Case Report
The Journey of a Patient with Post Laser-Assisted In-Situ Keratomileusis Complications and Contact Lenses: A Case Report
2803
Views & Citations1803
Likes & Shares
Significance: Post laser-assisted in-situ keratomileusis (LASIK) ectasia induces a significant amount of higher order aberrations (HOAs) which leads to visual symptoms like glare, haloes, monocular diplopia, ghosting, multiple images, and starbursts and decreased night vision. Special design gas permeable lenses of different diameter can compensate the HOAs by neutralizing the surface irregularities.
Purpose: To report the utilization of gas permeable contact lenses of different designs and diameters at various stages of post- LASIK complication.
Case report: A 38 years old male underwent LASIK in both eyes and postoperatively complained of glare, haloes and blurred vision in the right eye. He was diagnosed with epithelial ingrowth and decentered ablation. He subsequently developed post-LASIK ectasia and underwent collagen cross-linkage. After that he underwent deep anterior lamellar keratoplasty (DALK) for post cross-linkage induced corneal haze. Different gas permeable lens designs (ROSE K2 Post graft, ROSE K2 KC design) with additional modifications (asymmetric corneal technology) helped to improve lens fitting for the highly irregular oblate cornea secondary to decentered ablation and scaring due to epithelial ingrowth to the advanced prolate corneal shape secondary to ectasia. Visual quality and comfort has also improved with different vision enhancement options. Finally, the patient was fitted with prosthetic replacement of ocular surface ecosystem (PROSE, Boston Foundation for Sight, Needham, Massachusetts, USA) device and is using it successfully. The report focuses on how the different lens designs helped on reducing higher-order aberrations and enhanced patient’s quality of life at different stages of the disease.
Conclusions: Corneas with post LASIK complications require multiple lens options with different designs in different phases of the disease for a better fitting relationship, vision enhancement and improved comfort.
Keywords: Scleral lens, Post-LASIK ectasia, Deep anterior lamellar keratoplasty, Higher-order aberrations
INTRODUCTION
Laser-assisted in-situ keratomileusis (LASIK) is the commonest refractive procedure performed worldwide due to its high predictability and excellent safety profile [1]. Despite recent advancements in screening tools and surgical techniques, complications such as epithelial ingrowth; decentered ablation zones, post LASIK ectasia, dry eye and corneal neuralgia do occur [1].
The risk factors for corneal ectasia include high preoperative myopia, low residual stromal bed thickness, and topographic abnormalities [1]. Postsurgical alterations in the biomechanical strength of the cornea cause mechanical instability and keratectasia in predisposed eyes [1]. Post-LASIK ectasia is characterized by progressive thinning and steepening of the ablated cornea. It causes refractive or optical regression and induces significant irregular astigmatism and higher order aberrations (HOA) [2].
These HOAs can be compensated by masking or neutralizing the surface irregularities by fitting rigid gas permeable lenses of different advanced designs and diameters. In a highly irregular cornea, conventional rigid gas permeable (GP), piggyback, hybrid lenses might not fit, and scleral lenses might be the only option left [3].
Scleral lenses are large-diameter gas permeable contact lenses that vault over the entire corneal surface, limbus, and supported by the sclera. Fluid reservoir thickness is probably the most crucial advantage that these lenses offer over corneal lenses other than excellent comfort, stability, and proper centration and rigidity that improves vision [3]. Prosthetic replacement of ocular surface ecosystem (PROSE) (Boston Foundation for Sight, Needham, Massachusetts, USA) is a proven successful option for patients with irregular cornea and ocular surface disorders [3-5]. Due to its advanced customization option and additional features like front surface eccentricity, it has been considered an effective solution in eyes with post-LASIK ectasia [6].
This case report describes the use of different advanced designs and diameter of GP lenses in a post-LASIK eye, from an earlier oblate shape due to LASIK with decentered ablation to advanced prolate corneal profile secondary to ectasia.
