Research Article
Brain Trauma Injury Secondary to Fall from Tree: Epidemiological and Therapeutic Aspects
5302
Views & Citations4302
Likes & Shares
Introduction: The increase in cases of child falling from tree in our structure and the lack of data on this subject in the literature led us to initiate this work. Our objective was to describe the epidemiological, therapeutic and evolutionary aspects of this condition in our hospital.
Material and Methods: Our longitudinal and descriptive study was conducted from January to December 2019 in the neurosurgery department of Gabriel Touré university hospital in Bamako. It had concerned patients aged 0 to 18 years treated for head trauma secondary to a fall from tree height. Head injuries caused by other mechanisms were excluded from this study. Patient follow-up lasted 6 months. A total of 72 patients were identified.
Results: Childhood head trauma secondary to a fall from tree accounted for 59.5% of children with head trauma, with a predominance of boy (94.5%). The mango tree was implicated in 89%. Direct cause of fall was found in 15.3% of cases. On admission, 5 patients were in coma. Mild disturbance in alertness was present in 41.7% of cases. Motor deficit was observed in 33 patients (45.8%). Head CT had showed depressed skull fracture associated with brain contusion in most cases (50% of cases). A craniocerebral wound was found in 2 patients. Surgery was performed in 57% of patients. After 6 months of follow-up, 11 patients were lost to follow-up and 48.2% had a neurological disorder. Mortality was 4.2%.
Conclusion: Head trauma from falling from tree is one of the causes of disability in children in developing countries. Early and adequate management could reduce mortality.
Keywords: Fall from tree, Child, Head trauma
INTRODUCTION
Traumatic head injury is the leading cause of disability linked to neurological disorders in children in neurosurgical environments in Mali. Road accidents are the leading cause of traumatic head injury at Gabriel Touré University hospital in Bamako [1]. The increase in cases of traumatic head injury in children by falling from tree height and the lack of data on this subject led us to initiate this work. Our objective was to describe epidemiological, therapeutic and evolutionary aspects of this affection in the Neurosurgery department of Gabriel Touré university hospital in Bamako.
MATERIALS AND METHODS
We carried out a longitudinal and descriptive study over a period of 12-month from January 1 to December 31, 2019 in the Neurosurgery Department of Gabriel Touré University Hospital in Bamako. It concerned patients aged 0 to 18 years treated for traumatic head injury secondary to a fall from tree height. Patients over 18 years of age and patients who had head injuries due to mechanisms other than tree fall were excluded from the study. After discharge from hospital, patients were seen in outpatient at three (03) weeks then monthly for 3 months and at the sixth month after the trauma. Epidemiological, clinical and therapeutic data as well as the evolution were studied. A total of 72 patients were collected.
RESULTS
Epidemiological aspects
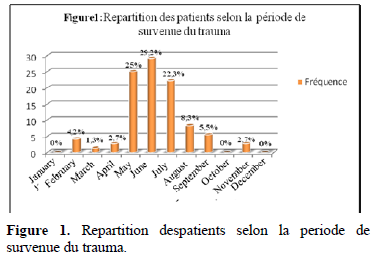
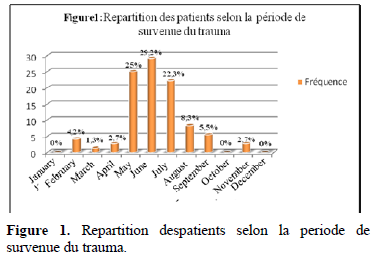
Between January 1 and December 31, 2019, 904 patients were treated for neurosurgical pathologies, including 530 cases of head trauma of all ages; which represented a frequency of 58.6%. Head trauma had been affected 121 children, or 22.8% of cases, including 72 cases related to a fall from tree. This had represented 59.5% of children with head injuries. Head injuries from falling a tree had accounted for 13.6% of all head injuries of all ages. This condition had affected boys in 94.5% of cases. The average age of our study population was 13.5 years with extremes of 10 and 17 years. These were students in 39% of cases, farmers in 23.6%, young unemployed and apprentice in 22.2% and 15.3% respectively. The trauma had occurred in rural and peri-urban areas in 70.8% of cases (51 patients). Mango tree was implicated in 89% (64 patients) and non-fruit trees in 8 patients. The direct cause of the fall was a broken branch in 11 patients (15.3%). In the others, this cause was undetermined. The frequency of the trauma was highest in May, June and July (Figure 1).
