Research Article
ANXIETY, DEPRESSION, AND SLEEP QUALITY DURING THE COVID-19 PANDEMIC
4453
Views & Citations3453
Likes & Shares
Purpose: This study aimed to determine the extent to which anxiety and depression were associated with sleep quality in college students, and if there were gender differences in the three variables.
Methods: The participants were 1292 college students (Meanage=21.5 years, SD=2.6 years); 67.4% female, 30.9% male). Participants completed a survey including the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), and the Sleep Assessment Questionnaire.
Results: The results indicated that higher anxiety and depression significantly predicted lower sleep quality (F=161.23, p=.000), accounting for 35.3% of the total variance. Further, the poor sleep quality group scored significantly higher in anxiety (F=117.59, p=.000) and depression (F=188.72, p=.000) while controlling for gender. Concerning gender differences, female participants scored significantly higher than the male participants in anxiety (t=-8.57, df= 787.83, p=.000), depression (t=-6.78, df=784.9, p=.000) and poor sleep quality (t=-7.23, df= 775.92, p=.000).
Conclusions: College students with higher levels of anxiety and depression symptoms had lower levels of sleep quality compared to students with lower levels of these symptoms. Females showed significantly higher depression and anxiety levels, and lower sleep quality than males. This study is one of the first to explore US college student depression, anxiety, and sleep quality relationships during a pandemic.
Key words: Depression, Anxiety, Sleep quality, College Students, Mental health
INTRODUCTION
Recently, there has been a great emphasis on identifying and treating mental health issues, with certain subsets of the United States (US) population experiencing higher rates and severity of conditions such as depression and anxiety. In particular, attention has been turned toward the college student population to better determine prevalence of mental health disorder, successful treatment options, and treatment accessibility (Eisenberg, et al., 2007; Pedrelli, et al., 2015). A recent study surveyed the state of US college student mental health and showed around 31% of the participating students experienced persistent symptoms of depression, such as sadness (Toscos, et al., 2018). A review comparing college student mental health status from 2007 to 2018 found that the depression rate has increased, with 41.1% and 21.1% of the total 788,235 students surveyed displaying moderate and severe depressive symptoms, respectively (Duffy, et al., 2019). The same review discovered that the anxiety symptom rate in 2018 was 34.4% and 11.7% respectively for moderate and severe anxiety classification (Duffy, et al., 2019).
It has been well-documented that mental health conditions, such as depression and anxiety, are correlated with decreased quality of sleep (Alkhatatbeh, et al., 2020; Breslau et al., 1996; Fang, et al., 2019; Franzen & Buysse, 2008; Horváth et al., 2016; Nutt et al., 2008; Oh, et al., 2019). Research has shown that traits of poor sleep quality, like insomnia, are symptoms of both anxiety and depression in adult populations (Mayers, et al., 2009; Ramsawh, et al., 2009), young adult populations (Breslau et al., 1996), and adolescents (Ramsawh, et al., 2009), in turn, reducing overall quality of life (Ramsawh, et al., 2009).
With the onset of the Coronavirus pandemic, many people have had to make drastic accommodations in their social and physical activities to follow government restrictions and safety protocols. Overall, young adults have been found to be receptive and adherent to protocols (Ravert, et al., 2021). The impact that these restrictions has had on quality of life has been explored in countries such as Italy. A study by (Marelli, et al.,2021) examined the impact of the Italian-implemented March-to-May lockdown on sleep and psychological distress. The results showed that the students had experienced worsened sleep quality at the end of the lockdown. Of these participants, 40% reported experiencing insomnia symptoms by May, up from 24% in March. They also experienced high rates of depression and anxiety post-lockdown, at 27.8% and 34.3% respectively (Marelli, et al., 2021). The researchers suggested that the increase in stress experienced by students during the Coronavirus pandemic had negatively affected their sleep quality and mental health.
Other nations have also investigated college students’ mental health and sleep quality during the current pandemic. A recent cross-sectional study by (Xie, et al. 2021). examined the prevalence of depressive symptoms, poor diet, and poor sleep quality in medical students at Kunming Medical University in China in the beginnings of the Coronavirus pandemic. They found an increase in depression and poor sleep quality in the total sample, with a higher rate of depression found in males compared to females (Xie, et al., 2021). In similar study on Chinese college students, results indicated that students had high levels of anxiety and increased sleep issues (Wang, et al., 2020).
