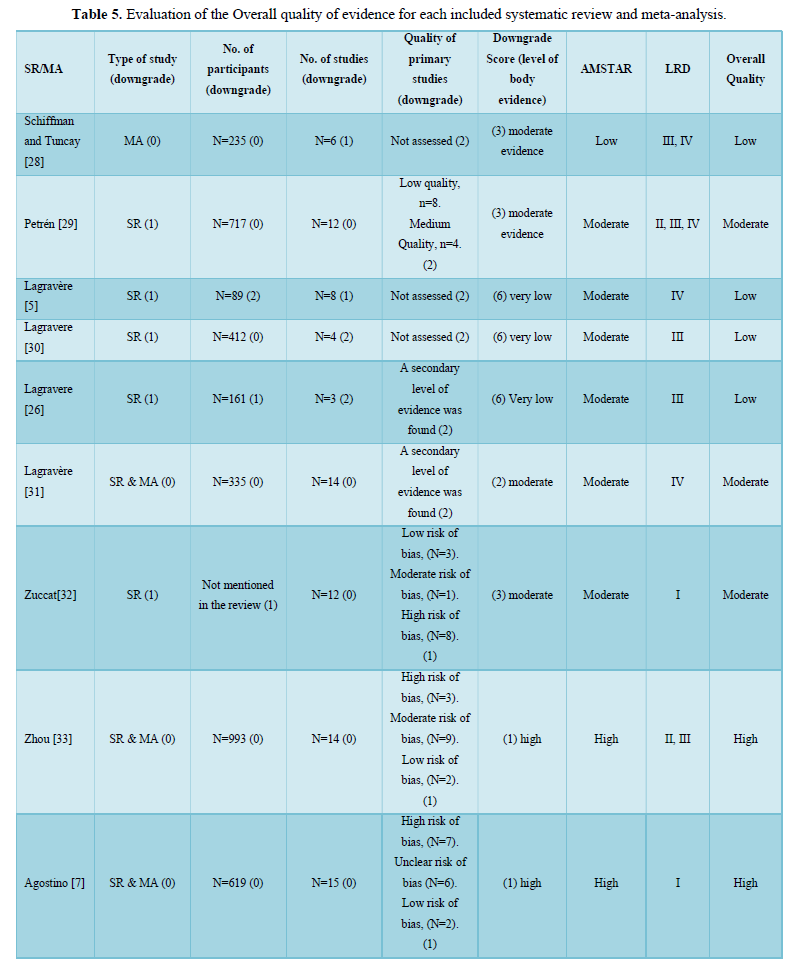
15 reviews [5,7,28-38] were primarily concerned with the effect of ME on the transverse dimension of the maxillary arch &/or maxilla, one review [39] was primarily concerned with the effect of ME on the transverse dimension of the mandibular arch, two reviews [13,40] studied the effect of ME on the anteroposterior and vertical jaws relationship, one review [11] studied the effect of ME on the adjacent sutures and orbital structures, two reviews [12,41] studied the effect of ME on facial soft tissue, one review [42] studied the retention period after ME, two reviews [43,44] studied the root resorption associated with ME, and one review [45] studied