4485
Views & Citations3485
Likes & Shares
Background: Patients admitted in the hospital following SARS-CoV-2 infection often experience hypoxic respiratory failure and a proportion require invasive mechanical ventilation to maintain adequate oxygenation. The combination of prone positioning and non-invasive ventilation in awake patients may have a role in improving oxygenation.
Aim and Objective: To compare the efficacy of BiPAP ventilator in covid-19 positive patients for prone VS Supine positions and to evaluate the outcome of the patients.
Materials and Methods: This is a prospective simple randomized study conducted in 200 COVID-19 positive patients admitted in COVID ICU, divided in two groups, each consists of 100. Group A- BiPAP on prone position and Group B- BiPAP on supine position. SpO2, PaO2 /FiO2 were compared. Other parameters like heart rate, blood pressure and respiratory rate were observed.
Statistical Analysis: The observed results in our study was calculated by using unpaired Student’s t test or Mann-Whitney test to compare among Group A and Group B.
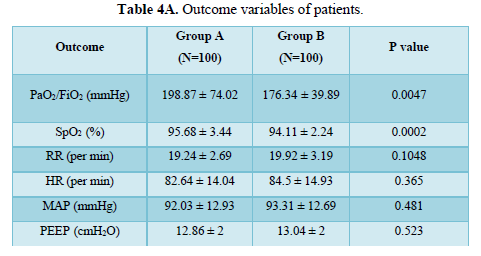
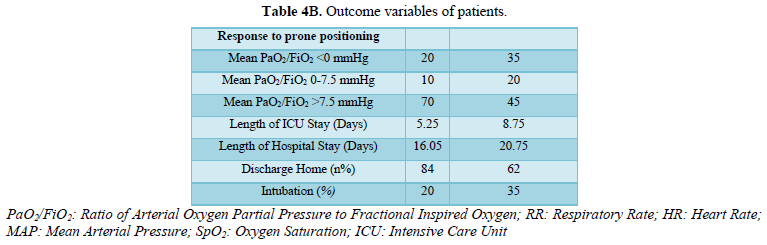
Results: The baseline characteristics were similar in the two groups. In Group A, PaO2/FiO2 became significantly higher than the group B (P value < 0.001). Proportion of patients requiring intubation in group A and group B (20% vs 35%). Length of hospital stay in days was (16.05 vs 20.75). There was no significant difference in heart rate, blood pressure and respiratory rate. There was significant improvement in SpO2 in group A as compare to group B (95.68 ± 3.44 vs 94.11 ± 2.24) (P value < 0.001).
Conclusions: Prone positioning in conjunction with BiPAP can improve oxygenation without any significant adverse effects in COVID-19 patients. Moreover, it decreases hospital stay of the patient and eventually it benefits economy of hospital. Prone positioning along with NIV is prudent tool in management of moderate to severe ARDS.