With the changes in public health regulations and in lifestyle being so recent, few studies have explored the influence of the coronavirus pandemic on mental health and sleep quality. Additionally, very few studies have examined the influence of mid-pandemic anxiety or depression on sleep quality in a US college student population, making it necessary to investigate this relationship further. Thus, the purpose of the study is twofold: (a) determining mid-pandemic depression and anxiety levels, and sleep quality in college students, and any gender differences in these variables; (b) examining the extent to which anxiety and depressive symptoms are associated with sleep quality in college students, and any gender differences in this relationship. Based on previous research findings, it was hypothesized that the anxiety and depression levels amongst college students would be relatively high, and that sleep quality would be relatively low due to increased stress associated with the pandemic. Concerning the associations between anxiety and depression symptoms and sleep quality, it was hypothesized that these variables would show a direct association, as has been found in previous studies (Alkhatatbeh, et al., 2020; Breslau, et al., 1996; Fang, et al., 2019; Franzen & Buysse, 2008; Horváth, et al., 2016; Nutt, et al., 2008; Oh, et al., 2019). Based on previous findings, it was expected that female students would display higher rates of depression, anxiety, and poor sleep quality relative to male students (Duffy, et al., 2019; Toscos, et al., 2018). Through understanding the current state of college student mental health and sleep quality, the impact of a pandemic-specific environment on quality of life can be established.
METHODS
Research Participants and Setting
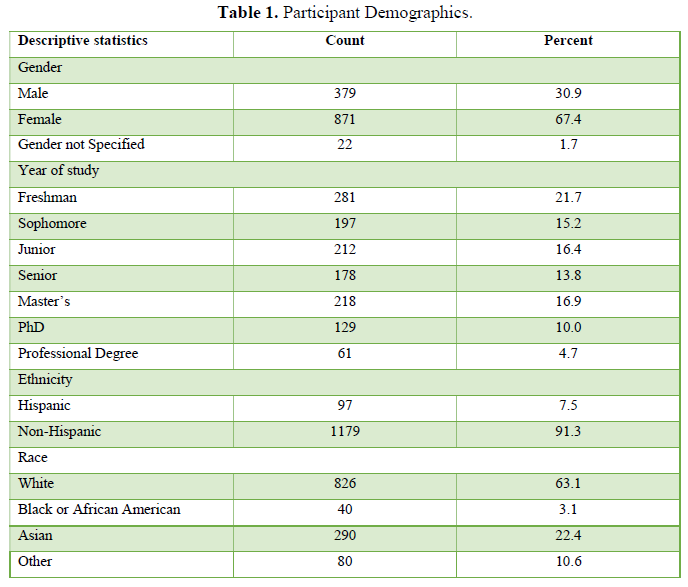
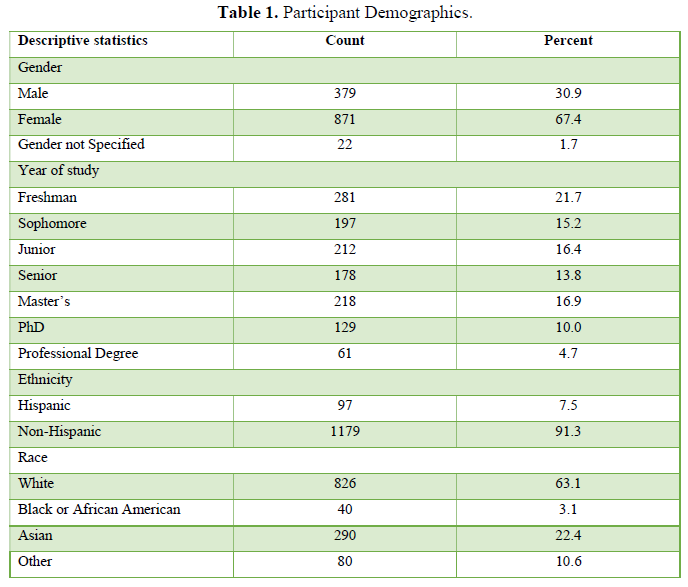
A total of 1292 undergraduate and graduate students (67.4% female, 30.9% male, 1.7% gender not specified) from a large public Midwestern university voluntarily participated in this study. The mean age was 21.5 (SD=2.6 years) and 68% were undergraduate students. The summary of demographic information is displayed in Table 1. Participants were recruited through the University’s targeted email response system, the university’s Canvas Learning Management Platform, undergraduate and graduate bulletins, and social media. An incentive of a $25 Amazon gift card was raffled off to thirty-one participants. The study (HUM00189120) protocols were approved by the University Institutional Review Board (IRB) of Health and Behavioral Sciences. Participants provided written consent prior to taking the survey.
DATA COLLECTION
The participants were asked to anonymously complete an online Qualtrics survey within 10 days during the fall semester of 2020 in the midst of the COVID-19 Pandemic. The online survey consists of three questionnaires measuring anxiety, depression, and sleep quality.