the periodontal problems associated with ME. The data extracted from each review are shown in (Table 3).
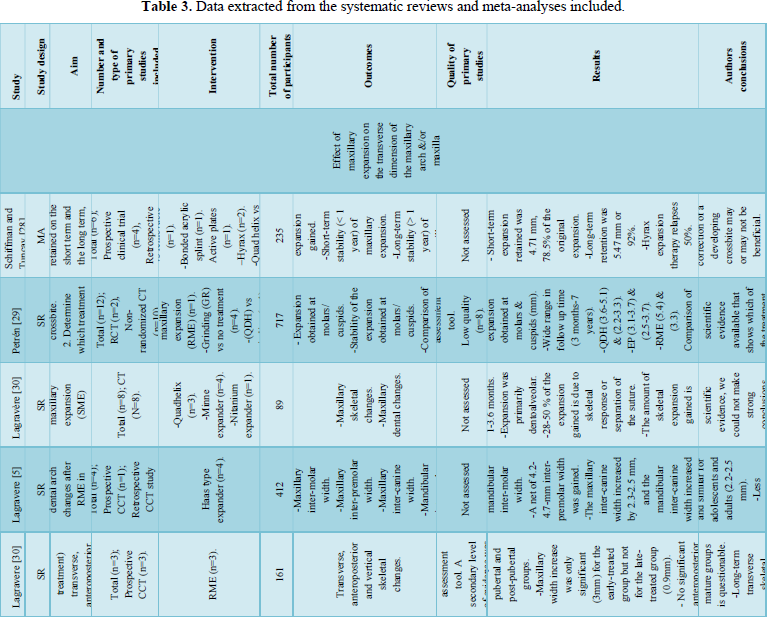
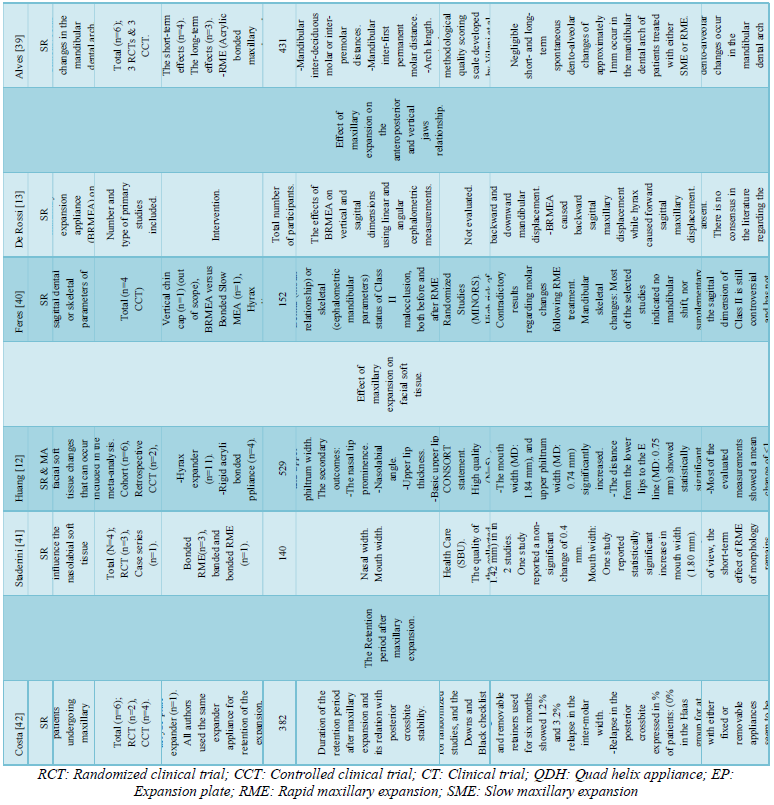
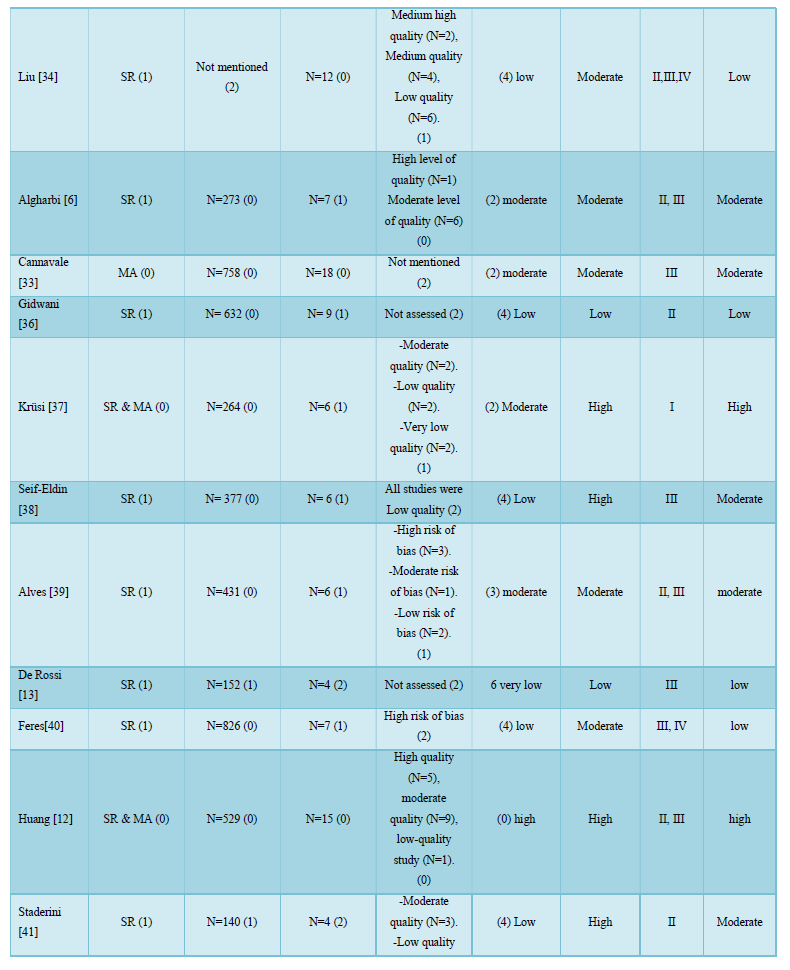
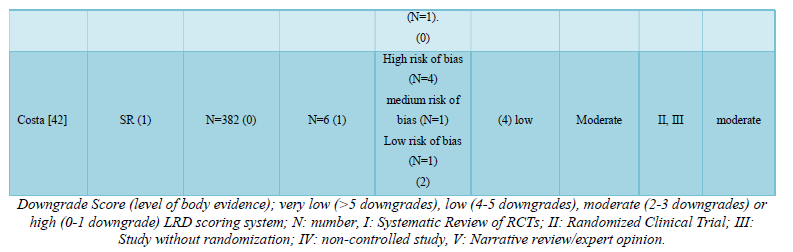
Quality assessment of the included SRs and MAs (AMSTAR & LRD)
The AMSTAR scores of the included reviews are shown in Table 4. The AMSTAR scores ranged from 2 to 10 (mean score 5). 3 reviews [13,28,36] were rated as low quality, 8 reviews [7,12,33,37,38,41,44,45] were rated as high quality and the rest were of moderate quality. The Cohen’s k coefficient for the AMSTAR was 0.826, indicating excellent inter-examiner agreement.
