2714
Views & Citations1714
Likes & Shares
DISCUSSION
From anatomic perspective we mean by anal canal, the segment between the dentate line tend the anal verge. Moreover, the surgical view considers the anal canal, as the area from the palpable anorectal ring to the peri-anal skin. This later definition is the most widely accepted in practice and the most preferred by the American Joint Committee on Cancer (AJCC). Therefore, any tumour involving the anorectal junction is stated as a rectal cancer in this case, the topography epicentre is more than 2 cm proximal to dentate line. In addition to, anal cancer is defined if the epicentre is 2 cm or less from the dentate line. Taxonomically, tumours of the peri-anal skin are designated as perianal cancers and resemble biologically to other skin tumours [72,13,30]. This contrast is crucial since anal cancers are more aggressive than cancers of the peri-anal skin, furthermore its incidence is up to 5 times more common than that of anal margin lesions [12,13,16,30].
Consistently, anal cancer was regarded as a disease of older women, with onset in the 7th decade of life. This neoplastic entity used to be of a very rare occurrence. However, over the past decades its incidence has raised especially in women and in homosexual men. Additionally, for the past decade, its escalated incidence has redheaded the range of 2,2 % annually. Furthermore, this cancer represented 0,5 % of all cancers diagnosed in the USA [1,9,17-19]. Etiologically, the nowadays occurrence of anal cancer is more related to Human Papilloma Virus infection in 91 % so that the frequency of this malignancy is merged in younger people of both genders affected by this virus. Therefore, since the probability of developing this cancer is 120-fold when there is a pre-existing HPV ano-rectal infection, anal cancer in young people can be regarded as a sexually transmitted neoplastic disease which needs a prophylactic measure involving a sexual education in puberty and adolescent age groups as well as, a vaccination against this infectious agent. And the most oncogenic serotypes are HPV 16 and 18. thus, the biopsy is recommended once there is ano-rectal HPV infection especially when there is a coexistent HIV infection [2-8,14,26-28]. Results of peer-reviewed studies of anal cancer, including detection of HPVDNA, demonstrated that the prevalence of HPV16 and 18 in 72 % of patients, and includes screening for vaginal and cervical cancer and male external genitalia. Anal cancer has numerous risk factors apart from HPV such as a non-protected sexual life in term of multiple partners, anal receptive intercourse in both genders, history of vulvar or vaginal and cervical dysplasia or cancer, advanced age, smoking and immunosuppression related to different organs such as HIV infection or solid [15,16,20,22-25].