Clinical aspects
Headache was the clinical symptom found in all patients. Thirty-eight patients (52.8%) had lost consciousness immediately after falling from the tree. When they arrived at the hospital, 5 patients were in coma (7% of the cases) and 30 had moderate alertness disorder (41.7% of the cases). Thirty-seven children had normal state of consciousness (Table 1). Motor deficit was observed in 33 patients, i.e., 45.8% of cases. It was hemiparesis in 54.5% of cases (18 patients) and monoparesis in 27.3% of cases (9 patients). Monoparesis was crural in 6 patients and brachial in 3 others. Hemiplegia and monoplegia accounted for 12% (4 cases) and 3% (1 case), respectively. One patient had tetraparesis. Eleven patients had phasic disorder like Wernicke's aphasia in 7 cases and Broca's aphasia in 4 cases. Frontal syndrome was found in 21 patients (29.2% of cases). Nine patients had presented psychomotor agitation (12.5% of cases). Three patients had generalized tonic-clonic seizure, 4.2% of the cases. Twenty-one patients (29.2%) had associated lesions. These were divided between limb trauma 17 cases, lumbar spine trauma without neurological disorders (3 cases) and one case of cervical trauma.
Table 1. Distribution of patients by state of consciousness upon arrival at the hospital.
|
Glasgow Score |
Number |
Frequency (%) |
|
15 |
37 |
51,4 |
|
12-14 |
17 |
23,6 |
|
9-11 |
13 |
18 |
|
≤ 8 |
5 |
7 |
Radiological aspects
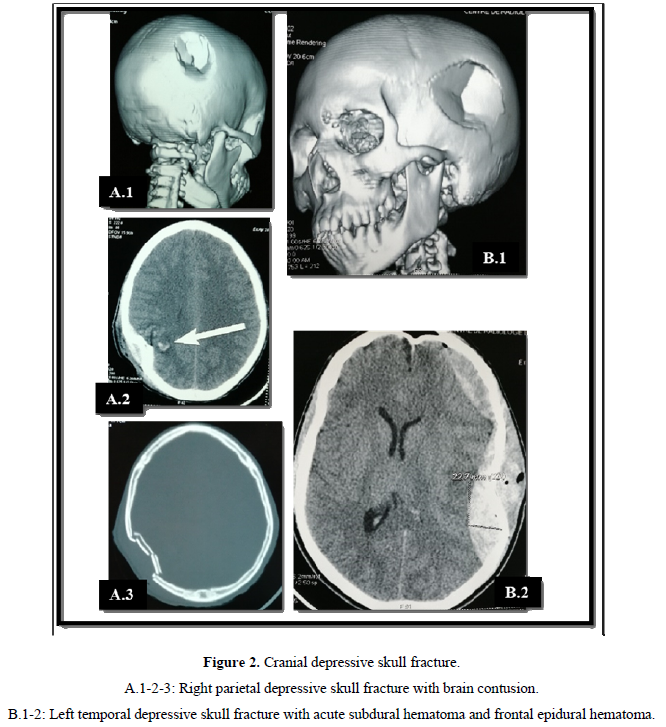
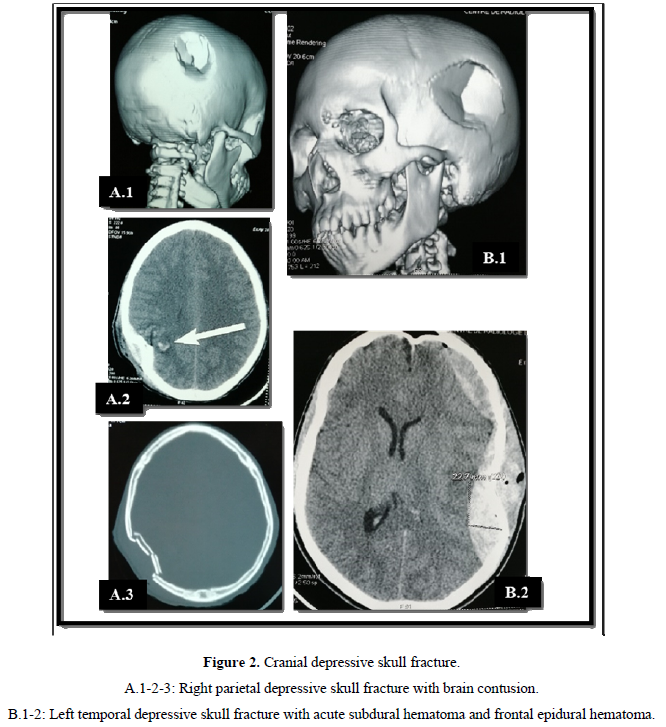
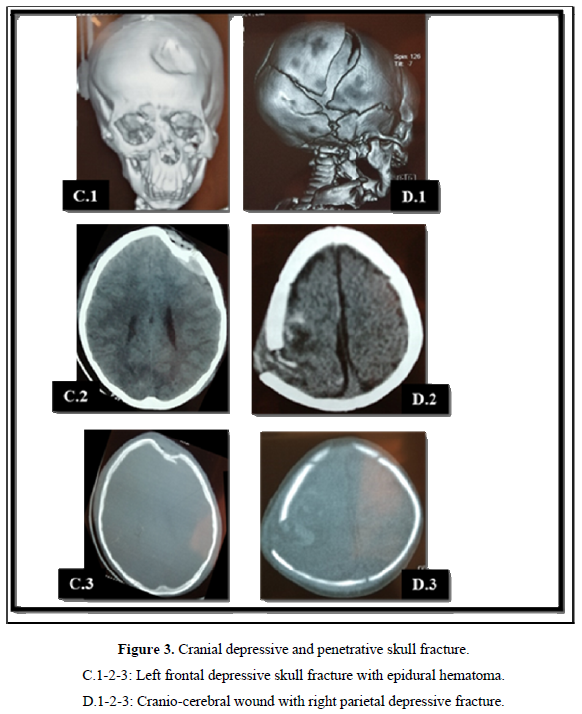
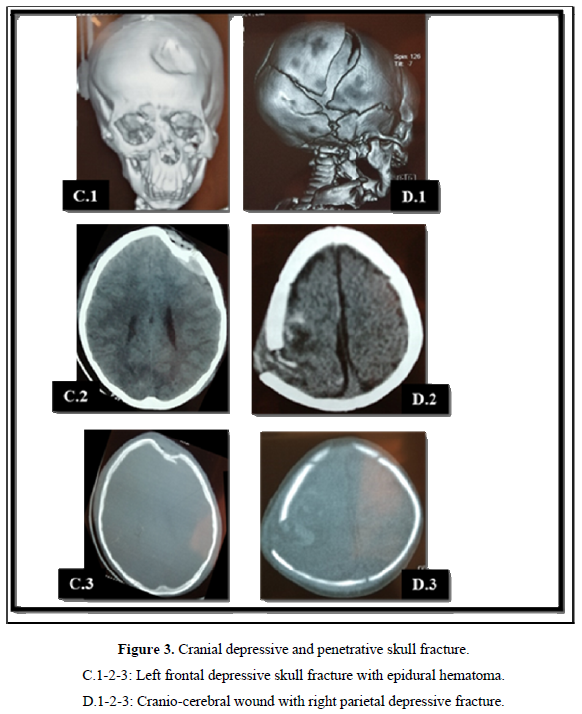
Computed tomography (CT) was the exam of choice for diagnosing lesions. It was performed in all patients and had made it possible to highlight a depressed skull fracture in 45 patients (62.5% of the cases) (Figure 2). These depressed skull fractures were isolated in 7 patients (15.6% of cases). They were associated with brain contusions in 36 cases (80%) Figure 2A and acute subdural hematoma in 2 patients (4.4%) Figure 2B. Isolated brain contusion was diagnosed in 18 patients (25%). Extradural hematoma (Figure 3C) and craniocerebral wound (Figure 3C) each accounted for 2.7% (2 cases). In 5 patients (7%), the CT scan was normal.
