Research Article
Scrub Typhus Case from Myanmar Complicated by Bilateral Frontoparietal Cortical Infarcts
4459
Views & Citations3459
Likes & Shares
A previously healthy 69-year-old agricultural man presented with prolonged fever, thrombocytopenia, acute hepatitis, acute kidney failure and acute bilateral fronto-parietal cortical infarcts. Screening tests for common systemic infections which can cause such multisystem involvement such as malaria, leptospirosis was negative. There was no eschar, rash or lymphadenopathy. Although being locally unavailable, rickettsia serology was finally sent to overseas laboratory and scrub typhus serology turned out to be positive. He significantly improved after intravenous azithromycin. At one-month after treatment initiation, he was completely back to normal. Here we report a case of scrub typhus in a resource-poor setting of Myanmar complicated with acute cerebral infarction which was not commonly reported.
Keywords: Scrub typhus, Cerebral infarct, Myanmar.
INTRODUCTION
Scrub typhus (ST) caused by Orientia tsutsugamushi, transmitted by trombiculid mites (chigger’s bite), is endemic in tsutsugamushi triangle in the Asia-Pacific area. Mortality can be as high as 30% without proper treatment [1]. It infects endothelial cells affecting all organs [2]. There is a wide spectrum of neurological manifestations, among which meningoencephalitis is classical [3]. Stroke cases mainly intracranial hemorrhage [4] were reported and acute cerebral infarct is one of the less common complications of ST.
CASE PRESENTATION
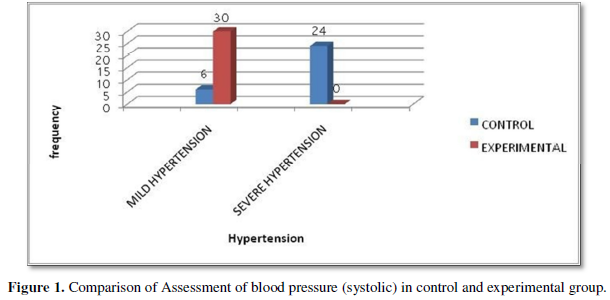
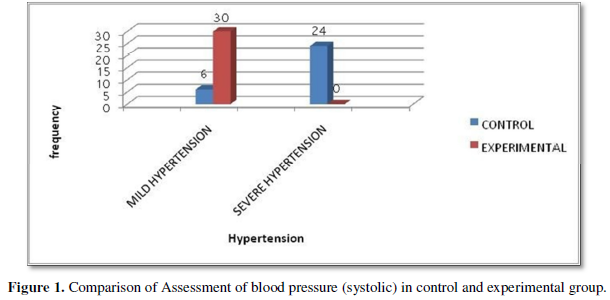
A 69-year-old man, an agricultural worker lived in a village near Pyay town in Bago Province, a non-drinker and non-smoker, was admitted to Sakura hospital with one-month prolonged fever, five days of jaundice, and three days of anuria, confusion and weakness of all four limbs. There was no history of seizures, headache and vomiting before. Fever was high up to 40°C, remittent, not associated with chills and rigors, rash, cough, dysuria, diarrhea or abdominal pain. He was already treated at local clinics and hospital with various antibiotics but referred to our hospital after a month because of persistent fever and worsening general condition with confusion. His past medical history was unremarkable. No febrile illness reported in the family. On examination, he had fever, conjunctival edema, pallor, jaundice, Glasgow Coma scale (GCS) 11 (E3V3M5), with stable vitals. There was no meningism, no cranial neuropathy but he had hypertonia and hyperreflexia with bilateral extensor plantar responses. Other systemic examination was normal except mild hepatomegaly. No eschar, rash or lymphadenopathy were noted. ECG and chest X-ray were unremarkable. Baseline blood tests on admission showed random blood sugar 429 mg%, hemoglobin 5.8 g/dL, WBC 25.88 x 109/L, absolute neutrophil 86.8%, lymphocyte 10.2%, platelet count 63 x 109/L, erythrocyte sedimentation rate 35 mm/1st hour, C reactive protein 80.89 mg/L, creatinine 804umol/L, urea 430 mmol/L, sodium 177mmol/L, potassium 5.6mmol/L, chloride 145mmol/L, bicarbonate 12.3mmol/L, serum bilirubin 44.46umol/L, alkaline phosphatase 122 U/L, ALT 195 U/L and AST 175 U/L, gamma GT 128 U/L, HbA1c 5.7%. serum amylase 126.6, PT 12.7 seconds, INR 1.08, APTT 28.4 seconds, D-dimer 3711.6 ng/mL, fibrinogen 7520 mg/dL. Widal test, malaria blood film, dengue and Chikungunya serology, leptospiral serology, HIV, HBs antigen, anti-HCV antibodies, Quantiferon-TB Gold plus ELIZA and syphilitic screening were all negative. Stool and urine routine examination were normal. Urine, sputum and blood cultures were sterile. Abdominal ultrasound showed acute hepatitis with splenomegaly. Echocardiogram did not reveal any vegetation. Non-contrast CT (Head) scan was normal. Electroencephalography showed mild diffuse encephalopathy with diffuse theta slowing at bilateral frontoparietal regions without clinical or electrographic seizures. MRI showed gyri form pattern of restricted diffusions without susceptibility consistent with acute bilateral frontoparietal cortical infarcts (Figure 1).