Keywords: Awake positioning, Prone positioning, Non-invasive ventilation, ARDS
ABBREVIATIONS
BiPAP: Bilevel Positive Airway Pressure; PP: Prone Position; BMI: Body Mass Index; M: Male; F: Female; PaO2/FiO2: Ratio of Arterial Oxygen Partial Pressure to Fractional Inspired Oxygen; SpO2: Oxygen Saturation; RR: Respiratory Rate; HR: Heart Rate; MAP: Mean Arterial Pressure;
INTRODUCTION
SARS-CoV-2 or the Novel Corona Virus (belonging to the zoonotic virus group Corona virus that caused MERS, SARS) is the ongoing global pandemic. The disease named COVID-19 is featured by flu like symptoms of fever, sore throat, headaches, dyspnea, cough, generalized bodyache, anosmia, loss of taste and acute respiratory symptoms [1]. Majority of cases are asymptomatic or mildly symptomatic (81%). However, this disease is aggravated in many patients which lead to pulmonary edema, multi-organ failure, and acute respiratory distress syndrome (ARDS). Critical disease (respiratory failure, shock, MODS) is reported in about 5%. Death reported in 3.4% [2]. Prone position is one of the most effective and supportive therapy for ministrations of ARDS patients [3]. Prone positioning ventilation is one of the prophylactic managements to avoid ventilator-induced lung injury in critically ill patients who suffered from ARDS [4]. The logic is to alleviate ventilation/perfusion mismatching, hypoxemia and shunting in such prone category patients [5]. Lung ventilation from dorsal to ventral areas is more homogeneous in the prone position. Thus, prone positioning improves oxygenation while perfusion remains constant in both postures [6,7]. Due to uniform ventilatory and perfusion strategy, there is persistent decrease in ventilation perfusion mismatch [8]. Prone positioning in non-intubated patients could prevent the need for intubation and so avoid the risk of harm associated with a stay in the ICU, such as ventilator induced lung injury. Early use of NIV can reduce the need for intubation in ARDS patients. NIV applies end-expiratory airway pressure (PEEP) and pressure support (PS). Optimally, PEEP increases functional residual capacity and opens collapsed alveoli, thereby improving ventilation-perfusion matching and reducing intrapulmonary shunt, as well as improving lung compliance, thus reducing respiratory load. The latter assists respiratory muscles during inspiration, reducing the work of breathing and dyspnea. Non invasive ventilation (NIV) is generally defined as mode of ventilatory support which consists of PEEP and pressure support. PEEP therapy has effective role in quick declining of functional residual capacity (FRC) and intrapulmonary shunt. To this point, there is overall refinement in V/Q mismatch which aids decrease work of breathing [9].
MATERIALS AND METHODS
This prospective simple randomized study was performed in ICU of tertiary care hospital after obtaining institutional ethics committee (GCSMC/EC/Proj/Approve/2020/156) and written informed consent. This study was also registered under (CTRI/2020/08/027080).
Study was carried out with 200 confirmed COVID-19 patients, they were divided into two groups. Each group consists of 100 patients.
Group A (100): Patients on BiPAP with prone position
Group B (100): Patients on BiPAP with supine position
Inclusion criteria
COVID-19 patients with ARDS meeting Berlin criteria, age 30-80 years, BMI < 30 kg/m2, FiO2 requirement more than 50%.
Exclusion criteria
COVID negative patients, drowsy patient, uncooperative, Glassgow Coma Scale < 6, PaO2/FiO2 30 kg/m2, Age 80 years, cervical spondylosis, glaucoma, pregnancy.
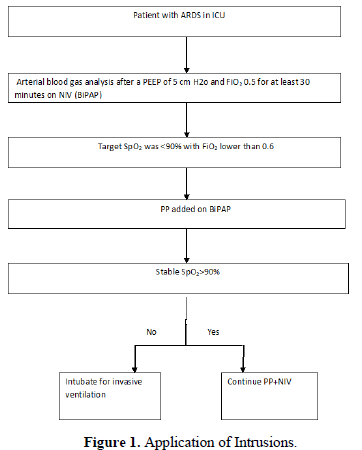
Data was collected after admission to the intensive care unit after confirmation of COVID-19 by reverse transcriptase polymerase chain reaction (RT-PCR). We included patients with moderate to severe ARDS according to Berlin criteria [10]. Patients whose requirement are more than standard oxygen therapy were put on BiPAP. Additionally, BiPAP settings of PEEP 5 cmH20 and FiO2 50% for at least 30 min were analyzed after proper ABG interpretation. In accordance with this setting, if there was no improvement in PaO2/FiO2 ratio, PEEP was gradually increased according to patient’s clinical condition. Indicated patients who needed BiPAP support when PaO2/FiO2 < 200mmHg and decision for intervention was made as shown in Figure 1. Moreover, depending on their tolerability, patients were proned. Duration and timings of positions shown in Table 1.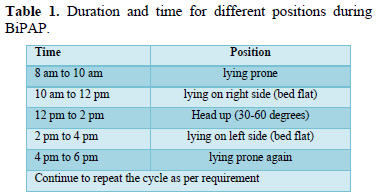
Baseline demographic data were collected (Age, Gender, BMI, Duration of symptoms). Arterial blood gas analysis was done in supine position and after prone position on BiPAP at 8:00 AM and at 8:00 pm and patients pulse rate (PR), blood pressure (BP), SpO2, respiratory rate (RR) and PaO2/FiO2 were observed.