Anxiety measure
The 7-item Generalized Anxiety Disorder Scale (GAD-7) by Spitzer et al. (2006) was used in this study for participants to self-rate their anxiety symptoms. The GAD-7 questionnaire measures anxiety symptoms occurring within the past two weeks on a scale from 0 (not at all) to 3 (nearly every day). Answering “more than half the days” or “nearly every day” on four or more questions was classified as having moderate anxiety. Answering “more than half the days” or “nearly every day” on five or more questions was categorized as having moderately severe anxiety. The 7 items were summed to receive a total anxiety score. The score for this questionnaire ranged from 0 to 21. The GAD-7 has proved to be a reliable scale for measuring anxiety with high internal consistency (α=.92) (Spitzer, et al., 2006).
Depressive symptoms measure
The 9-item Patient Health Questionnaire (PHQ-9) by Kroenke et al. (2001) was used in this study for participants to self-rate their depression symptoms. The PHQ-9 questionnaire measures depression symptoms occurring within the past two weeks on a scale from 0 (not at all) to 3 (nearly every day). Answering “more than half the days” or “nearly every day” on four or more questions was classified as having moderate depression. Answering “more than half the days” or “nearly every day” on five or more questions was categorized as having moderately severe depression. The 9 items were summed to receive a total depression score. The score for this questionnaire ranged from 0-27. The PHQ-9 has proved to be a reliable scale for measuring depression with high internal consistency ( =.89) (Kroenke, et al., 2001).
Sleep quality measure
The 6-item Sleep Assessment Questionnaire created by the Depression Center at Michigan Medicine (Sleep Assessment Questionnaire, 2018) was used in this study for participants to self-rate their sleep quality. It is a self-reported questionnaire to measure the amount and quality of sleep over the past 2 weeks. Examples of the types of questions asked are “how many hours did you sleep per night on average” and “what was your usual sleep quality.” The total score is calculated by adding the numbers of four questions with numeric answers. A score of 0-10 displays no indication of significant sleep problems. A score of 11-25 indicates that sleep needs to be observed as a potential problem and/or an aggravating factor in treatment that may require additional attention. A score ≥ 26 shows evidence of sleep problems that should be addressed.
DATA ANALYSIS
To examine the current status of anxiety, depression, and sleep quality among the participants, descriptive statistics of each study variable were calculated for the total sample, male group, and female group. Independent sample t-tests (Welch’s test was chosen due to unequal variance) were performed to examine if there was any significant difference in each of the study variable between the male and female groups. Multiple regression models were conducted to determine the extent to which anxiety and depression were associated with sleep quality the total sample, the male group, and the female group. To further examine if there is a difference in anxiety and depression among three sleep quality groups for the total sample, the male group, and the female group, MANOVA was performed, followed by post-hoc comparison performed for the three groups separately. The three sleep quality groups were categorized based on the criteria of the sleep quality measure. Participants whose sleep scores falling within 0-10 were in the “high” sleep quality group; those with sleep scores falling in the range of 10-25 were in the “medium” group; those with sleep scores being ≥ 26 were in the “poor” sleep group. All statistical analysis were performed using IBM SPSS 27. A significance level of p < .05 was set for all statistical methods.
RESULTS
Current Status Anxiety, Depression and Sleep Quality
Table 2 presents the means and standard deviations of the anxiety, depression, and sleep quality for the total sample, followed by scores for males and females.
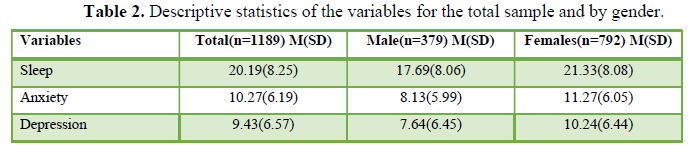
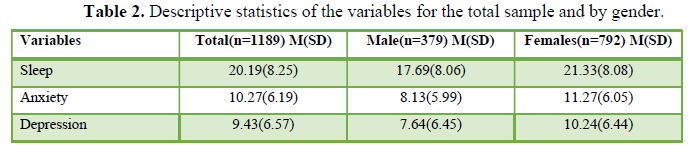
According to the population norms of the GAD-7 total score, a range of scores from 5-10 represents mild anxiety, while scores ranging from 10-14 indicate moderate anxiety (Spitzer et al., 2006). Both the total sample and the female group’s total mean scores were in the range of moderate anxiety (10-14). The male group’s mean total score was in the range of mild anxiety (5-10). With respect to depression, according to the population norms of the PHQ-9 total score, scores above 10 are considered to be in the depressive area (Kroenke et al., 2001). For the PHQ-9, a range of scores from 5-9 represents mild depression, while scores ranging from 10-14 indicate moderate depression (Kroenke et al., 2001). The female group scored within the range of moderate depression (10-14), and the male group scored within the range of mild depression (5-9). The total sample scored between the mild and moderate range cut-off points with a mean of 9.43. According to the Sleep Assessment Questionnaire total scoring, a score range of 0-10 indicates high sleep quality, a score range of 11-25 indicates moderate sleep quality, and a score above 26 qualifies as low sleep quality with the highest level of sleep issues (Sleep Assessment Questionnaire, 2018). The mean total sample scores, male mean total score, and female mean total score all fell within the range for moderate sleep quality.