The body of evidence score [8] was calculated individually for each SR/MA in Table 5. Concerning the design of the primary studies (LRD score), only three reviews [7,32,37] included randomized controlled trials (RCTs) exclusively, meanwhile twelve reviews [6,11,12,29,33,34,36,39,41,42,44] included RCTs along with other types of studies as controlled clinical trials, prospective and retrospective clinical trials. Finally, the remaining reviews were based on non-randomized clinical trials and case series. The detailed LRD scores and the overall quality of evidence for each review are shown in Table 5.
- Effect of maxillary expansion on the transverse dimension of the maxillary arch &/or maxilla
The age of the patients throughout the studies ranged from 5 to 15 years; hence the following results can be applied to pre-pubertal and pubertal patients only. Short-term effects refer to the effect of treatment immediately post-expansion, while the long-term effect refers to the effect of treatment after a retention period.
Effect of slow maxillary expansion (SME):
Short-term dento-alveolar effects of SME:
- Compared to control, SME increased the maxillary inter-molar and inter-canine widths by 4.45 mm and 2.58 mm, in pre-pubertal and pubertal patients respectively [33], (Level of Research Design scoring (LRD)).
Long-term dento-alveolar effects of SME:
- The inter-molar and inter-canine widths expansion achieved after retention period (3-6 months) using SME were 2.49 mm and 2.27mm, in pre-pubertal and pubertal patients respectively [33], (HQE).
Short-term skeletal effects of SME:
- 28-50 % of the expansion gained was due to separation of the MPS. Expansion was primarily dento-alveolar and was inversely proportional to the age of the patient. However strong conclusions regarding skeletal changes after SME could not be withdrawn [5], (Low quality evidence (LQE)).
Different types of SME appliances:
- Quadhelix (QDH) appliances can achieve 1.15 mm more molar expansion than expansion plates (EP); fixed QDH appliances may be more successful than removable EP at correcting posterior crossbites and expanding the inter-molar width in children with early mixed dentition aged 8 to 10 years [7], (HQE).
- Treatment with the EP was unsuccessful in one third of the subjects; QDH appliance was superior to the EP in success rate and treatment time owing to better patient compliance [32], (Moderate quality evidence (MQE)).
- The amount of arch expansion produced by QH appliance is equal to or better than other slow maxillary expanders [36] (LQE).
Effect of rapid maxillary expansion RME:
Short-term dento-alveolar effects of RME:
- RME increased the maxillary inter-molar, inter-premolar and inter-canine widths by 4.09 mm, 3.86 mm and 2.7 mm in pre-pubertal and pubertal patients respectively [33], (HQE).
- At the end of RME treatment, there is an inter-molar and inter-canine width expansion of 4.85 mm and 3.73 mm respectively [35], (MQE).
- At younger ages, the amount of anterior expansion is similar to that of the posterior, and it diminishes during growth, becoming half that of the posterior at 15 years of age [35], (MQE).
- The changes in the maxillary transverse plane following RME treatment were caused by more dental than skeletal expansion [31], (MQE).
Long-term dento-alveolar effects of RME: Non-significant relapse in the maxillary inter-molar width (-0.40 mm), inter-premolar width (-0.16 mm), and inter-canine width (-0.41mm) occurred in the retention period (3-6 months) [33], (HQE). -The maxillary inter-molar, inter-premolar and inter-canine widths expansion gained due to RME treatment after retention period (3-6 months) were 3.58mm, 3.52 mm and 2.64mm respectively [33], (HQE). -There was a maxillary inter-canine width relapse of -0.81 mm between the end of treatment and long-term follow-up after a mean of 9.95 years, with an overall expansion of 2.91 mm. Regarding the inter-molar width, there is a relapse of -0.47 mm between the end of treatment and long-term follow-up of a mean of 9.95 years, with an overall gain of 4.38 mm [35], (MQE). Clinically significant long-term (minimum 1 year post retention) maxillary inter-molar width increase (3.7-4.8 mm) and inter-canine width increase (2.2-2.5 mm) can be achieved [30], (LQE).
Short-term skeletal effects of RME:
- RME was able to produce transverse skeletal effects on the maxilla by opening the MPS regardless of the palatal expander type. MPS opening during RME amounted to 12-52.5 % of the total screw expansion [34], (LQE). MPS opening during RME amounted to 20-50 % of the total screw expansion [11], (LQE). There was no consistent evidence on whether the MPS opening was parallel or triangular following RME [11,34], (LQE).
