Review Article
Pharmacology Related to Pediatric Anesthesia
5121
Views & Citations4121
Likes & Shares
A child is not a mini adult. Each organ system is under development in pediatric age group. They differ in every way from an adult thus it is mandatory to have a basic knowledge of the pharmacokinetic and pharmacodynamics principles in pediatric population to prevent under dosing or toxicity of drugs. This review article aims to simplify the basic principles of pharmacokinetics and pharmacodynamics along with the drug interactions of commonly used drugs in anesthesia.
Keywords: Pediatric pharmacology, Pediatric anesthesia, Pharmacokinetics
Abbreviations: PK: Pharmacokinetic; PD: Pharmacodynamic; NPO: Nil Per Oral; IV: Intravenous; NMBD: Neuromuscular Blocking Drugs; GABAA: Gamma‑Amino‑Butyric‑Acid Type A; NMDA: N‑Methyl‑D‑Aspartic Acid
INTRODUCTION
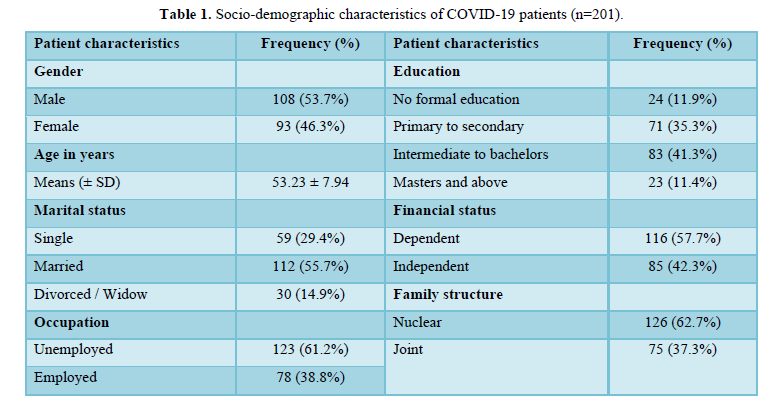
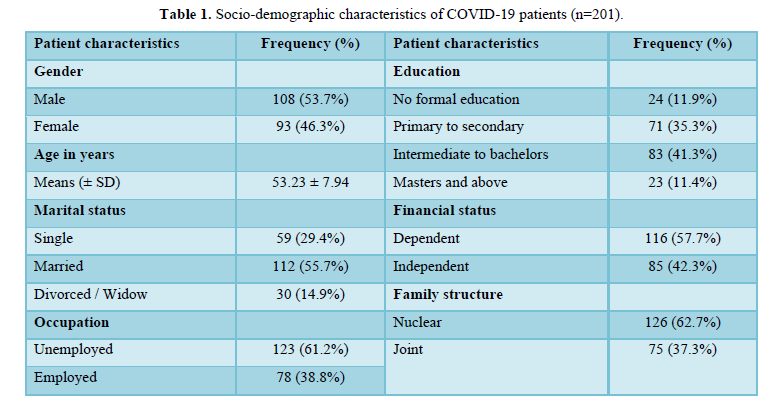
The Pharmacokinetic (PK), Pharmacodynamic (PD) and side effect profile of medications differ among adults and children. PK is affected by maturation of organ function and body composition [1]. The PD effects differ in children depending upon the capacity of end organs like brain, heart or skeletal muscle (Table 1).
Pharmacokinetics: This refers to movement of the drug in and alteration of the drug by the body; includes absorption, distribution, binding/storage, biotransformation & excretion of the drug.
Pharmacodynamics: It includes physiological & biochemical effects of drugs and their mechanism of action at organ system/subcellular levels.
Pharmacotherapeutics: It is the application of pharmacological information together with knowledge of the disease for its prevention, mitigation or cure. Selection of the most appropriate drug, dosage & duration of treatment.
PHARMACOKINETICS
Absorption
-
Oral: The efficacy of orally administered drug depends on the rate and extent of absorption from the gastrointestinal tract and physicochemical nature of the drug. The gastric pH, at birth is 6 to 8, reaches adult levels between 6 months to 3 years of age [2]. Total volume of gastric secretions is less in neonates. Decreased bile acid secretion in neonate decreases the absorption of lipid soluble drugs. Long chain fatty acids (found in neonatal formula) delay gastric emptying, and thus important while determining the NPO status of neonates before surgery.
-
Oral transmucosal drug or nasal administration: This bypasses the first pass hepatic effect and causes a rapid onset of drug action e.g., sublingual nitroglycerine, nasal midazolam, ketamine.
- Transdermal: It is hazardous in neonates as their stratum corneum is very thin with well hydrated epidermis leading to enhanced drug absorption and toxicity. However percutaneous theophylline gel has been used for the treatment of apnea in newborns.
- Parenteral: After IM administration systemic absorption of drug is more rapid and predictable than oral or rectal administration because of high density of skeletal muscle capillaries in infants than older children. Drugs injected intravenously act immediately.
- Rectal: Absorption via this route is slow and irregular and also depends on the drug form (suppositories, rectal capsules or enemas).
- Intrapulmonary: This mode is being used in infants and children e.g.: Surfactant and adrenaline.