The Welch’s t-test revealed significant differences in anxiety, depression, and sleep quality between the male and female groups. For anxiety, depression and sleep quality, a lower score indicated a lower presence of each condition. The female group scored significantly higher than the male group in anxiety (t=-8.57, df= 787.83, p=.000), depression (t=-6.78, df=784.9, p=.000) and sleep quality (t=-7.23, df= 775.92, p=.000).
Association of Anxiety and Depressive Symptoms with Sleep Quality
Table 3 presents the results of the multiple linear regression models with anxiety and depressive symptoms predicting the sleep quality for the total sample.
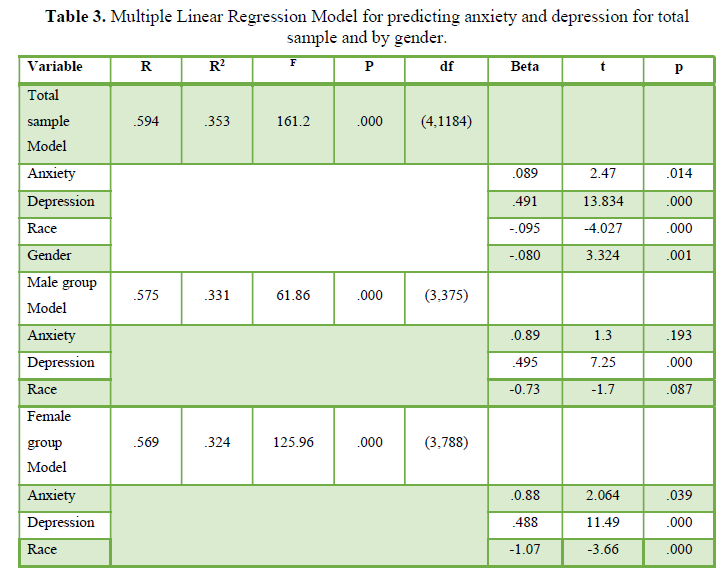
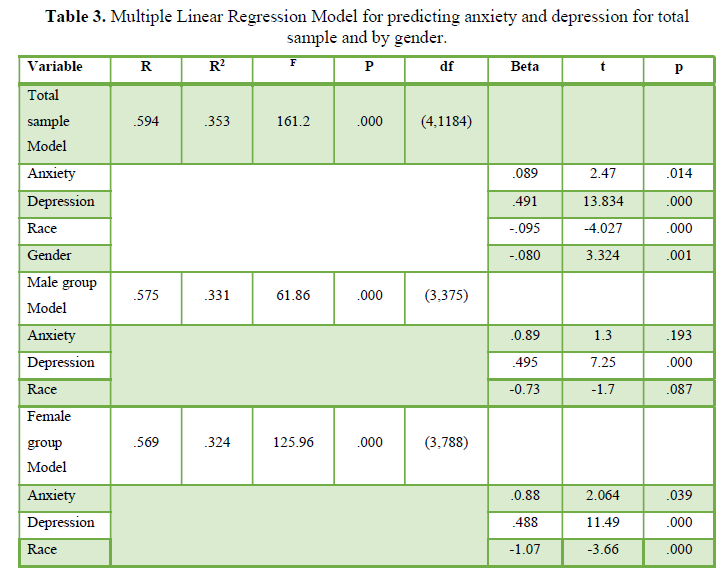
When accounting for covariates, there was a significant effect for race (p=.000) and for gender (p=.001). For the total sample, the results showed that high anxiety and depression significantly predicted poor sleep quality, accounting for 35.3% of the total variance in the sleep quality. Similarly, the results of the linear regression model indicated that anxiety and depressive symptoms significantly predicted the sleep quality for the male and female groups, explaining 33.1% of the total variance in male group and 32.4% of the total variance of in female group. When accounting for covariates, there was a significant effect for race in the female group (p=.000). For the total sample, the results of the standardized coefficient indicated that race (β=-.095, t=-4.027, p-.000), gender (β=.080, t=3.324, p-.001), anxiety (β=.089, t=2.470, p-.014), and depression (β=.491, t=713.834, p-.000) acted as stand-alone predictors of sleep quality. In the male group, the results of the standardized coefficient indicated that depression was a stand-alone predictor of sleep quality (β=.495, t=7.252, p-.000). For the female group, the results of the standardized coefficient indicated that anxiety (β=.008, t=2.064, p=.039), depression (β=.488, t=11.49, p=.000), and race (β=-.107, t=-3.66, p=.000) were all stand-alone predictors of sleep quality.