- Both bone-anchored and tooth-anchored maxillary expanders showed similar results; the dento-alveolar expansion gained was greater than skeletal expansion, however most of the studies were at high risk of bias therefore do not allow for sound comparison [32], (MQE).
Long-term skeletal effects of RME:
- Long-term changes of MPS opening following RME were not significant; the opening of the MPS was stable [34], (LQE). Long-term transverse skeletal ME is approximately 25% of the total appliance adjustment in pre-pubertal patients but non-significant for post-pubertal patients [30], (LQE). Long-term stability of transverse skeletal ME was better in pre-pubertal than pubertal and post-pubertal individuals [30,38], (MQE). The clinical significance of the long-term skeletal ME outcome in post-pubertal individuals is questionable [30], (LQE).
After a retention period post-expansion; bone-borne RME was associated with greater skeletal expansion at the incisal foramen (1.8 mm), greater suture opening at the first premolar (2.3 mm), and greater suture opening at the first molar (2.0 mm) than tooth-borne RME [37], (HQE).
Different types of RME appliances:
- Non-significant differences were observed in the inter-molar width expansion gained using tooth-borne Hyrax and tooth-tissue borne Haas, nor using banded and bonded Hyrax. However, the evidence was insufficient to conclude that any one intervention was better than another [7], (HQE). Non-significant differences were observed in the inter-molar width expansion gained using four-point and two-point banded hyrax, nor using tooth-borne and bone-born expander, yet the evidence was of low quality and do not allow for any sound comparison [7,32], (HQE). Dental-tipping effect between different appliances (Banded and bonded Hyrax, Tooth-borne and bone-borne expanders) were contradictory in the studies reviewed and no evidence-based conclusion could be drawn [6], (MQE). No significant differences between Bone-borne and tooth-borne RME could be identified for buccal tooth tipping, and root resorption [37], (HQE). Hybrid tooth-bone-borne RME was associated with less buccal tipping of the first premolar compared to tooth-borne RME post-retention, while no significant differences could be found regarding skeletal maxillary width and molar inclination [37], (HQE).
Comparison between different rates of expansion:
RME versus SME
- Both SME and RME are effective in treating posterior cross-bites in the early mixed dentition, however there is no evidence to show which of the treatment modalities was more effective [29], (MQE).
- Both RME & SME appliances are reliable methods for producing significant expansion at the MPS, which treats posterior crossbite effectively on the short-term [6], (MQE).
- The difference in the dental-tipping effect between RME & SME were contradictory in the studies reviewed and no evidence-based conclusion could be drawn [6], (MQE).
- In an age range of 8-14 years, the maxillary inter-molar width gain after the retention period (3-6 months) was significantly larger with SME than RME by 0.75 mm [33], (HQE).
- Non-significant differences were detected regarding post-expansion and post-retention maxillary inter-canine and inter-premolar widths using RME and SME [33], (HQE).
- Stable inter-molar and inter-canine widths were achieved using retention plate for 6 months following RME & SME, however most of the studies appear to be at high risk of bias therefore do not allow for any sound comparison between the stability of RME versus SME [32], (MQE).
RME versus semi-rapid (SRME)
- The evidence is insufficient to allow the conclusion that any intervention rate is better than another [7], (HQE).
Effect of primary teeth grinding:
- Grinding of the interferences as treatment in the primary dentition can be proposed [29], (MQE).
Effect of maxillary expansion on the transverse dimension of the mandibular arch
- The mandibular inter-molar width expansion gained due to SME immediately after treatment and retention period (3-6 months) were 0.49 mm and 0.06 mm in pre-pubertal and pubertal patients respectively [34], (HQE).
- The mandibular inter-molar width expansion gained due to RME immediately after treatment and the retention period (3-6 months) were 1.19 mm and 2.02 mm in pre-pubertal and pubertal patients respectively [34], (HQE).
- Non-significant differences were detected regarding post-expansion and post-retention mandibular inter-molar width using RME and SME [34], (HQE).
- Negligible short- and long-term spontaneous dento-alveolar changes of approximately 1mm occur in the mandibular arch of patients treated with either SME or RME in the mixed and early permanent dentition [40], (MQE).
- Less mandibular inter-molar and inter-canine width expansion was achieved in adults compared with adolescents treated with RME [30], (LQE).
Effect of maxillary expansion on the anteroposterior and vertical jaws relationship
- Anteroposterior and vertical dento-alveolar changes following RME:
- Immediately following RME, few vertical and anteroposterior dental changes were statistically significant, and none were clinically significant [32], (MQE).
- Regarding the effect of RME on Class II molar malocclusions, contradictory results regarding molar relationship changes following RME treatment [41], (LQE).
- No long-term anteroposterior or vertical dental changes were associated with RME [30], (LQE).