CASE REPORT
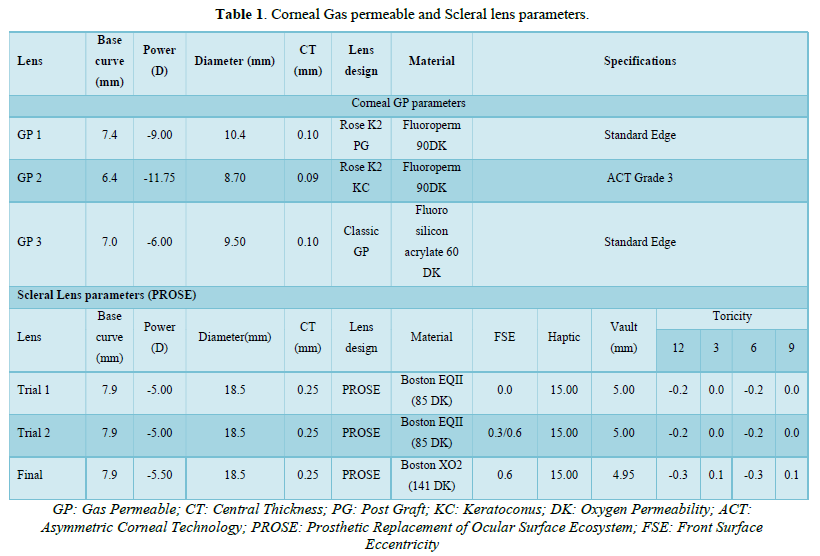
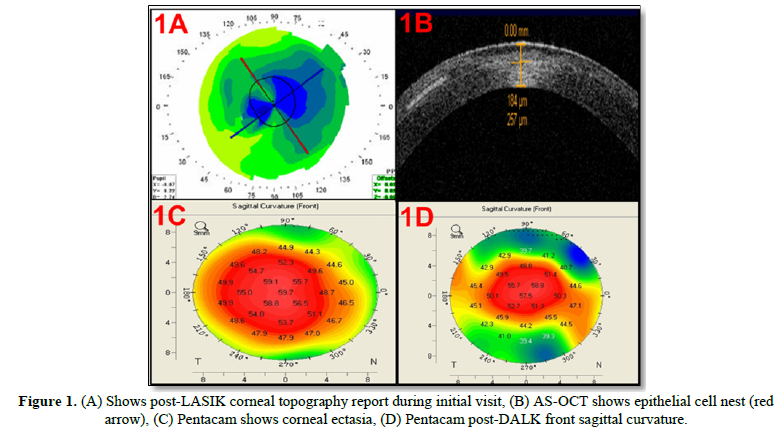
A 38-year old male presented with blurred vision, glare, haloes, and difficulty in night driving 10 months after the LASIK procedure. The preoperative refractive error was -4.00 -2.00 × 180 in both eyes. On examination, his spectacle-corrected visual acuity was 20/32, n6 with +1.00DS/-1.00DC @20 (20/32, N6) in right eye and with plano 20/25, N6 in left eye. The keratometric value was right eye: K1:36.75 D @20, K2 38.25D@110 and left eye: K1:37.00D @60, K2 39.25D@ 150. Slit-lamp examination of both eyes revealed epithelial nests or ingrowth under the Lasik flap. Corneal topographic (Pentacam HR, Oculus, Wetzlar, Germany) evaluation and anterior segment optical coherence tomography (AS-OCT) revealed irregular corneal topography with decentered ablation zone (Figure 1A) secondary to epithelial proliferation cells in the interface (Figure 1B), in right eye.
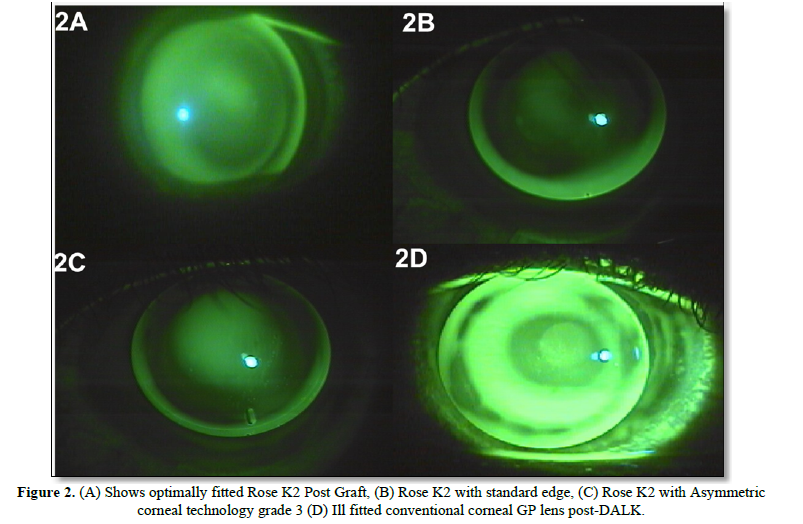
After flap lift with debridement of the epithelial cell nest he was advised contact lens trial in right eye due to blurring of vision. A trial with Rose K2 PG (Post Graft), specially designed reverse geometry corneal GP lens design for oblate cornea was performed (Table 1) in right eye, and with the final lens his vision improved to 20/20, N6. The lens fitting was acceptable with minimal central pooling, mid-peripheral touch and adequate edge clearance (Figure 2A).
