2655
Views & Citations1655
Likes & Shares
- Imaging time; as the time required viewing on a single cut
- For the PENG block: the femoral artery, the anterior inferior iliac spine, the iliopubic eminence and the psoas tendon.
- For the FIB: the femoral artery, the iliacus muscle, the fascia iliaca and the fascia lata.
- Puncture time; as the time that stretches from the introduction of the needle until the end of the injection of local
- Performance time: the imaging time + the time to
- Number of punctures: as the number of redirection of the needle after removing of 2 cm.
- VRS score at 5, 10, 15 and 20 min after the block when raising the affected limb to 15°.
- The imaging time, puncture time, performance time and the number of punctures.
- Hemodynamic status (mean blood pressure and heart rate) during surgery
- Cumulative consumption of bupivacaine.
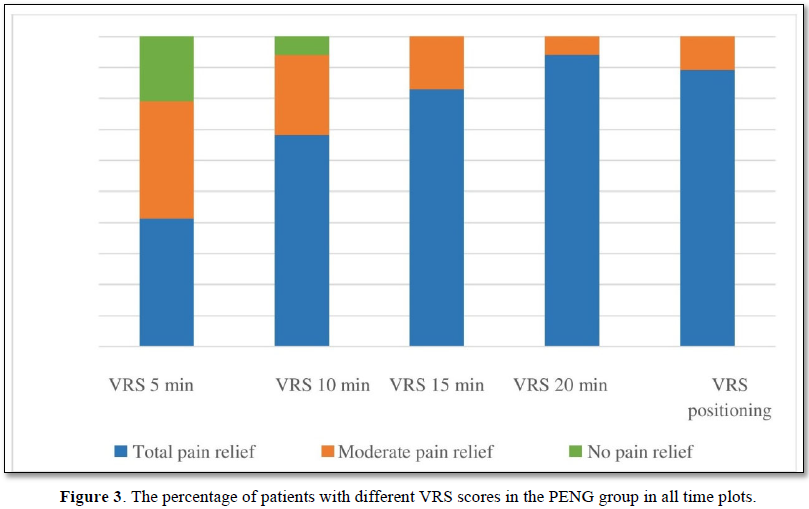
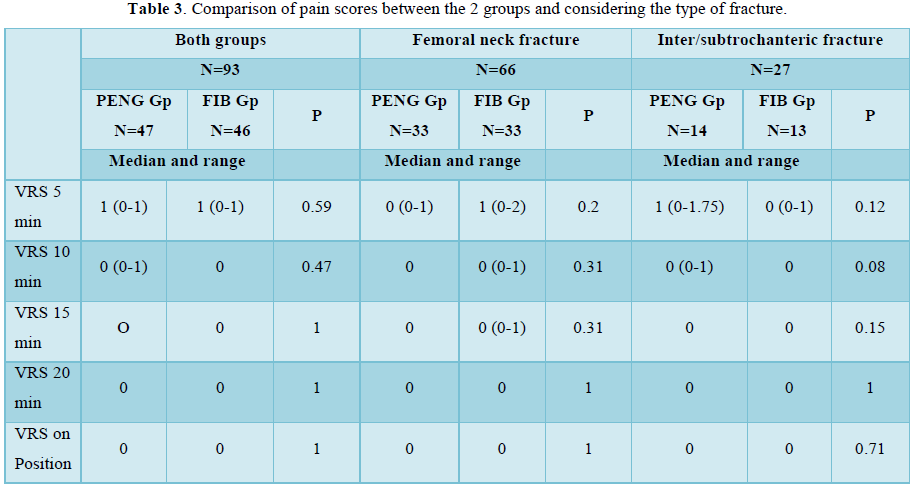
In both groups, 89% of patients had a total pain relief during positioning and more than 90% at 20 min. both blocks were efficient for all measurements and especially when positioning (Figures 2 & 3). The VRS declined significantly when compared with VRS at 5 min, for all measures and for both groups (p<0.001). No patient needed IV fentanyl. We didn’t find any difference in pain scores in all times, in all type of fractures and when positioning before SA in both groups (Table 2).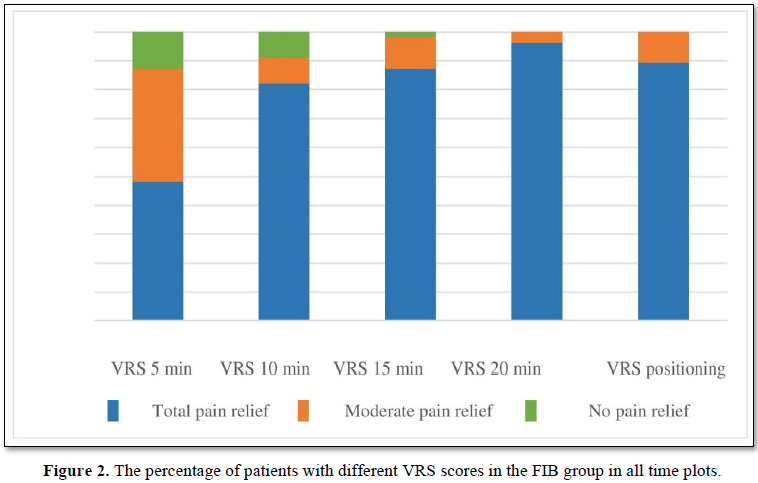