- Anteroposterior and vertical skeletal changes following RME:
- Immediately following RME treatment, few vertical skeletal changes were statistically significant, and none were clinically significant [32], (MQE).
- The effect of RME on the sagittal dimension of Class II is still controversial and has not been proved yet [41], (LQE).
- RME did not produce significant long-term anteroposterior or vertical skeletal changes in the position of the maxilla and mandible [31], (LQE).
- Different types of RME appliances:
- Bonded RME appliance caused less downward and backward displacement of the mandible than the banded appliances, but these alterations were not completely absent. There was not sufficient evidence to support the use of bonded RME appliances to control the undesirable vertical effects of RME [13], (LQE).
- Effect of maxillary expansion on the adjacent Sutures and orbital structures:
- All participants were pre-pubertal and pubertal patients (6-14.5 years).
- RME produced immediate significant changes in transverse dimensions of the circummaxillary sutures, spheno-occipital synchondrosis, and aperture width. Structures articulating directly with the maxilla (zygomaticomaxillary and frontomaxillary) had larger displacement than those located further away. However, the majority of the articles were judged to be of low quality, therefore no evidence-based conclusions could be drawn [11], (LQE).
- Effect of maxillary expansion on facial soft tissue:
- All subjects were in the facial skull growth phase (8-14 years).
- RME significantly increased nasal width, mouth width, upper philtrum width, and distance from the lower lip to the E line after the retention phase. No significant changes were detected in the height of the lower face, nose, or lips. However, most of the evaluated measurements showed a mean change of
- RME appliances produce slight clinically non-significant nasolabial soft tissue changes. In addition, the aesthetic impact provided by RME appliances may be considered as not clinically significant [42], (MQE).
- The Retention period after maxillary expansion:
- 24 h/ day of retention using the expansion appliance fixed in place or removable palatal plate for six months seemed enough to avoid relapse in the short-term [43], (MQE).
- Root resorption associated with maxillary expansion:
- CBCT radiography displayed significant root volume loss associated with RME. However, when considering volume loss percentages, no statistical significance was found [44], (LQE).
- RME caused root resorption of posterior teeth with the first molars being the most affected as assessed by CBCT. Root resorption was similar in anchored and unanchored teeth [45], (MQE).
- Periodontal problems associated with maxillary expansion:
- RME caused thinning of the alveolar buccal bone and reduction of the marginal bone level of anchored teeth less than 1 mm [54], (HQE).
- SME protocol seemed to cause more severe alveolar bone loss, bone dehiscence and periodontal impairment than RME [6, 54], (HQE).
DISCUSSION
Conducting overviews is the next rational step that should be taken in attempt to summarize and critically appraise the massive amount of evolving evidence. It can also serve as guidelines for both clinicians and researchers [47]. The current overview presented and evaluated the available evidence concerned with ME treatment effects, providing a comprehensive analysis of all reported short- and long-term outcomes of the different ME protocols. Unlike the previous ME overview conducted by Bucci [8], the aim of the present study was to report and criticize all the available three dimensional dental and craniofacial effects of ME, besides the direct effect of ME on the transverse maxillary dimension.
Quality of the evidence
It was of utmost importance to critically appraise and evaluate the included reviews with appropriate tools. The methodological quality of the included reviews was assessed with AMSTAR [18], a recent valid and reliable quality tool. 8 reviews [7,12,34,38,39,42,45,46] out of 25 were rated as high quality. Most of the studies lost points for not performing a grey literature search and not mentioning a list of excluded studies (Questions 4 and 5). Nevertheless, AMSTAR score evaluates whether a SR was conducted in appropriate way, without considering the design of the individual articles included in the SR. To overcome this shortcoming, the Level of Research Design Scoring (LRD) was also implemented, a score system based on the design of the primary studies according to the hierarchy of evidence [21-24]. Only three reviews [7,33,38] included randomized controlled trials (RCTs) exclusively, while the majority of SRs were based on non-randomized controlled clinical trials and clinical trials. The body of evidence was also evaluated individually for each review according to a scoring system adopted previously [8]. The overall quality of evidence was judged based on the individual AMSTAR, LRD and body of evidence scores, to be able to manipulate the scientific quality of the included reviews in formulating conclusions.
The highest overall quality was the Cochrane review conducted by Agostino [7]. This result is in agreement with what previously reported that Cochrane SRs present less shortcomings and superior methodological quality than other peer-reviewed SRs [48]. Krüsi [37] was also rated as a high-quality systematic review and meta-analysis owing to the high AMSTAR and LRD scores. Huang [12] and Zhou [34] were also judged as high-quality reviews, however the primary studies included were not solely based on RCTs. The remaining reviews were judged as moderate and low-quality evidence, all representing future research points to be able to reach solid guidelines and clinical recommendations.