A study using data from the Danish Cancer Registry demonstrated that the probability of developing anal cancer after a diagnosis of cervical cancer or cervical intraepithelial neoplasia was three to five times as high as the probability of developing stomach or colon cancer with a strong association between cervical cancer and anal cancer. Frisch et al. have found an association between anal cancer and lymphoma or leukaemia and raises a possible role of immunodeficiency in the development of anal cancer [29].
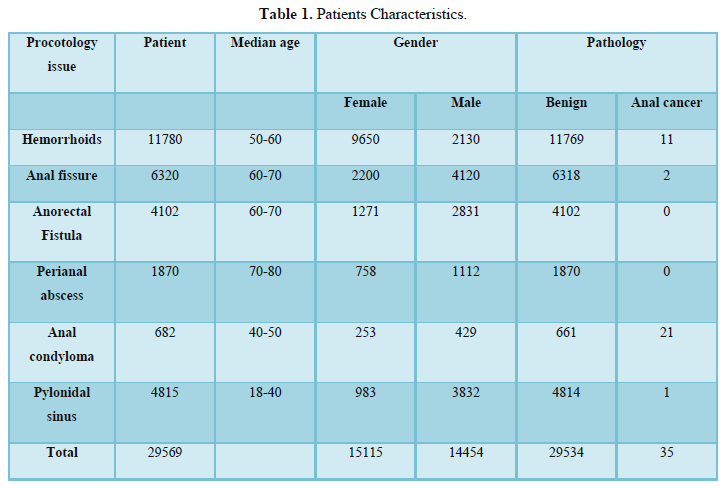
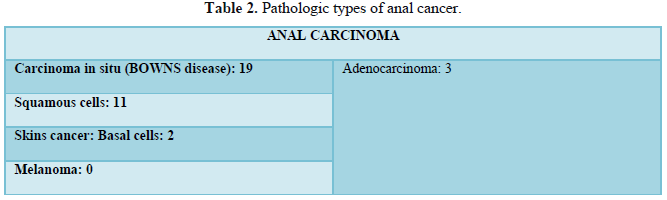
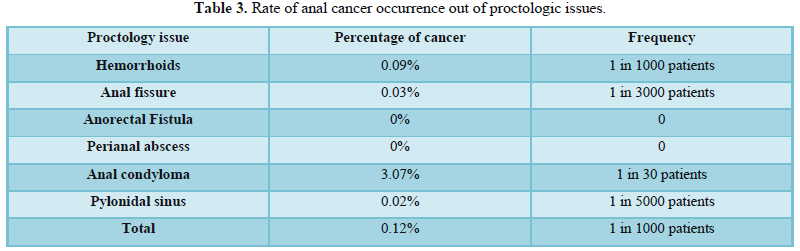
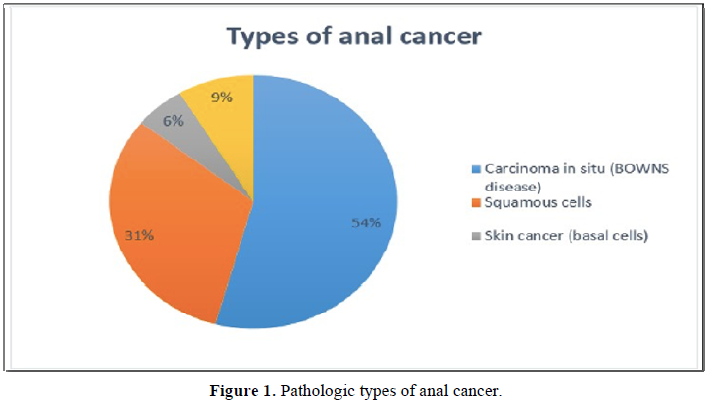
Regarding pathologic perspective, 85 % of anal cancers are of squamous type [21,29] but in us study the most prevalent histologic type was carcinoma in situ (Bowns disease) with 54% followed squamous cell carcinoma with 31 % and adenocarcinoma with 9 %, skin cancer (basal cell) 6%. There was no case of anal melanoma in our study.
CONCLUSION
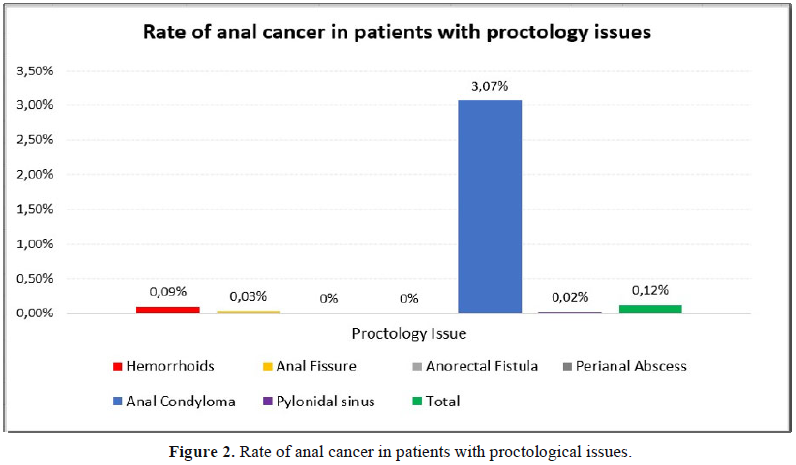
Anal cancer remains a nosologic entity of rare occurrence even among different proctologic issues. Its incidence is nowadays increasing because of the epidemiologic profile of HIV infection in both genders, especially in young population. We suggest a good sexual education in adolescent population as well as vaccination against this etiological as well as a screening ano-rectal biopsy in women with history of vulvo-vaginal HPV infection or cancer and in general in high risk patients such as immunocompromised patients from different origins.
- Nelson VM, Benson AB (2017) "Epidemiology of Anal Canal Cancer". Surg Oncol Clin North Am 26 (1): 9-15.
- Anal Cancer Prevention (2014) National Cancer Institute. Accessed on: 30 May 2019.
- National Cancer Institute (2009) Anal Cancer Treatment (PDQ) Patient Version. Archived July 14, 2009, at the Way back Machine 13 June 2008. Accessed on: 26 June 2009.
- Margaret AS, David MW, Jane SC, Goon, Peter KC (2012) HPV infection, anal intra-epithelial neoplasia (AIN) and anal cancer: Current issues. BMC Cancer 12 (1): 398.
- Frisch M (2002). "On the etiology of anal squamous carcinoma". Danish Med Bullet 49 (3): 194-209.