Difference in Anxiety and Depressive Symptoms among the High, Medium, and Poor Sleep Quality for the Total Sample and By Gender
For the total sample, the mean scores of anxieties and depression among high, medium, and poor sleep quality groups were presented in Figure 1.
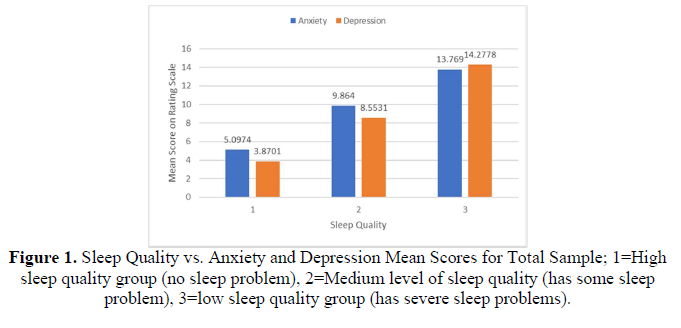
The results of the ANCOVA analysis with controlling for gender showed significant group effects on anxiety (F=117.59, p=.000, η2=.157) and depression (F=188,72, p=.000, η2= .23). Further, the post hoc comparisons indicated that the poor sleep quality group scored significantly higher in anxiety and depression than the medium and high sleep quality groups (p=.000). The medium sleep quality group scored significantly higher in anxiety and depression than the high sleep quality group (p=.000). Further, the mean scores of anxieties and depression among high, medium and poor sleep quality groups for males was shown in Figure 2 and females in Figure 3.
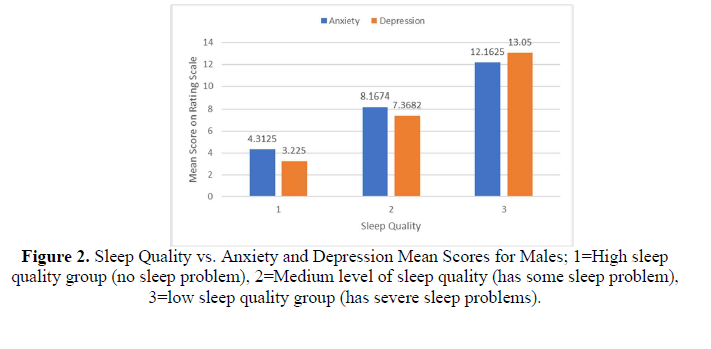
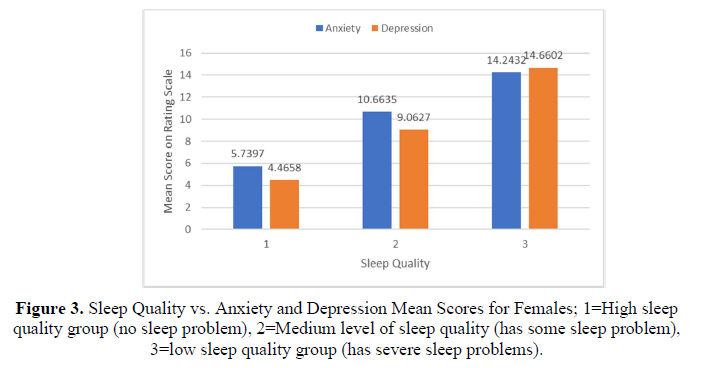
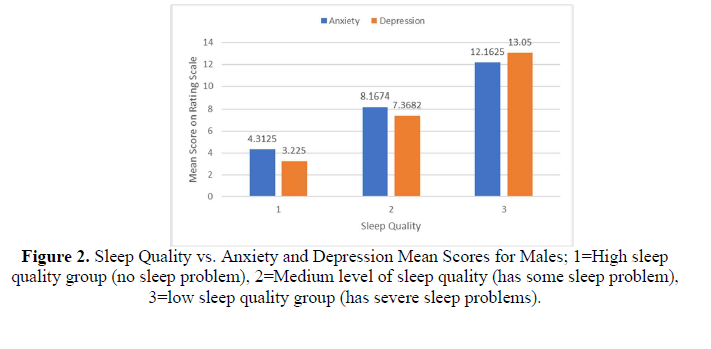
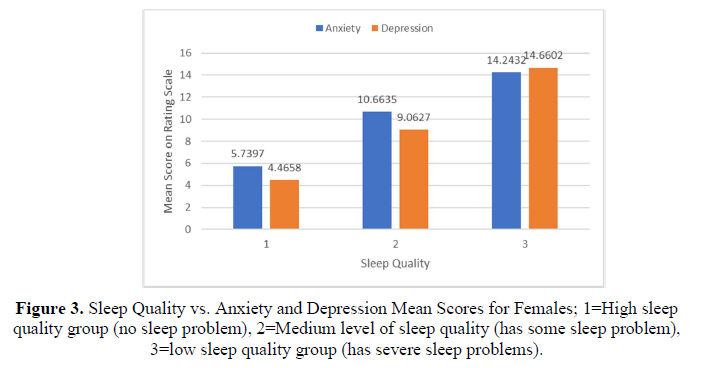
For males, the results of ANOVA revealed a significant group effect on the anxiety (F=41.349, p=.000, η2=.173) and depression (F=61.52, p=.000, η2=.237). Further, the post hoc comparisons indicated that the male poor sleep quality group scored significantly higher for anxiety and depression than the high and medium sleep quality groups (p=.000). Additionally, the male medium sleep quality group scored significantly higher for anxiety and depression than the high sleep quality group (p=.000). For females, the results of ANOVA indicated a significant group effect on anxiety (F=75.846, p=.000, η2=.151) and depression (F=125.67, p=.000, η2=.227). Further, the post hoc comparisons showed that the female poor sleep quality scored significantly higher for anxiety and depression than the high and medium sleep quality groups (p=.000). The female medium sleep quality group scored significantly higher for anxiety and depression than the high sleep quality group (p=.000).
DISCUSSION
This study was central to examining the anxiety, depression, and sleep quality levels and the relationship of these variables in US college students during the Coronavirus pandemic. Supporting the first hypothesis, students’ anxiety, depression, and poor sleep quality were relatively high. The results showed that, overall, the students experienced a moderate level of anxiety and had a low-moderate level of depression. On average, the students suffered from a moderate level of potential sleep problems. Compared to mental health research on college students conducted prior to the onset of the COVID-19, results from this study reflect a heightened prevalence of anxiety and depression in the examined population (Duffy, et al., 2019; Toscos, et al., 2018).