Therapeutic aspects
Exclusive medical treatment had been undertaken in 31 patients, or 43.1% of cases. It was based on symptomatic treatment. Five children had been admitted to intensive care for coma. Chlorpromazine had been administered to 9 patients who exhibited psychomotor agitation. It was administered intravenously. Osmotherapy using mannitol at dose of 100 ml every 6 hours for 24 h was performed in 6 patients. They had presented intracranial hypertension syndrome with significant brain contusion and subfalcine herniation on CT scan. For the 3 patients who had had epileptic seizures, intravenous clonazepam had been used to treat emergency seizures in combination with valproic acid as a background treatment over a period of 6 months. Surgery was indicated in 41 patients (57%). It consisted of performing a lifting of depressed skull fracture in 31 patients. There were 5 cases of isolated depressed skull fracture and 26 patients with depressed skull fracture associated with underlying brain contusion. A decompressive craniectomy with feeding of the flap was
performed in 5 patients for major intracranial hypertension. Evacuation of acute subdural hematoma was performed in 2 patients. Surgery for extradural hematoma was performed in one patient.
EVOLUTION
The average length of hospital stay was 10 days with extremes of 3 and 23 days. Operative complications had concerned 3 patients. These were surgical site infections in 2 cases and brain abscesses in one patient. Outcome was favorable in 28 patients with mild headaches and the absence of neurological disorders, i.e., 39% of cases. Three patients had died during hospitalization, i.e., 4.2% of cases. On discharge from hospital, motor deficit persisted in 25 patients (34.7% of cases). They left with hemiparesis in 14 cases, monoparesis in 6 cases, hemiplegia and monoplegia in 4 and 1 case respectively. Nine patients were aphasic (12.5% of cases) including 7 cases of Wernicke's aphasia. Mental confusion persisted in 7 patients (9.7%) with 4 cases of psychomotor agitation under Levomepromazine. At 6 months, 11 patients were lost from sight (16% of cases). Outcome was good in 27 patients (45.5%) with an absence of neurological disorder. Motor deficit persisted in 19 patients (32.7%). Aphasia affected 6 patients (10.3%). Mental confusion and agitation continued in 3 patients each (5.2%).