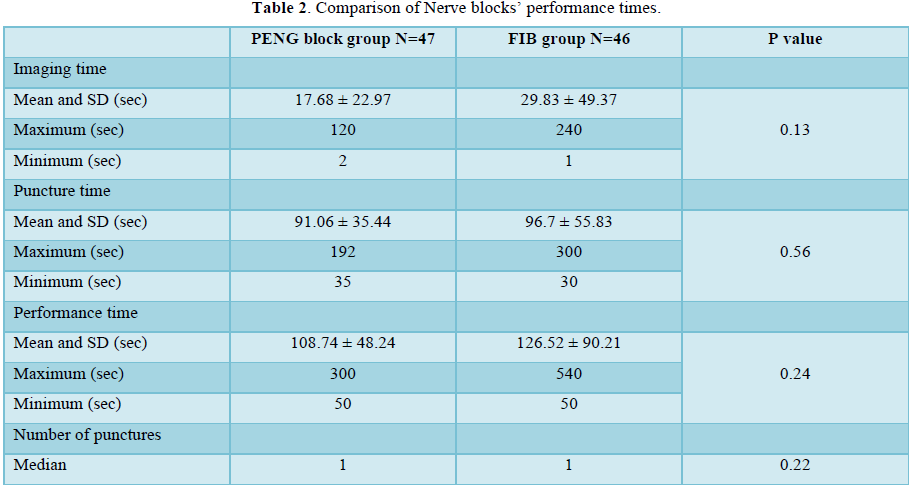
Performance time for PENG block was shorter but with no significant difference (Table 3).
Intra operative mean blood pressure and heart rate were equivalent in both groups. Total bupivacaine consumption was similar in both groups (4.76 ± 1.44 mg in PENG group vs. 4.63 ± 1.84 mg in FIB group; p=0.63). Duration of surgery was not different between groups (75.34 ± 32.25 min in PENG group vs. 80.12 ± 33.17 min in FIB group; p=0.54).
DISCUSSION
In our study both PENG block and FIB were confirmed to be efficient in providing adequate preoperative analgesia. We noted a significant decrease in pain scores at 15 min, 20 min and while positioning when compared to pain score at 5 min for both nerve blocks. However, we didn’t find any difference between the 2 blocks in pain scores in all time, in all type of fractures and even when positioning before CSA.
This study had two main limitations. First, we did not evaluate sensory dermatomal level to check the effective coverage from both blocks. Second, we didn’t assessed postoperative analgesia to evaluate any superiority of PENG block compared to FIB in the early postoperative period. But, these two limitations didn’t interfere with our main result, as no painful sitting position was reported in both groups.