On the sixth month follow up patient reported an inability to tolerate the lenses and was noted to have developed corneal ectasia in the right eye (Figure 1C). He underwent collagen cross-linkage in the right eye to stabilize his condition, and post-cross-linkage was reevaluated for contact lens fitting.
The patient was fitted with the Rose K2 KC (keratoconus) design contact lens due to its different modification options like standard, flat, steep peripheral system, toric curves, and aspheric lens design. Rose K2 KC multi-curve design (Table 1) showed an acceptable fitting with minimal central clearance (to compensate for further progression), edge lift at 6 o clock position (Figure 2B) and adequate edge was achieved with asymmetric corneal technology grade 3 (Figure 2C) and vision improved to 20/25, N6 with mild shadowing.
The patient was unhappy with his quality of vision secondary to the mild haze post-cross-linkage and underwent DALK but he still had fairly steep cornea with prolate surface (Figure 1D). The flattening of cornea post DALK helped to fit a spherical corneal GP lens for his myopic astigmatism (Table 1).
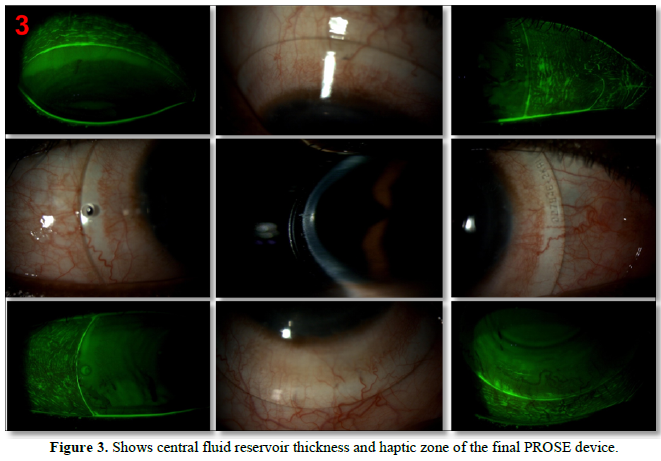
In follow-up visits, the lens fitting was compromised (Figure 2D) and fitted with a PROSE device. During initial trial lens patient was complaining of mild shadowing (Table 1), hence further trials were done with front surface eccentricity (FSE) of 0.30 and then 0.60 (Table 1) to reduce shadowing. Spherical equivalent over refraction was done and vision was recorded. Central and limbal fluid reservoir thickness and haptic zone modifications were done and the lens was ordered with Boston XO2 (DK=141) material. The final lens with FSE 0.60 provided the corrected visual acuity of 20/20, N6 without any shadowing showed adequate central and limbal clearance with properly aligned haptic (Table 1 & Figure 3).
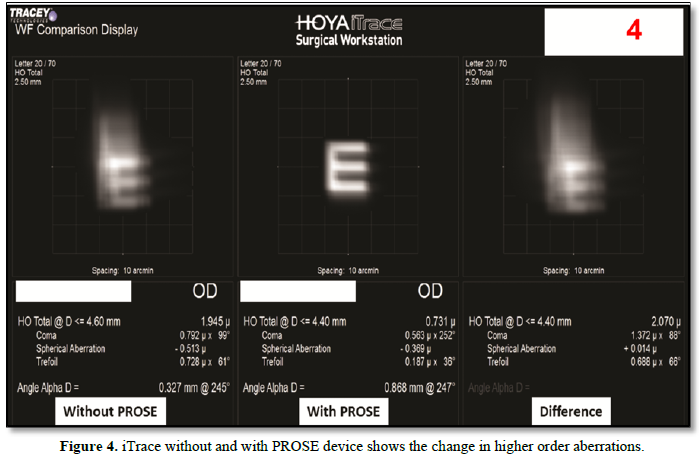
iTrace (Tracey Technologies Corp, Houston, TX) was done before and during PROSE wear and showed a significant reduction in higher order aberrations (Figure 4), improvement in quality of vision and felt comfortable even during night driving with device on eye. Pentacam pachymetry showed a central corneal thickness of 498 microns at baseline, which increased to 516 microns after 8 h of lens wear and caused 3.61% of corneal edema. The reported corneal edema was within normal physiological closed eye corneal edema and also not reported any hypoxia-related complications. The patient reported significant improvement in the quality of vision, reduced visual symptoms, dryness, and enhanced quality of life and has been using the lens regularly for the last 1years.
DISCUSSION
Post LASIK complications causes significant corneal irregularity with increased amount of HOAs [2] leading to different visual symptoms like reduced vision, monocular diplopia; ghosting of images mainly in scotopic conditions [7]. Sometimes, the large pupil size further deteriorates the condition. In this report the ROSE K2 Post Graft lenses, a specially designed lens for post graft and post-refractive
surgery eyes were used. This lens incorporates reverse geometry curves to closely align the lens's back to the cornea and decreases the tear layer thickness over the pupil and provides improved vision.