DISCUSSION
Head injury from falling from tree is the second leading cause of head injury in children. The first cause being accidents on the public highway [1]. Trauma from falling from tree remains very little reported [2,3]. These are pathologies frequently encountered in hospitals in developing countries [4]. As for head trauma from falling from a tree, the literature is very poor. It had represented 32.5% of cases of trauma by falling from a tree in Burkina Faso [5]. We did not find data in the literature about this subject in children. In our cohort, the male predominance was 94.5%, made up mostly of students and young farmers. In our context, the great precariousness in rural areas leads young boy to take risks in order to contribute to the functioning of the family unit. These risks include collecting and searching for firewood. These activities are done in traditional way by climbing trees. The direct cause of the fall was found in only 15.3% of our patients. It was a broken shank. In the study carried out by Djientcheu [4], the causes were diverse and variable. They were distributed among others in sliding (36.8%), broken branch support (17.5%), misstep (3.5%), percussion of the climber by a cut branch and the poor appreciation of the jump from one branch to another. The main motivation of the climber in our series was looking for fruits, which partly explained the fact that the mango tree is the most incriminated tree and the predominance of these accidents in May, June and July (mango season). This has been reported by several authors from different countries [4-6]. Forty-eight-point six percent of the patients in our series had had disturbance of consciousness, including 7% of coma. Motor deficit was observed in 45.8% of cases and phasic disorders were found in 7 patients. Neurological disorders manifested by impaired state of consciousness and motor deficits reflected moderate to severe brain damage. Height of the fall, surprise effect and quality of the landing on the ground are factors that determine the severity of the lesions found in patients. CT scan has been the defining diagnostic test for brain damage in our patients. It had made it possible to highlight fractures of the cranial vault (62.5%) associated with endocranial lesions in 80% of cases. CT scan is an excellent first-line diagnostic exam in our countries given its availability, accessibility and speed of its performance. The management of brain contusion injuries constituted the mainstay of the treatment of the patients in our series. It was based on symptomatic treatment. Osmotherapy is best indicated for post-traumatic brain oedema. It had participated in the reduction of intracranial pressure. Among the 41 patients operated on, 8 had had endocranial lesions which required surgical approach other than lifting of depressed skull fracture. These were decompressive craniectomy (5 cases), evacuation of acute subdural hematoma (2 cases) and that of an extradural hematoma (1 case) by cranial flap. Two thirds of the postoperative complications were infections of the surgical site of the feeding of the craniectomy flap. The absence of organ bank in our country leads us to keep the craniectomy bone subcutaneously at the level of the right iliac fossa. This lengthens the operating time and would increase the risk of infection. After 6-month of follow-up, 48.2% of the children had had neurological disorder. This had a significant impact on the socio-economic level of the community. The absence of reintegration program in our states means that these neurological disorders will constitute a handicap leading most of these children to drop out of school. The mortality rate was 4.2% in our cohort. In 2005, in Cameroon, 4 out of 5 patients which had had head trauma secondary to a fall from tree had died [4]. Earlier adequate care could reduce the death rate.
CONCLUSION
Falling from tree height is a common occurrence in developing countries. It constitutes one of the serious causes of disabled children in these countries. There are certain factors that determine the severity of brain damage. Early and adequate management could reduce mortality. Raising awareness and fighting poverty are essential in preventing these accidents.
- Diallo M, Faye M, Cissé MA, Sogoba Y, Djibo D, et al. (2019) Epidemiological and surgical aspects of brain trauma injury of the child: Experience of the Gabriel Touré University Hospital Center, Bamako, Mali. Neuro Neurosurg 1: 1-5.
- Adeloye A (1989) Neurosurgery in Africa. Ibadan University Press, pp: 253-271.
- Kraus JF (1985) Epidemiological aspect of spinal cord injury: A review of incidence, prevalence, causes and outcome. In Central nervous system trauma status report, edited by Dp Decker and J Povlishock. National Institute of Health, pp: 313-25.
- Djientcheu VP, Djamen PG, Njamnshi AK, Zogo PO, Etoundi AG (2005) Traumatismes secondaires à la chute du haut d’un arbre. AJNS 24: 107-109.
- Kiendrebeogo S (2012) Les traumatismes par chute du haut d’un arbre aux urgences traumatologiques du CHU-YO de Ouagadougou: Aspects épidémiologiques, anatomopathologiques, thérapeutiques et évolutifs. Thèse Méd. UFR/SDS, Université de Ouagadougou N 103
- Ngaro SB (1975) Lochouarn P, Kounetkov P. Pathologie du manguier en République Centrafricaine. Méd Afr Noire 22: 633-639.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- International Journal of Diabetes (ISSN: 2644-3031)