Optimal sitting position is one of the prerequisites for smooth conduct of SA as the majority of hip-fracture patients experience severe pain. The femoral nerve block (FNB) and FIB are commonly used for analgesia in hip fractures. A Cochrane review evaluating nerve blockades in hip fractures has shown high quality evidence supporting a reduction in dynamic pain after either FNB or FIB [3].
The FIB is the most popular nerve block among anesthesiologists to provide immediate and postoperative analgesia in hip fractures [7,8]. It provides better quality during positioning than intravenous analgesic and was safer [9]. However, recent study failed to demonstrate any superiority of FIB to neither IV morphine nor FNB [10,11]. Literature suggests that the obturator nerve is not covered by these blocks [4]. Hip joint is richly innervated. Anatomical studies show that the anterior hip joint capsule is mainly innervated by the femoral nerve, the obturator nerve, and, inconsistently, the accessory obturator nerve [12,13]. The PENG block, described by Giron-Arango [4] is a musculofascial plane block between psoas tendon and pubic ramus targeting the articular branches of both femoral nerve and accessory obturator nerve. In a pilot study, authors found median drop of 7 points in pain score following the PENG block for hip fracture.
Cadaveric study demonstrated the diffusion of methylene blue into the anterior hip capsule when administered with PENG block [14]. Although PENG block targets these nerves that supply the hip capsule, femoral nerve block and fascia iliaca block do not target them.
First case series reported efficacy of PENG block for intra and postoperative analgesia in hip surgery with a median reduction of 4 to 7 points in preoperative NRS (numeric rate scale) [15,16]. Furthermore, PENG block provided prolonged postoperative analgesia up to 12.5 h [16]. PENG block administered prior to positioning patients for SA, showed significant drop in pain scores during active movement and a comfortable positioning during SA for most patients [5,17,18]. In our study, the PENG block provided a significant pain reduction at 20 min compared to prior to block. The sitting position was optimal for all patients.
When compared to supra inguinal FIB, PENG Block provided a significantly quicker onset of pain control in neck fracture (13.6 min vs. 22 min) but a similar duration (9.9 h in PENG block vs. 10.32 h in FIB) [19]. In Shankar [18] study, mean reduction in pain score during dynamic movement and sitting position, was significantly higher in PENG group; 7.2 ± 0.7 vs. 5 ± 0.8 in FIB group; p <0.00 [18]. Quality of patient positioning for SA was higher in group PEN, but no patient required additional IV fentanyl. Duration of block was comparable in both groups (7.85 and 8.16 h, respectively).
Similar results were reported by Jadon A [6], reduction of the NRS at rest and at movement in PENG block group was significantly higher than in the FIB group (6 and 9 to 3 and 4; 5 and 8 to 4 and 5). Patients in PENG group were significantly more comfortable than with FIB when sited (2.15 ± 0.6 vs. 1.39 ± 0.49; P < 0.0001). But, analgesic duration was equivalent in both groups (11.8 h and 11.2 h).
We failed to demonstrate any superiority of PENG Block compared to FIB during hip mobilization and sitting position. Our results were different from the literature. The study design differences were the first reason. We used a simple pain scale with only 3 points score compared to scores reported in literature. Such score is usually used in our unit to assess pain in elderly. In our study, we aimed to reduce proportion of patient with uncomfortable/failed positioning, which was more clinically relevant compared to objectives chosen in other studies. Another difference is the age of our population, who was the oldest compared to literature (81±8 years vs. 68±13 years [18]). Finally, we did not check onset time and duration of blocks in our study as all blocks were done with lidocaine.
In a recent series of 52 elderly patients with hip fracture in the emergency department, similar results to our study were reported [20]. The PENG block (19 patients) was compared to either FIB (19 patients) or FNB (14 patients). No difference in pain score reduction within 60 min between groups has been reported. Postoperative opioid use was similar between the groups. The PENG block was as effective for extracapsular proximal femur fractures compared to intracapsular fractures.