Overall completeness and applicability of evidence
The age range of participants in all SRs/MAs were between 6-14 years, which is considered pre-pubertal and pubertal age. There is insufficient evidence on ME for post-pubertal patients. Although, treatment of posterior crossbite is recommended early up to the peak of pubertal growth, there is significant variation in the timing of skeletal maturation among individuals [9]. Moreover, MPS fusion is poorly correlated with age [10]. Accordingly, it was recommended that clinicians and researchers use proper diagnostic tools to individually assess MPS maturation to identify each patient’s ideal expansion treatment option and timing [10]. Prematurely referring a patient to surgically assisted ME, will expose him to a significant burden of treatment including increased pain, recovery time and expenses.
Summary of main results
HQE supported the short- and long-term dento-alveolar effects of SME [5] and RME [34,36] in growing patients, where both protocols successfully increased the inter-molar and inter-canine widths. Upon comparing both ME protocols, HQE supported that the maxillary inter-molar width expansion after a brief retention period was slightly greater using SME than RME by about 0.75mm [34]. However, this modest difference limits its clinical applicability.
The amount of skeletal expansion gained due to maxillary expanders was debatable. Only LQE supported the short-term skeletal effects of RME & SME protocols, which was assumed to be no more than 20-50 % of the total expansion gained [5,11,35]. Moreover, there was no evidence to detect the long-term skeletal effects of SME [5], while LQE supported the long-term stability of the MPS opening following RME [35], which was better retained in less skeletally mature individuals [31].
One of the aims of the current study was to formulate clinically useful recommendations regarding the best ME appliance and protocol for every dentition stage. Unfortunately, the evidence was insufficient to allow the conclusion that any ME rate (RME, SRME, SME) nor ME appliance is superior than another [6,7,33].
HQE also supported the spontaneous mild increase in the mandibular inter-molar width due to ME, however no significant differences were detected between RME and SME protocols [40].
Despite being accused of increasing the vertical dimension and pushing the maxilla forward [49,50], MQE supported the negligible vertical and anteroposterior changes occurring following RME on the short- and long-term [13,41].
Regarding soft tissue changes following ME, HQE pointed out negligible changes with limited clinical consequence [12,42]. The latter finding expands the indication of ME; it can be safely utilized with no significant profile changes.
MQE concluded that 24 h/day of retention for six months with either fixed or removable appliances are recommended to avoid relapse [43], unlike the traditional 3 months expansion which was long suggested [51].
Because of the considerable force needed to break the MPS during RME, and yet most of the treatment effect is dento-alveolar rather than skeletal expansion, it may be thought that RME may have detrimental effects on the teeth and their supporting tissues. Fortunately, MQE pointed out that non-significant root resorption occurred in the posterior teeth following RME when compared to the total root volume [44,45]. However, ME caused mild thinning of alveolar buccal bone and reduction of the marginal bone level of anchored teeth, attributed to the buccal tipping of the posterior teeth [46].
CONCLUSIONS
Implications for practice
Based on high quality evidence, the following could be concluded:
- Both RME and SME can effectively increase the maxillary inter-molar and inter-canine widths on the short- and long-term in pre-pubertal and pubertal patients.
- The maxillary inter-molar width gain after a retention period of 3-6 months was significantly larger in SME than in RME protocols by 0.75 mm pre-pubertal and pubertal patients. Regarding the maxillary inter-canine and inter-premolar widths, non-significant differences were detected.
- Fixed quad-helix appliances may be more successful than removable expansion plates at correcting posterior crossbites in children at early mixed dentition.
- In pre-pubertal and pubertal patients, mandibular inter-molar width expansion of approximately 1mm was gained due to SME and RME immediately after treatment and retention period (3-6 months), with non-significant differences detected between both protocols.
- RME increased nasal width, mouth width and upper philtrum width, and decreased lower lip thickness by
Based on moderate quality evidence, the following could be concluded:
- The maxillary transverse width increase following RME treatment was mainly dento-alveolar.
- At the end of the RME treatment, the inter-molar and inter-canine widths could be increased by 4.85 mm and 3.73 mm respectively. Upon long-term follow-up (mean of 9.95 years), an overall gain of 4.38 mm and 2.91 mm were detected.
- At younger ages, the amount of anterior expansion due to RME is similar to that of the posterior, and it diminishes with growth, becoming half that of the posterior opening at 15 years of age.
- On the short-term, clinically insignificant vertical and anteroposterior, dental and skeletal changes occur following RME protocol.
- Six months of full-time retention with either fixed or removable appliances seem to be enough to avoid relapse.
- RME side effects include root resorption of posterior teeth, affecting both anchored and unanchored teeth equally. Besides, RME causes thinning of alveolar buccal bone and reduction of the marginal bone level of anchored teeth less than 1 mm.
- SME protocol seemed to cause more severe alveolar bone loss than RME.
- Low level laser therapy seemed to improve the opening of the MPS and stimulate the repair process during the retention phase after RME, however did not increase the amount of expansion significantly.
- Grinding away of interferences as treatment for crossbite in the primary dentition can be proposed.