Previous mental health and sleep quality studies in a collegiate population during the Coronavirus pandemic have supported our study findings (Charles et al., 2021; Marelli et al., 2021; Wang et al., 2020; Xie et al., 2021). Consistent with our results, the Italian lockdown study reported that students were experiencing decreased sleep quality and increased mental health problems due to the unprecedented stress of the pandemic as a primary causal factor (Marelli et al., 2021). Studies conducted on Chinese college students also found an increase in depression and anxiety prevalence, as well as decreased sleep quality (Wang et al., 2020; Xie et al., 2021). A study from (Charles, et al. (2021). examined the level of mood disorder symptoms, perceived stress, and alcohol use in US college students during the rise of the Coronavirus pandemic. The study found that anxiety and depression showed an increase above pre-pandemic levels, indicating that concerns about the pandemic impacted the variables (Charles et al., 2021).
Supporting the second research hypothesis, our study showed that increased anxiety and depression symptoms were significantly related to poor quality of sleep across both female and male students. Specifically, we found that the students who suffered from the poorest sleep quality experienced the highest levels of anxiety and depression. These findings are supported by results from previous, similar studies (Becker et al., 2018; Schneiderman et al., 2005). Several studies have determined that a range of sleep issues, such as insomnia, often manifest as symptoms of depression and anxiety (Baglioni et al., 2016; Moshe et al., 2021; Riemann et al., 2020). The correlation between sleep quality and mental health status has possibly strengthened due to increased life stress from the ongoing pandemic. The results of a recent study showed an association between heightened stress levels and higher rates of mental health disorder, suggesting that pandemic-related stress may have affected mental health deterioration (Karyotaki et al., 2020). A different study found that adults have suffered increases in anxiety, depression, and poor sleep quality in relation to increased pandemic-related stress (Janati Idrissi et al., 2020). Research conducted prior to the Coronavirus pandemic found that college students experienced higher rates of mental health issues due to stress that stems from attending college (Balaji et al., 2019; Pedrelli, et al., 2015) in addition to other sources of stress, such as financial crises (Van Droogenbroeck et al., 2018). The additional lifestyle stress of navigating a mid-pandemic world likely could have contributed to the marked increase in mental health severity and sleep disorder in US college students.
