5104
Views & Citations4104
Likes & Shares
- Proper positioning of the baby with a roll placed under the shoulder and the head turned to the contralateral side
- Deep sedation increases the cannulation success
- Prescanning of veins i.e., RaCeVA: Rapid Central Vein Assessment
- Size measurement of the targeted vein sonographically because the caliber of the catheter must not exceed ⅓ of the vessel lumen in order to avoid thrombosis
- Maximal barrier precautions including skin antisepsis with 2% chlorhexidine in 70% isopropilic alcohol
- USG venipuncture by using a high-quality ultrasound machine with a small broadband linear array transducer providing a resolution between 13-22MHz
- Seldinger technique by inserting a soft tipped, straight 0.018-inch (0.46mm) Nitinol guidewire
- Ultrasound assessment of the direction of the guidewire into the vasculature i.e., tip navigation
- Insertion of preferably power injectable 2-4 Fr catheters made from silicone or polyurethane
- Tip location by intracavitary ECG and/or transthoracic echocardiography
- Consider subcutaneous tunneling of the catheter to the infraclavicular area if the catheter is to remain in place for a longer period of time
- Securement by sutureless devices such as Securcath®, Grip-Lok®, or StatLock®
- Cyanoacrylate glue for the closure of the puncture site and for the sealing of the exit site
- Coverage of the exit site with semipermeable transparent membrane
FEMORAL VEIN CANNULATION (FICC, FEMORALLY INSERTED CENTRAL CATHETER)
A towel is folded and placed under the pelvic region to eliminate any inward flexion of the hips or concavity to the area. The US probe is placed so as to obtain a good short-axis view of the femoral vein. By using usually an OOP technique which can also include a DNTP technique the needle is inserted into the vein. After successful puncture of the vein Seldinger technique is applied. Femoral venous cannulations can be difficult in neonates because of the small size of the vein, its collapse, and the narrow angle making sometimes the insertion of the guide-wire difficult. High catheter related obstruction, infection, and thrombosis rates have been described, however, recently Ostroff [26] has reported the successful long-term use of tunneled femoral venous catheters in neonates [15,25].
COMPLICATIONS
Due to the meticulous use of real-time USG cannulation techniques including a proper training in this field fatal puncture complications should not occur any more. Inadvertent arterial injuries are now reported to be below 1% [1-3]. Likewise, by applying the previously mentioned insertion bundles, long term complications in particular catheter related infections, and thrombosis should also be avoided nearly completely. However, it has to be said that catheter dwell time, small size of the veins, and overall extreme fragility of these babies will remain constant risk factors for complications. Apart from this ultrasound has also become the first choice to diagnose/exclude pneumothorax, pericardial effusion, and thrombotic events [27]. The latter one must not be confounded with the harmless fibroelastic sheaths frequently detected in vessels after catheter removal.
CONCLUSION
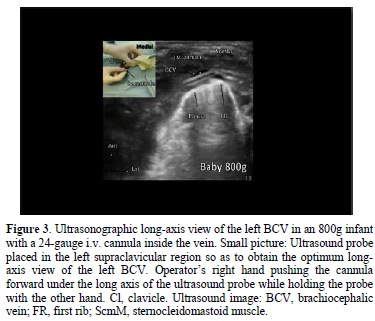
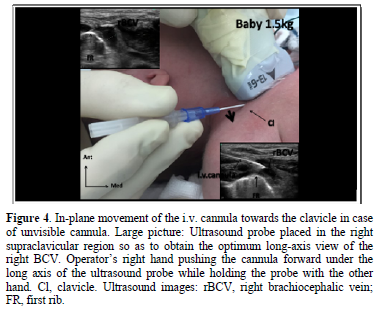
The most appropriate access in neonates seems to be the supraclavicular, USG in-plane cannulation of the BCV. By using the insertion bundles meticulously fatal catheter complications should not occur any more.
- Barone G, Pittiruti M, Ancora G, Vento G, Tota F, et al. (2020) Centrally inserted central catheters in preterm neonates with weight below 1500 g by ultrasound-guided access to the brachiocephalic vein. J Vasc Access 10: 1129729820940174.
- Montes-Tapia F, Rodríguez-Taméz A, Cura-Esquivel I, Barreto-Arroyo I, Hernández-Garduño A, et al. (2016) Efficacy and safety of ultrasound-guided internal jugular vein catheterization in low-birth-weight newborn. J Pediatr Surg 51(10): 1700-1703.
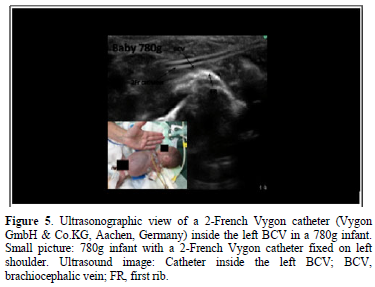
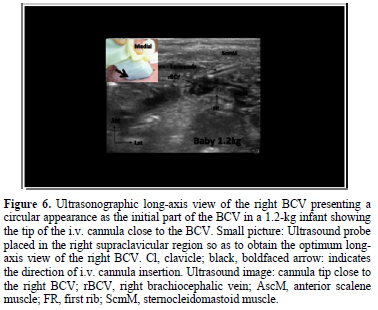
- Breschan C, Graf G, Arneitz C, Stettner H, Feigl G, et al. (2020) Feasibility of the ultrasound-guided supraclavicular cannulation of the brachiocephalic vein in very small weight infants: A case series. Paediatric Anaesth 30(8): 928-933.
- Breschan C, Graf G, Jost R, Stettner H, Feigl G, et al. (2018) A retrospective analysis of the clinical effectiveness of supraclavicular, ultrasound-guided brachiocephalic vein cannulations in preterm infants. Anesthesiology 128(1): 38-43.