The patient developed progressive post LASIK ectasia and at this stage and a specialized multi-curve ROSE K2 KC with aspheric optics design was fitted optimally. Aspheric optics and front surface aberration control optics of these lenses also helped to provide an improved quality of vision.
The patient was shifted to a scleral lens in the post graft state, as the special design corneal GP lens fit and comfort was suboptimal. Scleral lenses are considered to be an effective option for correcting refractive error and HOAs by masking the corneal irregularities [2]. The advanced characteristics of PROSE lenses make the lens fitting facile even in the post-DALK steep cornea. The patient reported comfortable lens wear for long hours with the PROSE device and could be more independent than before.
In patients with highly irregular corneal surfaces or who had undergone multiple corneal surgeries, a scleral device with FSE will result in better visual quality, by reducing the higher-order aberrations [8,9]. FSE can be best explained by the term aspehricity (Q) that defines the rate of change in curvature from apex to the periphery, higher the ectasia, Q value will be higher and will need a higher eccentricity value. Our patient had a significant decrease in shadowing and distortion with the PROSE device with a FSE of 0.60 compared to FSE 0.30 and the same has been reported by previous studies [8]. Previous studies have quantified the amount of HOAs in post-LASIK ectasia [2] eyes and also reported the usefulness of Scleral lenses on reduction of that and the result of the present case report is also in broad agreement with that.
Dry eyes are a remarkably frequent consequence of LASIK surgery, and a small proportion of patients develop chronic and severe dry eyes. Studies have reported that the tear film and the tear quality were reduced post-LASIK and observed a significant decrease in corneal sensitivity [10]. In current report the patient was not able to use his laptop for longer hours due to dryness, and was dependent on lubricant eye drops. He reported a marked reduction in dryness with scleral device and very occasional use of lubricants. He also had significant improvement in the quality of vision and could wear the lens without any discomfort or lens awareness.
Fitting contact lenses in post-LASIK eyes on its different phases of complications is very complex and challenging. It requires flexible lens design and diameter of GP lenses with additional features like aspheric optics and front surface eccentricity. The choice of design depends on the profile of the cornea. By dispensing different lens designs in a different stage of the disease, we provided the patient with a better vision and improved quality of life. Aberrometer should be considered as an important measurement tools and should be regularly used in specialty practice to quantify the amount of HOAs mainly in irregular corneas like post-LASIK ectasia.
ACKNOWLEDGEMENT
The authors would like to thank the entire Contact Lens department for their continuous support.
POTENTIAL CONFLICT OF INTEREST
The authors report no conflicts of interest.
FUNDING
This case report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
- Randleman JB (2006) Post-laser in-situ keratomileusis ectasia: Current understanding and future directions. Curr Opin Ophthalmol 17: 406-412.
- Kumar M, Shetty R, Lalgudi VG, Khamar P, Vincent SJ, et al. (2021) The effect of scleral lenses on vision, refraction and aberrations in post-LASIK ectasia, keratoconus and pellucid marginal degeneration. Ophthalmic Physiol Opt 41(4): 664-672.
- Baran I, Bradley JA, Alipour F(2012) PROSE treatment of corneal ectasia. Cont Lens Anterior Eye 35: 222-227.
- Jacobs DS, Rosenthal P (2007) Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea 26: 1195-1199.
- Papakostas TD, Le HG, Chodosh J (2015) Prosthetic replacement of the ocular surface ecosystem as a treatment for the ocular surface disease in patients with a history of Stevens-Johnson syndrome/toxic epidermal necrolysis. Ophthalmology 122: 248-253.
- Mian SZ, Agranat JS, Jacobs DS (2016) Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) treatment for complications after LASIK. Eye Contact Lens 42: 371-373.
- McCormick GJ, Porter J, Cox IG (2005) Higher-order aberrations in eyes with irregular corneas after laser refractive surgery. Ophthalmology 112: 1699-1709.
- Kumar P, Mohamed A, Bhombal F, Dumpati S, Vaddavalli PK (2019) Prosthetic replacement of the ocular surface ecosystem for corneal irregularity: Visual improvement and optical device characteristics. Cont Lens Anterior Eye 42(5): 526-532.
- Hussoin T, Le HG, Carrasquillo KG, Johns L, Rosenthal P, et al. (2012) The effect of optic asphericity on visual rehabilitation of corneal ectasia with a prosthetic device. Eye Contact Lens 38: 300-305.
- Shtein RM (2011) Post-LASIK dry eye. Expert Rev Ophthalmol 6: 575-582.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Dermatology Clinics and Research (ISSN:2380-5609)