Finally, as expected, this study found gender differences in the three variables. The results indicated that females experienced significantly poorer sleep quality and increased levels of anxiety and depression symptoms compared to males, which are consistent with previous studies (Baglioni et al., 2016; Becker et al., 2018; Duffy, et al., 2019; Moshe et al., 2021; Riemann et al., 2020; Toscos, et al., 2018). One study suggested that the higher rates of mental health disorder in females may stem from reporting bias, as male college students are less likely to seek professional assistance with mental health issues than females (Toscos, et al., 2018). A study by Van (Droogenbroeck, et al.,2018). found that young adults tend to experience a great degree of mental health disorder severity, with a lower amount of social support being associated with a higher degree of mental health issues, especially in females (Van Droogenbroeck et al., 2018). As concern over the Coronavirus pandemic has led to decreased in-person social contact (Marelli et al., 2021), social support has diminished, potentially affecting mental health. Inconsistent with our study results, (Xie, et al.,2021). found that males experienced a greater degree of depressive symptoms than females. These results may have differed from ours due to differences based on location, as the (Xie, et al. 2021). study examined medical students in China only.
This study was not without its limitations. One limitation involved the self-reported nature of the study, as the variables were all measured via survey. The self-reporting of these variables could have influenced participants’ bias to respond with greater emphasis on reporting lower anxiety, depression, and sleep quality. Additionally, due to the cross-sectional nature of the study, it was not possible to control for confounding variables. However, the variance in this study suggested that mental health status had influenced the participants’ sleep quality to a relatively high degree despite the lack of controlling for other factors. Another potential limiting factor came from the disproportionate involvement of females over males (67.4% of the participants identified as female compared to 30.9% for males). Future research on this topic could focus on more evenly recruiting between the two genders, and accounting for non-binary gender effects as well. Finally, all means of participating in this study were exclusive to an online environment. This could have inadvertently excluded possible participants that lacked access to online services, thus potentially limiting the scope of the sample that participated.
ACKNOWLEDGMENTS
We would like to thank the students who participated in this study during this unpredictable year. We extend our special thanks to Dan Burgess, MSISM, University of Michigan (O of M), ITS Teaching and Learning Service Owner for Learning Management; Zhen Qian, Teaching and Learning Application Develop Manager, and Catherine Crouch, Business Systems Analyst, Teaching and Learning Development, U of M for their helping recruit the participants for our study using Canvas.
CONCLUSION
This study showed that college students’ anxiety symptoms, depression symptoms, and poor sleep quality were at a moderate level on average in the midst of the Coronavirus pandemic, with female students being affected to a greater degree across all three variables than male students. Additionally, the association between increased mental health symptom severity and decreased sleep quality has shown to be significant across both genders. Future research should focus on exploring effective interventions to resolve increased mental health and poor sleep problems in a college student population. Colleges could use this study and other research on the topic of mid-pandemic mental health and sleep quality to conduct further investigations into the best methods of improving student quality of life.
- Alkhatatbeh, M., Abdul-Razzak, K., & Khwaileh, H.N. (2020). Poor sleep quality among young adults: The role of anxiety depression, musculoskeletal pain, and low dietary calcium intake. Perspectives in psychiatric care 57(1):117-128.
- Baglioni, C., Nanovska, S., Regen, W., Spiegelhalder, K., Feige, B., et al. (2016). Sleep and mental disorders A meta-analysis of polysomnographic research. Psychological bulletin 142(9), 969-990.
- Balaji, N.K., Murthy, P.S., Kumar, D.N., & Chaudhury, S. (2019). Perceived stress anxiety and coping states in medical and engineering students during examinations. Industrial psychiatry journal 28(1), 86-97.
- Becker, S.P., Jarrett, M.A., Luebbe, A.M., Garner, A.A., Burns, G.L., et al. (2018). Sleep in a large multi university sample of college students sleep problem prevalence sex differences and mental health correlates. Sleep health 4(2), 174-181.
- Breslau, N., Roth, T., Rosenthal, L., & Andreski, P. (1996). Sleep disturbance and psychiatric disorders a longitudinal epidemiological study of young adults. Biological psychiatry 39(6), 411-418.
- Charles, N.E., Strong, S.J., Burns, L.C., Bullerjahn, M.R., & Serafine, K.M. (2021). Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry research 296, 113706.
- Duffy, M.E., Twenge, J.M., & Joiner, T.E. (2019). Trends in Mood and Anxiety Symptoms and Suicide-Related Outcomes Among U.S. Undergraduates, Evidence from Two National Surveys. Journal Adolesc Health 65(5), 590-598.
- Eisenberg D., Golberstein E., & Gollust S.E. (2007). Help seeking and access to mental health care in a university student population. Med Care 45(7), 594-601.