Based on low quality evidence, the following could be concluded:
- 28-50 % of the total expansion gained immediately following SME was due to skeletal response (MPS separation). Expansion was primarily dento-alveolar and inversely proportional to the age of the patient.
- MPS separation immediately following RME treatment constituted 20-50 % of the total expansion gained. There was no consistent evidence on whether the MPS opening was parallel or triangular.
- Long-term stability of the skeletal maxillary width increase following RME was stable, and was better retained in pre-pubertal than pubertal & post-pubertal individuals.
- CBCT radiography displayed significant root resorption associated with RME. However, when considering volume loss percentages, it was non-significant.
FUNDING
The authors did not have receive any funding to declare.
CONFLICTS OF INTEREST
The authors hereby declare that there are no conflicts of interest.
ETHICS APPROVAL
None.
- Harrison JE, Ashby D (2001) Orthodontic treatment for posterior crossbites. Cochrane database Syst Rev 2: CD000979.
- Mitchell L (2015) An introduction to orthodontics. Fourth Edition. 13: 47-53.
- Proffit WR, Fields HW, Sarver DM (2007) Summary of finding tables. 4th
- Manfredini D, Lombardo L, Siciliani G (2017) Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil 5: 908-923.
- Lagravere MO, Major PW, Flores-Mir C (2005) Skeletal and dental changes with fixed slow maxillary expansion treatment: A systematic review. J Am Dent Assoc 136: 194-199.
- Algharbi M, Bazargani F, Dimberg L (2018) Do different maxillary expansion appliances influence the outcomes of the treatment. Eur J Orthod 40(1): 97-106.
- Agostino P, Ugolini A, Signori A, Silvestrini-Biavati A, Harrison JE, et al. (2014) Orthodontic treatment for posterior crossbites. Cochrane Database Syst Rev 8: CD000979.
- Bucci R, D'Antò V, Rongo R, Valletta R, Martina R et al. (2016) Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and meta-analyses. J Oral Rehabil 43(7): 543-564.
- Baccetti T, Franchi L, Cameron CG, McNamara JA (2001) Treatment timing for rapid maxillary expansion. Angle Orthod 71: 343-350.
- Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, et al. (2013) Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofac Orthop 144: 759-769.
- Bazargani F, Feldmann I, Bondemark L (2013) Three-dimensional analysis of effects of rapid maxillary expansion on facial sutures and bones. Angle Orthod 83(6): 1074-1082.
- Huang J, Li CY, Jiang JH (2018) Facial soft tissue changes after nonsurgical rapid maxillary expansion: A systematic review and meta-analysis. Head Face Med 14(1): 6.
- De Rossi M, Rocha R, Gavio M (2016) Effects of bonded rapid maxillary expansion appliance (brmea) in vertical and sagittal dimensions: A systematic review. Braz J Oral Sci 7(25): 1571-1574.
- Ellabban MT, Abdul-Aziz AI, Fayed MMS, Aboul Fotouh MH, Elkattan ES, et al. (2018) Positional and dimensional temporomandibular joint changes after correction of posterior crossbite in growing patients: A systematic review. Angle Orthod 88(5): 638-648.
- Buck LM, Dalci O, Darendeliler MA, Papageorgiou SN, Papadopoulou AK (2017) Volumetric upper airway changes after rapid maxillary expansion: A systematic review and meta-analysis. Eur J Orthod 39(5): 463-473.
- Lagravère MO, Gamble J, Major PW, Heo G (2013) Transverse dental changes after tooth-borne and bone-borne maxillary expansion. Int Orthod 11(1): 21-34.
- Nordmann AJ, Kasenda B, Briel M (2012) Meta-analyses: What they can and cannot do. Swiss Med Wkly 142: w13518.
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, et al. (2007) Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 15: 7-10.
- Smith V, Devane D, Begley CM, Clarke M (2011) Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 11: 15.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med 62(10): e1-34.
- Rogante M, Kairy D, Giacomozzi C, Grigioni M (2015) A quality assessment of systematic reviews on telerehabilitation: What does the evidence tell us? Ann Ist Super Sanità 46: 11.
- Antes G (1998) Evidence-based medicine. Internist (Berl) 39: 899-908.
- Cooke IE (1996) Finding the evidence. Bailli_ere’s Clin Obstet Gynaecol 10: 561-567.
- D'Antò V, Bucci R, Franchi L, Rongo R, Michelotti A, et al. (2015) Class II functional orthopedic treatment: A systematic review of systematic reviews. J Oral Rehabil 42(8): 624-642.
- Pithon MM, Santos NL, Santos CR, Baião FC, Pinheiro MC, et al. (2016) Is alternate rapid maxillary expansion and constriction an effective protocol in the treatment of Class III malocclusion? A systematic review. Dental Press J Orthod 21(6): 34-42.
- Isfeld D, Lagravere M, Leon-Salazar V, Flores-Mir C (2017) Novel methodologies and technologies to assess mid-palatal suture maturation: A systematic review. Head Face Med 13(1): 13.