MRA revealed normal major intracranial arteries and MRV was normal. Cerebrospinal fluid study was normal. Differential diagnoses on admission were Weil’s disease or severe falciparum malaria. He was treated with insulin, hydration, correction of electrolyte imbalance, anti-malaria treatment and various empirical antibiotics including intravenous ceftriaxone, levofloxacin, vancomycin, piperacillin/tazobactam and metronidazole for persistent high fever. Finally, his fever subsided after intravenous azithromycin for five days. Rickettsia serology (indirect fluorescent antibody test) was sent late to overseas laboratory after 6 weeks from onset of fever and scrub typhus serology turned out to be positive with IgM 1:800, IgG 1:400 while murine and tick typhus serologies were negative. His neurological status returned back to normal completely with normal blood parameters including platelet count, renal and liver functions in 4 weeks after initiation of azithromycin.
DISCUSSION
We presented a case of ST that was diagnosed late, besides suffered from acute ischemic small vessel infarcts and multiorgan failure, and recovered after treatment without sequelae. While diagnosis is to be based on history of exposure, clinical features and serological test, it was late in current case because of absence of eschar, which is a necrotic skin lesion at the site of a chigger mite bite, and low index of clinical suspicion by attending doctors. Although being endemic, ST is not as well-known as malaria, typhoid, dengue and leptospirosis in our country, the reason for which might be poor awareness due to lack of local diagnostic facilities and few published studies and case reports from Myanmar on it. In 1947, Davis GE first documented about ST in Myanmar [5]. Thailand published studies on ST cases at Thai-Myanmar border 2003 and 2017 [6,7]. Japan published a case with ST imported from Myanmar in 2009 [8]. There was a case report on two Indian soldiers who contracted ST after travel to Indo Myanmar border in 2015 [9]. In 2020, first Myanmar group led by Win did serologic and molecular surveillance on clinically suspected ST cases in Sagging and Magway Provinces (central Myanmar) and affirmed genetic heterogeneity and endemicity of ST in Myanmar [10]. Recently Elders et al studied seroprevalence at various parts of Myanmar and concluded that the widespread distribution of rickettsioses in Myanmar was particularly high in central and northern regions [11]. However, our case was from Bago province in Southern Myanmar. Apart from above few studies, there were scarce literature and reports of ST from Myanmar [1]. Our case agrees with the findings of the 14-year study in Laos on spatial and temporal distributions of ST, which concluded that ST is more common in rural area, and visiting rice fields and forests with surface flooding and high vegetation density poses higher risk of getting it [12]. Wilairatana [13] reviewed that malaria and scrub typhus co-infection was high in endemic areas such as India (8%) and Thailand (35%) among febrile patients. However, malaria tests (blood film and ICT) were negative in our case so co-infection was unlikely although both are undeniably endemic in Myanmar [13]. There has been no case report on its CNS sequelae in Myanmar yet. Ischemic stroke complication was reported only in few cases, presenting with both small vessel [14,15] and large vessel infarcts [16]. Pathogenesis of bilateral cortical infarcts in the presence of normal INR and APTT and normal MRA in our case can be explained by widespread cerebrovascular endothelial dysfunction and vasculitis in small vessels due to direct invasion of endothelium by rickettsia, which is the main pathologic findings described in ST cases [1]. Our case is also in accordance with previous case reports where stroke complicated cases were those who received delayed effective antibiotics after onset [16]. Although being life-threatening with severe hepatorenal failure in addition to multiple infarcts, our case, on receiving appropriate antibiotics which was inexpensive and easily available, fully recovered. So, it is essential to have high index of clinical suspicion and to establish easily accessible testing facility since ST is not susceptible to routinely and empirically used β-lactam-based regimens. In conclusion, ST should be one of the differentials not to be overlooked in febrile patients from rural areas of Myanmar.