DistributionThe drug distribution is directly related to the lipid solubility and inversely related to the protein binding. Neonates have greater proportion of body water (approx. 75%) and are called as “little bags of water”. Therefore, the volume of distribution of water-soluble drugs is higher in neonates, therefore higher initial dose required in the neonate compared to the infant, older child or adult.Neonates lack in muscle and fat content; resulting in prolonged clinical effect of the drugs like thiopentone which redistribute to muscle and fat. Immaturity of blood brain barrier in neonates also increases the risk of toxicity of otherwise lipid insoluble drugs like morphine.MetabolismLiver is the principle site of drug metabolizing enzymes. Liver function is deficient in neonates reaching adult values by one year of age and manifesting as slower rate of drug metabolism [3]. The plasma levels of albumin and other proteins necessary for binding of drugs are lower in term newborns than in older infants.ExcretionExcretion is the domain of kidneys which attain maturity by two years of age. Renal function is decreased in neonates and preterm babies due of low perfusion pressure and immature glomerular & tubular function. The ability to handle free water & soluble loads may be impaired in neonates, thus half-life of drugs excreted by kidneys will be prolonged [4]. Premature neonates often possess multiple renal defects, like decreased creatinine clearance, impaired sodium retention, glucose excretion and bicarbonate reabsorption; and poor diluting and concentrating ability [5].RELEVANCE OF PK AND PD CHANGES TO ANESTHESIADrug interactions can occur on a PK or PD level, or both. When a drug has a higher affinity for tissues other than plasma, the volume of distribution may be large. Drugs may compete for binding sites on plasma proteins (albumin and α1 acid glycoprotein), thus increasing the unbound fraction and resulting in a higher volume of distribution or drugs that decrease cardiac output may decrease the perfusion of tissues thereby altering their volume of distribution. Volatile anesthetics and opioids exhibit strong supra-additive interactions. The interaction between opioids and the IV anesthetic agents is also supra-additive. The knowledge about pharmacodynamic drug interactions can optimize anesthetic drug dose.Pharmacology of Neuromuscular JunctionThe increased sensitivity of the neuromuscular junction of the human neonate and infant to non-depolarizing neuromuscular blocking agents is the result of reduced release of ACh from immature motor nerves [6]. The relatively high volume of extracellular fluid in infants and children corresponds to an increase in the volume of distribution of NMBDs and influences dose requirements.Relaxants in ChildRecent developments like laryngeal mask airways in clinical practice have eliminated the need for muscle relaxants in pediatric anesthesia. Muscle relaxants are required for intubation and procedures requiring profound muscle relaxation. The duration of action of these doses is about the same or less than that of the standard 1 mg/kg intubating dose in adults. Increased potency is associated with greater specificity of drug action and fewer side effects.Anesthesia and the Developing BrainBrain development begins during the last trimester of intrauterine life; human brain is not fully developed at birth and continues to grow over the first couple of years of postnatal life.Prevention of ApoptosisMelatonin prevents anesthesia-induced apoptotic neuronal degeneration. Beta-estradiol protect against anesthesia-induced apoptotic cell death. L-carnitine protect neuronal cell.According to a Danish study young child exposed to a brief, single anesthetic did not show any evidence of adverse long‑term effects on the brain. Based on the work of Ikonomidou [7] it is widely accepted that the commonly used general anesthetics potentiate inhibitory transmission through gamma‑amino‑butyric‑acid type A (GABAA) receptors and the excitatory transmission is reduced through N‑methyl‑D‑aspartic acid (NMDA) glutamate receptors at the peak of synaptogenesis causing apoptotic neurodegeneration. Furthermore, based on the studies by Jevtovic-Todorovic [8] it appeared that exposure to general anesthetics at the peak of synaptogenesis causes significant learning and memory deficit later in life.CONCLUSIONAnaesthetizing the pediatric patients can be fascinating, albeit challenging, even for experienced anesthesiologists. It is evident that the pediatric population differs even amongst themselves physiologically, anatomically as well as pharmacologically depending upon their age group. It is imperative to have thorough knowledge about the pharmacological difference for each age group along with the PK and PD interactions of anesthetic drugs to prevent therapeutic misadventures. Target controlled infusions in pediatric and the neurodevelopmental outcome of anesthetic drugs is still being studied. We have tried to review the literature and articles specific to pediatric anesthesia and pharmacology briefly.
- Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, et al. (2003) Developmental pharmacology-drug disposition, action, and therapy in infants and children. N Engl J Med 349(12): 1157-1167
- Jacob R, Krishnan, Venkatesan (2004) Pharmacokinetics and Pharmacodynamics of Anesthetic drugs in Pediatrics. Indian J Anaesth 48(5): 340-346.
- Benedetti MS, Baltes EL (2003) Drug metabolism and disposition in children. Fundam Clin Pharmacol 17: 281-299.
- Anderson BJ, Holford NH (2013) Understanding dosing: children are small adults, neonates are immature children. Arch Dis Child 98(9): 737-744.
- Anker JNV (1996) Pharmacokinetics and renal function in preterm infants. Acta Paediatr 85: 1393-1399.
- Gregory GA (1994) Pharmacology. In: George A Gregory. Pediatric Anaesthesia, Churchill Livingstone, New York pp: 13-47.
- Ikonomidou C, Bittigau P, Koch C, Genz F, Hoerster F, et al. (2001) Neurotransmitters and apoptosis in the developing brain. Biochem Pharmacol 62: 401-405.
- Jevtovic-Todorovic V, Todorovic SM, Mennerick S, Powell S, Dikranian K, et al. (1998) Nitrous oxide (Laughing gas) is as NMDA antagonist, neuroprotectant and neurotoxin. Nat Med. 4: 460-463.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Oncology Clinics and Research (ISSN: 2643-055X)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- International Journal of AIDS (ISSN: 2644-3023)