- Andrade AS, Gameiro GH, Derossi M, Gavião MB (2009) Posterior crossbite and functional changes. A systematic review. Angle Orthod 79(2): 380-386.
- Schiffman PH, Tuncay OC (2001) Maxillary expansion: A meta-analysis. Clin Orthod Res 4(2): 86-96.
- Petrén S, Bondemark L, Söderfeldt B (2003) A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod 73(5): 588-596.
- Lagravere MO, Major PW, Flores-Mir C (2005) Long-term dental arch changes after rapid maxillary expansion treatment: A systematic review. Angle Orthod 75(2): 155-161.
- Lagravère MO, Heo G, Major PW, Flores-Mir C (2006) Meta-analysis of immediate changes with rapid maxillary expansion treatment. J Am Dent Assoc 137(1): 44-53.
- Zuccati G, Casci S, Doldo T, Clauser C ( (2013Expansion of maxillary arches with crossbite: A systematic review of RCTs in the last 12 years. Eur J Orthod. 35(1): 29-37.
- Zhou Y, Long H, Ye N, Xue J, Yang X, et al. (2014) The effectiveness of non-surgical maxillary expansion: A meta-analysis. Eur J Orthod 36(2): 233-242.
- Liu S, Xu T, Zou W (2015) Effects of rapid maxillary expansion on the midpalatal suture: A systematic review. Eur J Orthod 37(6): 651-655.
- Cannavale R, Chiodini P, Perillo L, Piancino MG (2018) Rapid palatal expansion (RPE): Meta-analysis of long-term effects. Orthod Craniofac Res 21(4): 225-235.
- Gidwani KV, Bendgude VD, Kokkali VV, Mehta V (2018) Comparison of effectiveness of quad helix appliance with other slow maxillary expanders in children with posterior crossbite: A systematic review. J Indian Soc Pedod Prev Dent 36(3): 225-233.
- Krüsi M, Eliades T, Papageorgiou SN (2019) Are there benefits from using bone-borne maxillary expansion instead of tooth-bornemaxillary expansion? A systematic review with meta-analysis. Prog Orthod 20(1): 9.
- Seif-Eldin NF, Elkordy SA, Fayed MS, Elbeialy AR, Eid FH (2019) Transverse Skeletal Effects of Rapid Maxillary Expansion in Pre and Post Pubertal Subjects: A Systematic Review. Open Access Maced J Med Sci 7(3): 467-477.
- Alves ACM, Maranhão OBV, Janson G, Garib DG (2017) Mandibular dental arch short and long-term spontaneous dentoalveolar changes after slow or rapid maxillary expansion: A systematic review. Dental Press J Orthod 22(3): 55-63.
- Feres MF, Raza H, Alhadlaq A, El-Bialy T (2015) Rapid maxillary expansion effects in Class II malocclusion: A systematic review. Angle Orthod 85(6): 1070-1079.
- Staderini E, Patini R, De Luca M, Gallenzi P (2018) Three-dimensional stereophotogrammetric analysis of nasolabial soft tissue effects of rapid maxillary expansion: A systematic review of clinical trials. Acta Otorhinolaryngol Ital 38(5): 399-408.
- Costa JG, Galindo TM, Mattos CT, Cury-Saramago AA (2017) Retention period after treatment of posterior crossbite with maxillary expansion: A systematic review. Dental Press J Orthod 22(2): 35-44.
- Forst D, Nijjar S, Khaled Y, Lagravere M, Flores-Mir C (2014) Radiographic assessment of external root resorption associated with jackscrew-based maxillary expansion therapies: A systematic review. Eur J Orthod 36(5): 576-585.
- Lo Giudice A, Galletti C, Gay-Escoda C, Leonardi R (2018) CBCT assessment of radicular volume loss after rapid maxillary expansion: A systematic review. J Clin Exp Dent 10(5): e484-e494.
- Lo Giudice A, Barbato E, Cosentino L, Ferraro CM, Leonardi R (2018) Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur J Orthod 40(3): 296-303.
- Jadad AR, Cook DJ, Jones A, Klassen TP, Tugwell P, et al. (1998) Methodology and reports of systematic reviews and meta-analyses: A comparison of Cochrane reviews with articles published in paper-based journals. JAMA 280(3): 278-280.
- Akkaya S, Lorenzon S, Uçem TT (1999) A comparison of sagittal and vertical effects between bonded rapid and slow maxillary expansion Eur J Orthod 21(2): 175-180.
- Halicioğlu K, Yavuz I (2016) A comparison of the sagittal and vertical dentofacial effects ofmaxillary expansion produced by a memory screw and a hyrax screw. Aust Orthod J 32(1): 31-40.
- Graber TM (1969) Chapter 10. Dentofacial orthopedics. In: Graber TM, editor.Current orthodontic concepts and techniques. Philadelphia: WB Saunders Company. Vol: 11.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Pathology and Toxicology Research