The FNB is considered as one of a standard of care for hip fractures [3]. However, it induces a motor block of the quadriceps muscle, provoking a potential delay in reeducation. A comparative observational study [21] including 42 patients, PENG block was comparable to FNB for postoperative pain control but produces less quadriceps muscle block. Postoperative muscle strength of the quadriceps in the immediate postoperative period, was greater in the PENG group than in the FNB group (5/5 vs. 2/5, p = 0.001). A recent randomized trial [22] with sixty patients, postoperative pain in the recovery room and quadriceps strength in the PENG group were better compared to FNB. The preservation of quadricipital motricity is another theorical advantage of the PENG block. Histological studies showed that nociceptive hip joint capsule fibers primarily innervate the anterior aspect of the capsule, while the nerve fibers innervating the posterior aspect of the capsule are mainly mechanoreceptors [23-25]. These findings suggest that blocking the nerves innervating the anterior capsule is the most important factor in achieving good analgesia and preserving quadriceps strength when performing PENG block. However, Yu [26] reported that 2 of over 100 patients who underwent PENG block developed motor blockade [25]. They suggested that abnormal spread of local anesthetic to motor branches of the femoral nerve could be possible when blockade is technically challenging to perform. In a cadaveric model using 20 mL of methylene blue, Tran [15] did not observe the spread pattern posterior to the articular capsule. Mistry [27], reported that the injection zone of the local anesthetic in PENG block is very important and would influence the effectiveness of the block. Optimal injection is reflected in the ultrasound vision of a medial diffusion towards the iliopubic eminence.
In our study, PENG block was easy to perform. The performance time in the PENG block group was shorter than the FIB group. In one study [27] comparing the two ultrasounds approach’s, performance time for PENG block was shorter in out-of-plane approach (53 sec. vs. 84 sec.). We used in-plane approach with a mean performance time of 108.74 ± 48.24 sec [28].
CONCLUSION
We conclude that, PENG block was as efficient as FIB in providing painless and comfortable sitting position for SA in hip surgery repair for elderly. It was easy to assimilate and perform and was also safe. More studies should be conducted to enhance our knowledge about real advantages of this new block: success rate and quadriceps muscle preservation.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
ACKNOWLEDGEMENTS
We would like to thank all the surgeons, nurses and patients who participated in the realization of this work.
TRIAL REGISTRATION
The study was registered in ClinicalTrials.gov under the number NCT 04285333.
CONFLICTING INTERESTS
The Authors declare that there is no conflict of interest.
- Abou-Setta AM, Beaupre LA, Rashiq S, Dryden DM, Hamm MP, et al. (2011) Comparative effectiveness of pain management interventions for hip fracture: A systematic review. Ann Intern Med 155: 234‑245.
- Safety ACo, Care QiH (2016) Hip Fracture Care: Clinical Care Standard. Australian Commission on Safety & Quality in Health Care pp: 2.
- Guay J, Parker MJ, Griffiths R, Kopp S (2017) Peripheral nerve blocks for hip Cochrane Database Syst Rev 5: CD001159.
- Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A (2018) Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med 43: 859‑863.
- Jadon A, Sinha N, Chakraborty S, Singh B, Agrawal A (2020) Pericapsular nerve group (PENG) block: A feasibility study of landmark based technique. Indian J Anaesth 64: 710-713.
- Jadon A, Sinha N, Chakraborty S, Singh B, Agrawal A (2021) Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anesthesia: A randomized double-blinded trial. Indian J Anaesth 65: 572-578.
- Amin NH, West JA, Farmer T, Basmajian HG (2017) Nerve blocks in the geriatric patient with hip fracture: A review of the current literature and relevant Geriatr Orthop Surg Rehabil 8: 268‑275.
- Wennberg P, Norlin R, Herlitz J, Sarenmalm EK, Möller M (2019) Pre-operative pain management with nerve block in patients with hip fractures: A randomized, controlled trial. Int J Orthop Trauma Nurs 33: 35-43.
- Hsu YP, Hsu CW, Bai CH, Cheng SW, Chen C (2018) Fascia iliaca compartment block versus intravenous analgesic for positioning of femur fracture patients before a spinal block: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 97: e13502.