RESULTS
Quantitative data were expressed as means ± SD in form of continuous variables with help of IBM SPSS software version 20.0 Results were analyzed by using unpaired Student’s t test or Mann-Whitney test. P values < 0.05 were considered significant. Comparison of two groups Group A (n=100) and Group B (n=100) were done and it was observed that the average age of these patients was 56.91 ± 10.02, 70% were male and 30% were females and the average BMI was 26.74 ± 2.06 in group A. In group B the average age was 58.68 ± 10.05, 78% were male and 22 % were female and average BMI was 26.60 ± 2.26. The other characteristics such as RR, SpO2 and PaO2/FiO2 on ICU admission are presented in Table 2.
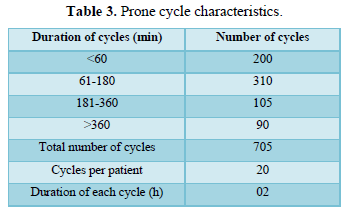
The proning duration of each cycle was 2 h so, the daily requirement is 3 cycles of 6 h. Prone cycles and duration of proning shown in Table 3. It is shown that there was significant increase in PaO2/ FiO2 in group A patients and also there was significant increase in SpO2 in group A as compared to patients in group B. There was not much difference in RR, HR, MAP, PEEP between the two groups, shown on Tables 4A and 4B. In group A 20% patients were undergone intubation whereas in group B 35% patients were intubated.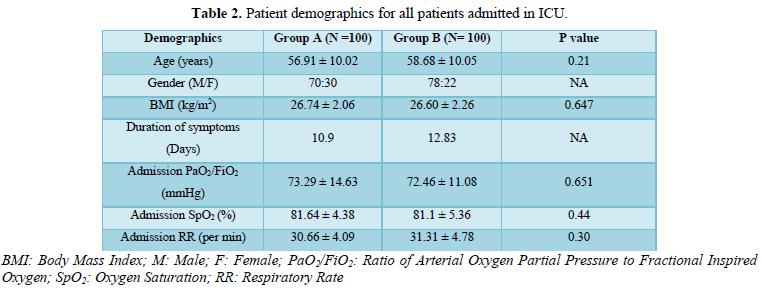
DISCUSSION
In moderate to severe ARDS timing is very critical during initial period of BiPAP with prone position. More than 50% of patient could be saved from intubation. Therefore, avoid the need for invasive ventilation. Ding [9] suggested that by adding PP, PaO2/ FIO2 ratio increased by 20-25 mmHg which was not possible in supine position. Bernard [11] has revealed 90% of death in ARDS patients. But over a period of time with development of latest technology, number of deaths were reduced [12].
In our study, 20% patients required intubation in group A as compared to 35% in group B. SpO2 was higher in group A than group B. There was improve in oxygenation in group A patients compare to group B. Late prone position to BiPAP in severe ARDS results in high risk for delayed intubation, whereas early application of PP to BiPAP in patients with moderate ARDS avoid the need for invasive ventilation. Moreover, the prone positioning has beneficial role in improving oxygenation in ARDS patients [13,14].
In our study patients on prone position actually showed an improvement in oxygenation in most cases compared to patients in supine position. PaO2/FiO2 increased significantly in group A patients than group B. When Invasive ventilation was applied to prone position patients have demand of muscle relaxant and deep sedation [15,16]. In our study awake prone position patient’s compliance was good and tolerated well. So, Hani [17] found that peripheral ground glass changes converted into linear consolidation in HRCT of COVID -19 patients. Yaqian [18] stated autopsy findings of exudation, macrophage infiltration, fibrosis and mucus plugs. So, the advantage of prone position is to drain the secretion from distal areas of the lungs.