- Frisch M, Glimelius B, van den Brule AJ, et al. (1997) Sexually transmitted infection as a cause of anal cancer. N Engl J Med 337 (19): 1350-1358.
- Parkin DM (2006) The global health burden of infection-associated cancers in the year 2002. Int J Cancer 118 (12): 3030-3044.
- Fred Hutchinson Cancer Research Centre (2007) Changing trends in sexual behaviour may explain rising incidence of anal cancer among American men and women. Fred Hutchinson Cancer Research Centre (fhcrc.org).
- "Anal Cancer" American Cancer Society (2014).
- Esiashvili N, Landry J, Matthews RH (2007) “Carcinoma of the Anus Management”. Armenian Health Network, Health.
- Saleem AM, Paulus JK, Shapter AP, Baxter NN, Roberts PL, et al. (2011) "Risk of anal cancer in a cohort with human papillomavirus-related gynaecologic neoplasm". Obstet Gynaecol 117 (3): 643-649.
- American Joint Committee on Cancer (2018) AJCC Cancer Staging Form Supplement, AJCC Cancer Staging Manual, Eighth Edition, Last updated 05 June 2018.
- MB Amin, SB Edge, FL Greene, et al. (2017) AJCC Cancer Staging Manual. 8th edition, New York: Springer.
- Tuller, David (2007-01-31) “HPV vaccine may help to prevent anal cancer”. International Herald Tribune.
- Agency for Healthcare Research and Quality (2008) "Hospital HIV Clinic Offers Convenient, Proactive Screening for Anal Cancer, Enabling Identification and Treatment of Precancerous Lesions".
- National Comprehensive Cancer Network (2013) "NCCN Clinical Practice Guidelines in Oncology: Anal Carcinoma. V 1".
- Cancer Research (2008) "Detailed Guide: Anal Cancer What Are the Key Statistics About Anal Cancer?"
- net (2019) "Anal Cancer: Statistics" Cancer.net.
- net (2014) "Anal Cancer Statistics" Cancer Research UK.
- Tong WW, Hillman RJ, Kelleher AD, Grulich AE, Carr A (2014) Anal intraepithelial neoplasia and squamous cell carcinoma in HIV-infected adults. HIV Med 15: 65-76.
- Flejou JF (2015) An update on anal neoplasia. Histopathology 66:147-160.
- Berry JM, Jay N, Cranston RD, Darragh TM, Holly EA, et al. (2014) Progression of anal high-grade squamous intraepithelial lesions to invasive anal cancer among HIV-infected men who have sex with men. Int J Cancer 134: 1147-1155.
- Nagle D (2009) Anal squamous cell carcinoma in the HIV-positive patient. Clin Colon Rectal Surg 22: 102-106.
- Ouhoummane N, Steben M, Coutlee F, Vuong T, Forest P, Rodier C, et al. (2013) Squamous anal cancer: Patient characteristics and HPV type distribution. Cancer Epidemiol 37: 807-812.
- Mendez-Martinez R, Rivera-Martinez NE, Crabtree-Ramirez B, Sierra-Madero JG, Caro Vega Y, et al. (2014) Multiple human papillomavirus infections are highly prevalent in the anal canal of human immunodeficiency virus-positive men who have sex with men. BMC Infect Dis 14: 671.
- Garcia-Espinosa B, Moro-Rodriguez E, Alvarez-Fernandez E (2013) Human papillomavirus genotypes in human immunodeficiency virus-positive patients with anal pathology in Madrid, Spain. Diagn Pathol 8: 204.
- Cachay E, Agmas W, Mathews C (2015) Five-year cumulative incidence of invasive anal cancer among HIV-infected patients according to baseline anal cytology results: an inception cohort analysis. HIV Med 16: 191-195.
- Wexler A, Berson AM, Goldstone SE, Waltzman R, Penzer J, Maisonet OG, et al. (2008) Invasive anal squamous-cell carcinoma in the HIV-positive patient: Outcome in the era of highly active antiretroviral therapy. Dis Colon Rectum 51: 73-81.
- Abunassar M, Reinders J, Jonker DJ, Asmis T (2015) Review of anal cancer patients at the Ottawa hospital. Eur J Surg Oncol 41: 653-658.
- Sinnatamby CS (1999) Last's anatomy: Regional and applied. 10th edition, Edinburgh: Churchill Livingstone.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Spine Diseases
- International Journal of Anaesthesia and Research (ISSN:2641-399X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)