- Breschan C, Kraschl R, Krenn R, Krumpholz R, Jost R, et al. (2000) Anesthetic management of liver hemorrhage during laparotomy in a premature infant with necrotizing enterocolitis. Pediatr Anesth 4: 425-428.
- Stevens B, Johnston C, Franck L, Petryshen P, Jack A, et al. (1999) The efficacy of developmentally sensitive interventions and sucrose for relieving procedural pain in very low birth weight neonates. Nurs Res 48(1): 35-43.
- Crawford M, Soukup SM, Woods SS, Deisch P (2000) Peripherally inserted central catheter program. Nurs Clin North Am 35: 349‑360.
- Ahn Y (2006) The relationship between behavioral states and pain responses to various NICU procedures in premature infants. J Trop Pediatr 52: 201‑205.
- Pandit PB, Pandit FA, Govan J, O'Brien K (1999) Complications associated with surgically placed central venous catheters in low-birth-weight neonates. J Perinatol 19: 106-109.
- Wu J, Mu D (2012) Vascular catheter-related complications in newborns. J Paediatr Child Health 48: E91-E95.
- Hsu CC, Kwan GN, Evans-Barns H, Rophael JA, van Driel ML (2016) Venous cutdown versus the Seldinger technique for placement of totally implantable venous access ports. Cochrane Database Syst Rev 8: CD008942.
- Blum LV, Abdel-Rahman U, Klingebiel T, Fiegel H, Gfroerer S, et al. (2017) Tunneled central venous catheters in children with malignant and chronic diseases: A comparison of open vs. percutaneous implantation. J Pediatr Surg 52: 810-812.
- Kim JH, Lee YS, Kim SH, Lee SK, Lim MK, et al. (2001) Does umbilical vein catheterization lead to portal venous thrombosis? Prospective US evaluation in 100 neonates. Radiology 219(3): 645-650.
- Breschan C, Platzer M, Jost R, Schaumberger F, Stettner H, et al. (2007) Comparison of catheter-related infection and tip colonization between internal jugular and subclavian central venous catheters in surgical neonates. Anesthesiology 107(6): 946-953.
- Habas F, Baleine J, Milési C, Combes C, Didelot MN, et al. (2018) Supraclavicular catheterization of the brachiocephalic vein: a way to prevent or reduce catheter maintenance-related complications in children. Euro J Pediatr 177(3): 451-459.
- Oulego-Erroz I, Alonso-Quintela P, Terroba-Seara S, Jiménez-González A, Rodríguez-Blanco S, et al. (2018) Ultrasound-Guided Cannulation of the Brachiocephalic Vein in Neonates and Preterm Infants: A Prospective Observational Study. Am J Perinatol 35(5): 503-508.
- Goldstein SD, Pryor H, Salazar JH, Dalesio N, Stewart FD, et al. (2015) Ultrasound-Guided Percutaneous Central Venous Access in Low-Birth-Weight Infants: Feasibility in the Smallest of Patients. J Laparoendosc Adv Surg Tech A 25(9): 767-769.
- Di Nardo M, Tomasello C, Pittiruti M, Perrotta D, Marano M, et al. (2011) Ultrasound-guided central venous cannulation in 374 infants weighing less than 5 kilograms. J Vasc Access 12(4): 321-324.
- Pirotte T, Veyckemans F (2007) Ultrasound-guided subclavian vein cannulation in infants and children: A novel approach. Br J Anaesth 98: 509-514.
- Breschan C, Platzer M, Jost R, Stettner H, Likar R (2010) Size of internal jugular vs subclavian vein in small infants: an observational, anatomical evaluation with ultrasound. Br J Anaesth 105(2): 179-184.
- Eifinger F, Brisken K, Roth B, Koebke J (2011) Topographical anatomy of central venous system in extremely low-birth weight neonates less than 1000 grams and the effect of central venous catheter placement. Clin Anat 24(6): 711-716.
- Breschan C, Graf G, Jost R, Stettner H, Feigl G, et al. (2015) Ultrasound-guided supraclavicular cannulation of the right brachiocephalic vein in small infants: A consecutive, prospective case series. Pediatr Anesth 25(9): 943-949.
- Breschan C, Platzer M, Jost R, Stettner H, Feigl G, et al. (2012) Ultrasound-guided supraclavicular cannulation of the brachiocephalic vein in infants: A retrospective analysis of a case series. Pediatr Anesth 22(11): 1062-1067.
- Breschan C, Platzer M, Jost R, Stettner H, Beyer AS, et al. (2011) Consecutive, prospective case series of a new method for ultrasound-guided supraclavicular approach to the brachiocephalic vein in children. Br J Anaesth 106(5): 732-737.
- Dubbink-Verheij GH, Pelsma ICM, van Ommen CH, Smits-Wintjens VEHJ, Visser R, et al. (2018) Femoral Vein Catheter is an Important Risk Factor for Catheter-related Thrombosis in (Near-)term Neonates. J Pediatr Hematol Oncol 40(2): e64-e68.
- Ostroff M, Zauk A, Chowdhury S, Moureau N, Mobley C (2020) A retrospective analysis of the clinical effectiveness of subcutaneously tunneled femoral vein cannulations at the bedside: A low risk central venous access approach in the neonatal intensive care unit. J Vasc Access 5: 1129729820969291.
- Lichtenstein DA, Meziere G, Lascols N, Biderman P, Courret JP (2005) Ultrasound diagnosis of occult pneumothorax. Crit Care Med 33: 1231-1238.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Alcoholism Clinical Research
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Spine Diseases