- Fang, H., Tu, S., Sheng, J., & Shao, A. (2019). Depression in sleep disturbance A review on a bidirectional relationship mechanisms and treatment. Journal of cellular and molecular medicine 23(4), 2324-2332.
- Franzen, P.L., & Buysse, D.J. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues in clinical neuroscience 10(4), 473-481.
- Horváth, A., Montana, X., Lanquart, J.P., Hubain, P., Szűcs, A., et. al. (2016). Effects of state and trait anxiety on sleep structure A polysomnographic study in 1083 subjects. Psychiatry research 244, 279-283.
- Janati Idrissi, A., Lamkaddem, A., Benouajjit, A., Ben El Bouaazzaoui, M., ElHouari, F., et al. (2020). Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep medicine 74, 248-253.
- Karyotaki, E., Cuijpers, P., Albor, Y., Alonso, J., Auerbach, R.P., et.al. (2020). Sources of Stress and Their Associations with Mental Disorders Among College Students: Results of the World Health Organization World Mental Health Surveys International College Student Initiative. Frontiers in psychology 11, 1759.
- Kroenke, K., Spitzer, R.L., & Williams, J.B.W. (2001). The PHQ9 validity of a brief depression severity measure Journal of General Internal Medicine 16(9), 606-613.
- Marelli, S., Castelnuovo, A., Somma, A., Castronovo, V., Mombelli, S., et al. (2021). Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of neurology 268(1), 8-15.
- Mayers, A.G., Grabau, E.A., Campbell, C., & Baldwin, D.S. (2009). Subjective sleep depression and anxiety inter relationships in a non-clinical sample. Human psychopharmacology 24(6), 495-501.
- Moshe, I., Terhorst, Y., Opoku Asare, K., Sander, L.B., Ferreira, D., et al. (2021). Predicting Symptoms of Depression and Anxiety Using Smartphone and Wearable Data. Frontiers in psychiatry 12, 625247.
- Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in clinical neuroscience 10(3), 329-336.
- Oh, C.M., Kim, H.Y., Na, H.K., Cho, K.H., & Chu, M.K. (2019). The Effect of Anxiety and Depression on Sleep Quality of Individuals with High Risk for Insomnia A Population Based Study. Frontiers in neurology, 10, 849.
- Pedrelli, P., Nyer, M., Yeung, A., Zulauf, C., & Wilens, T. (2015) College Students: Mental Health Problems and Treatment Considerations. Acad Psychiatry, 39(5), 503-511.
- Ramsawh, H.J., Stein, M.B., Belik, S., Jacobi, F., & Sareen, J. (2009). Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. Journal of psychiatric research 43(10), 926-933.
- Ravert, R.D., Fu, L.Y., & Zimet, G.D. (2021). Young Adults COVID-19 Testing Intentions: The Role of Health Beliefs and Anticipated Regret. The Journal of Adolescent Health, 68(3), 460-463.
- Riemann, D., Krone, L.B., Wulff, K., & Nissen, C. (2020). Sleep insomnia and depression. Neuro psychopharmacology 45(1), 74-89.
- Schneiderman, N., Ironson, G., & Siegel, S.D. (2005). Stress and health: psychological, behavioral, and biological determinants. Annual review of clinical psychology 1, 607-628.
- Sleep Assessment Tools Sleep Assessment Questionnaire (2018). Eisenberg Family Depression Center. Available online at: https://www.depressioncenter.org/toolkit/im-looking-more-resources-1/self-assessment-tools
- Spitzer, R.L., Kroenke, K., Williams, J.B.W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder the GAD-7. Arch intern med, 166(10), 1092-1097.
- Toscos, T., Carpenter, M., Drouin, M., Roebuck, A., Kerrigan, C., et al. (2018). College Students Experiences with and Willingness to Use Different Types of Telemental Health Resources Do Gender Depression Anxiety or Stress Levels Matter. Telemed J E Health 24(12), 998-1005.
- Van Droogenbroeck, F., Spruyt, B., & Keppens, G. (2018). Gender differences in mental health problems among adolescents and the role of social support results from the Belgian health interview surveys. BMC Psychiatry 18(1),6.
- Wang, X., Chen, H., Liu, L., Liu, Y., Zhang, N., et al. (2020). Anxiety and Sleep Problems of College Students During the Outbreak of COVID-19. Frontiers in psychiatry 11, 588693.
- Xie, J., Li, X., Luo, H., He, L., Bai, Y., et al. (2021). Depressive Symptoms, Sleep Quality and Diet During the 2019 Novel Coronavirus Epidemic in China: A Survey of Medical Students. Frontiers in public health, 8, 588578.