CONFLICT OF INTEREST
None.
CONSENT
Written informed consent was obtained from the patient’s family.
- Xu G, Walker DH, Jupiter D, Peter CM, Christine MA (2017) A review of the global epidemiology of scrub typhus. PLoS Negl Trop Dis 11(11): e0006062.
- Moron CG, Popov VL, Feng HM, Wear D, Walker DH (2001) Identification of the target cells of Orientia tsutsugamushi in human cases of scrub typhus. Mod Pathol 14(8): 752-759.
- Mahajan SK, Mahajan SK (2017) Neuropsychiatric Manifestations of Scrub Typhus. J Neurosci Rural Pract 8(3): 421-426.
- Kotwal M, Vaish E, Gupta KK, Ozair A (2020) Scrub typhus manifesting with intracerebral hemorrhage: Case report and review of literature. J Family Med Prim Care 9: 2535-2537.
- Davis GE, Austrian RC, Bell EJ (1947) Observations on tsutsugamushi disease (scrub typhus) in Assam and Burma: the recovery of strains of Rickettsia orientalis. Am J Hyg 46: 268-286.
- Parola P, Miller RS, McDaniel P, Telford SR, Rolain MJ, et al. (2003) Emerging rickettsioses of the Thai-Myanmar border. Emerg Infect Dis 9: 592-595.
- Brummaier T, Kittitrakul C, Choovichian V, Lawpoolsri, Wattanagoon Y, et al. (2017) Clinical manifestations and treatment outcomes of scrub typhus in a rural health care facility on the Thailand-Myanmar border. J Infect Dev Ctries 11: 407-413.
- Matsumura Y, Shimizu T (2009) Case of imported scrub typhus contracted in Myanmar. Kansenshogaku Zasshi 83(3): 256-260.
- Biradar C, Rama S, Nizami A, Asif I (2015) Soldiers from Indo-Myanmar border presenting with scrub typhus: case report. IOSR J. Dental Med. Sci 14: 123-127.
- Win AM, Nguyen YTH, Kim Y, Ha NY, Kang JG, et al (2020) Genotypic heterogeneity of Orientia tsutsugamushi in scrub typhus patients and thrombocytopenia syndrome co-infection, Myanmar. Emerg Infect Dis 26: 1878-18881.
- Elders PND, Swe MMM, Phyo AP, Alistair RDM, Kyaw S, et al (2021) Serological evidence indicates widespread distribution of rickettsioses in Myanmar. J Infect Dis 103: 494-501.
- Roberts T, Parker DM, Bulterys PL, Rattanavong S, Elliott I, et al. (2021) A spatio-temporal analysis of scrub typhus and murine typhus in Laos; implications from changing landscapes and climate. PLoS Negl Trop Dis 15(8): e0009685.
- Wilairatana P, Kuraeiad S, Rattaprasert P, Manas K (2021) Prevalence of malaria and scrub typhus co-infection in febrile patients: A systematic review and meta-analysis. Parasites Vectors 14: 471.
- Kim JH, Lee SA, Ahn TB, Yoon SS, Park KC, et al. (2008) Polyneuropathy and cerebral infarction complicating scrub typhus. J Clin Neurol 4: 36-39.
- Chowdhury S, Mukherjee R, Sinha PK (2020) Novel occurrence of Acute Ischaemic Stroke and DVT simultaneously in a patient of Scrub Typhus: A case report. Asi J Med Sci 11(4).
- Chung JH, Yun NR, Kim DM, Lee WJ, Win SK, et al. (2013) Scrub typhus and cerebrovascular injury: A phenomenon of delayed treatment? Am J Trop Med Hyg 89(1): 119-122.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Pathology and Toxicology Research
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)