- Pasquier M, Taffé P, Hugli O, Borens O, Kirkham KR et al. (2019) Fascia iliaca block in the emergency department for hip fracture: a randomized, controlled, double-blind trial. BMC Geriatrics 19: 180.
- Zhou Y, Zhang W-C, Chong H, Xi Y, Zheng S-Q, et al. (2019) A Prospective Study to Compare Analgesia from Femoral Obturator Nerve Block with Fascia Iliaca Compartment Block for Acute Preoperative Pain in Elderly Patients with Hip Fracture. Med Sci Monit 25: 8562-8570.
- Swenson JD, Davis JJ, Stream JO, Crim JR, Burks RT (2015) Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: The pattern of distribution and effects on the obturator J Clin Anesth 27: 652‑627.
- Short AJ, Barnett JJG, Gofeld M, Baig E, Lam K, et al. (2018) Anatomic study of innervation of the anterior hip capsule: Implication for image guided intervention. Reg Anesth Pain Med 43: 186-192.
- Tran J, Agur A, Peng P (2019) Letter to the editor. Is pericapsular nerve group (PENG) block a true pericapsular block? Reg Anesth Pain Med 44: 257.
- Pagano T, Scarpato F, Chicone G, Carbone D, Bussemi CB, et al. (2019) Analgesic evaluation of ultrasound-guided Pericapsular Nerve Group (PENG) block for emergency hip surgery in fragile patients: A case series. Arthroplasty 1: 18.
- Brown B, Lin D-Y, Saies A, Vermeulen M, Kroon HM, et al. (2021) The Pericapsular Nerve Group Block for Hip Fracture Surgery: A Prospective Case Report J Anesth Clin Res 12: 999.
- Acharya U, Lamsal R (2020) Pericapsular Nerve Group Block: An Excellent Option for Analgesia for Positional Pain in Hip Fractures. Case Rep Anesthesiol 2020: 1830136.
- Shankar K, Rangalakshmi S, Ashwin AB, Nandini U, Chandra M, et al. (2020) Comparative Study of Ultrasound Guided PENG [Pericapsular Nerve Group] Block and FIB [Fascia Iliaca Block] for Positioning and Postoperative Analgesia Prior to Spinal Anesthesia for Hip Surgeries: Prospective Randomized Comparative Clinical Study. Indian J Anesth Analg 7: 798-803.
- Bhattacharya A, Bhatti T, Haldar M (2019) Pericapsular nerve group block - Is it better than the rest for pain relief in fracture neck of femur? Reg Anesth Pain Med 44: A116.
- Fahey A (2021) Pericapsular nerve group block for hip fracture is safe and effective in the emergency department: A prospective observational study comparing pericapsular nerve group block to fascia iliaca compartment block and femoral nerve block.
- Allard C, Pardo E, De la Jonquière C, Wynieck A, Soulier A, et al. (2021) Comparison between femoral block and PENG block in femoral neck fractures: A cohort study. PLoS One 16: e0252716.
- Lin D-Y, Morrison C, Brown B, Saies AA, Pawar R, et al. (2021) Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: A single-center double-blinded randomized comparative trial. Reg Anesth Pain Med 46: 398-403.
- Tomlinson J, Zwirner J, Ondruschka B, Prietzel T, Hammer N (2020) Innervation of the hip joint capsular complex: A systematic review of histological and immunohistochemical studies and their clinical implications for contemporary treatment strategies in total hip arthroplasty. PLoS One 15: e0229128.
- Yu HC, Moser JJ, Chu AY, Montgomery SH, Brown N, et al. (2019) Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg Anesth Pain Med 44: 611-613.
- Mistry T, Sonawane KB (2019) Gray zone of pericapsular nerve group (PENG) block. J Clin Anesth 58: 123-124.
- Lopez‑Lopez D, Reza PC, Vazquez MG, Garcia PD (2021) PENG block: Advantages of out‑of‑plane approach. Indian J Anaesth 65: 563-564.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Spine Diseases
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- International Journal of AIDS (ISSN: 2644-3023)