CONCLUSION
We concluded that early application of prone position with BiPAP in COVID-19 patients with moderate to severe ARDS can improve oxygenation without any adverse effect. This also helps to avoid invasive mechanical ventilation. Further research work is required for conclusive remarks.
ACKNOWLEDGEMENT
We are thankful to Director Dr. Kirti M Patel, Dean Dr. Yogendra Modi, Medical superintendent Dr. Bharat Ghodadra, CEO Dr. Sunil Rao, Prof. Medicine Dr. Naimesh Patel, Associate Prof. Community medicine Dr. Arpit Prajapati, GCSMCH & RC, Ahmedabad, for their constant support and help.
-
Vinetz J (2020) Written by Maria Cohut, Ph.D. Novel coronavirus: Your questions, answered: Medical news today. Accessed on: October 29, 2020. Available online at: https://www.medicalnewstoday.com/articles/novel-coronavirus-your-questions-answered
-
World Health Organization (WHO) (2020) Clinical management of severe acute respiratory infection. SARI when COVID-19 disease is suspected: Interim Guidelines. Accessed on: March 13, 2020. Available online at: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf
-
Bender K (2020) Prone Position Could Allow Ventilation Without Intubation for COVID-19. Accessed on: May 3, 2020. Available online at: https://www.contagionlive.com/view/prone-position-ventilation-intubation-covid-19
-
Munshi L, Fralick M, Fan E (2020) Prone positioning in non-intubated patients with COVID-19: Raising the bar. Lancet Respir Med 8(8): 744-745.
-
Koeckerling D, Barker J, Mudalige NL, Oyefeso O, Pan D, et al. (2020) Awake prone positioning in COVID-19. Thorax 75(10): 833-834.
-
Ng Z, Tay WC, Ho CHB (2020) Awake prone positioning for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur Respir J 56(1): 2001198.
-
Damarla M, Zaeh S, Niedermeyer S, Merck S, Niranjan-Azadi A, et al. (2020) Prone Positioning of Non-Intubated Patients with COVID-19 Am J Respir Crit Care Med 202(4): 604-606.
-
Pappert D, Rossaint R, Slama V, Grüning T, Falke KJ (1994) Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest 106(5): 1511-1516.
-
Ding L, Wang L, Ma W, He H (2020) Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: A multi-center prospective cohort study. Crit Care 24: 114.
-
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al (2012) Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 307(23): 2526-2533.
-
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, et al. (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149: 818-824.
-
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, et al. (2012) The Berlin definition of ARDS: An expanded rationale, justification, and supplementary material. Intensive Care Med 38(10): 1573-1582.
-
Mancebo J, Fernández R, Blanch L, Rialp G, Gordo F, et al. (2006) A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med 173(11): 1233-1239.
-
Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, et al. (2009) Prone positioning in patients with moderate and severe acute respiratory distress syndrome: A randomized controlled trial. JAMA 302(18): 1977-1984.
-
Scholten EL, Beitler JR, Prisk GK, Malhotra A (2017) Treatment of ARDS with Prone Positioning; Chest 151(1): 215-224.
-
Guérin C, Beuret P, Constantin JM, Bellani G, Garcia-Olivares P, et al. (2018) A prospective international observational prevalence study on prone positioning of ARDS patients. Intensive Care Med 44(1): 22-37.
-
Hani C, Trieu NH, Saab I, Dangeard S, Bennani S, et al. (2020) COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagn Interv Imaging 101(5): 263-268.
-
Mao Y, Lin W, Wen J, Chen G (2020) Clinical and pathological characteristics of 2019 novel coronavirus disease (COVID-19): A systemic review. medRxiv. pp: 1-31. Available online at: https://www.medrxiv.org/content/10.1101/2020.02.20.20025601v2
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Alcoholism Clinical Research



