1803
Views & Citations803
Likes & Shares
Most of the currently available medical literature describes GISTs with gastrointestinal bleeding, intussusception and obstruction. Small bowel GIST presenting with prolonged fever is probably not documented in the current literature.
We decided to report this case of a 53year old male patient presented with prolonged fever for nearly six weeks due to necrotic mid ileal GIST managed successfully with minimally invasive surgery.
CASE PRESENTATION
A 53 years old previously well male patient was referred form the medical ward after being investigated for ongoing fever by the consultant physician. This patient initially presented to a nearby base hospital and was evaluated for ongoing fever for five weeks with multiple basic investigations without a cause.
Patient had on and off nocturnal fever with mild degree of weight loss and loss of appetite, there was no history of chronic cough or pleuritic type chest pain. Direct questioning did not reveal any significant bowel or urinary symptoms. He was a nonalcoholic and a nonsmoker with no past history of significant surgical procedures.
Clinical examination was unremarkable without significant lymphadenopathy. Respiratory, cardiovascular and neurological systems were normal. Abdominal examination was also normal with mild tenderness in the central abdomen. Investigations revealed a total white cell count of 13.8 x109 /L with 73% neutrophils. C-Reactive protein was 146 mg/L. Erythrocyte Sedimentation Rate was 120mm/h.
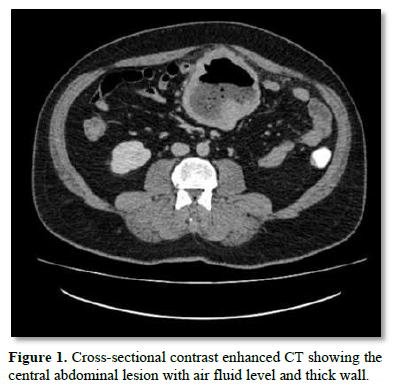
Serum Lactate Dehydrogenase (LDH) was within normal limits with normal liver and renal function tests. Urine and blood cultures didn’t yield any growth. Blood picture was normochromic normocytic red cells with roulex formation and demonstrated toxic neutrophils with monocytosis. Patient had a negative Mantoux test. On imaging studies, he had a normal chest x-ray with a normal 2D-Echo cardiogram. There was no evidence of endocarditis on trans esophageal echo cardiogram. Ultra sound scan of the abdomen done in our institution showed a thickened segment of bowel loop in the central abdomen and suggested a contrast enhanced CT scan which demonstrated a 9 x 8cm cavitatory lesion with thick wall and air fluid level in the central abdomen with mild fat stranding around the lesion (Figure 1). Rest of the abdomen and pelvis was normal. Considering the location and the features the radiologist suggested that this could be a cavitatory tumor like a GIST.
With this background, we performed a diagnostic laparoscopy and found a mid ileal mass as described before. Rest of the abdomen and pelvis was unremarkable except for few enlarged mesenteric lymph nodes. As the mass was nearly 10cm in size we exteriorized the small bowel using a limited mid line incision by extending the umbilical port site and using a disposable wound retractor (Figure 2). Tumor containing small bowel was segmentally resected and the bowel was anastomosed in an end to end fashion. Patient recovered without any post-operative complications and was discharged on post op day 6. On subsequent follow up he was referred to oncologist for further management.
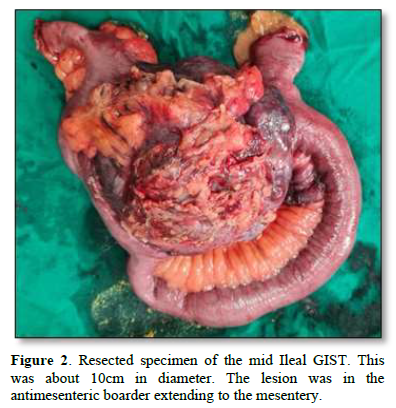
On pathological examination there was a nodular mass adhered to the ileal mesentery with a dimension of 110mm x 95mm x 90mm. There were adequate intestinal margins on either side. Cut surface showed a cystic central area filled with necrotic material. Preliminary histological evaluation demonstrated a well-defined bland spindle cell lesion with ischemic type necrosis in the central area. Immunohistochemistry was performed to confirm the diagnosis and the lesion was negative for SMA, Desmin and CD34. CD117 was positive with Ki67 less than 1%. Therefore, it was a Gastrointestinal stromal tumor with central cystic degeneration and Ki67 < 1%.
DISCUSSION
Gastrointestinal stromal tumors (GISTs) are rare neoplasms of the gastrointestinal tract originating from pluripotential mesenchymal stem cells, which differentiate into the interstitial Cajal cell. 50% are seen in the stomach and about 30% are seen in the small intestine [1,2]. The clinical presentation of this uncommon tumors is highly variable and depends on the size, location and presence of mucosal ulceration. These lesions are generally immune histochemically positive for KIT (CD117). Clinical behaviors of these tumors can range from benign to malignant and this depends on the size and the mitotic activity. Histologically they can be one of three types spindled, epithelioid, or mixed spindled and epithelioid type. The most common spindle type is 95% positive to CD1179 [3].
GISTs can be asymptomatic and detected during cross sectional imaging during investigation for a different complaint or during endoscopic examination. Most of these tumors when symptomatic present with abdominal discomfort and nonspecific abdominal pain. Tumors more than 4cms have presented with gastrointestinal hemorrhage [2]. Very rarely they have caused intussusception and bowel obstruction. Our patient though had some degree of nonspecific pain the main worrying symptom was the prolonged fever for nearly six weeks by definition which falls into PUO. Through workout with relevant investigations are necessary to arrive in a diagnosis. This type of presentation of a GIST was extremely rare and not accounted for in the current surgical literature.
Cross sectional imaging with contrast enhanced CT scans is really helpful in detecting small bowel GISTs [5]. Once diagnosed the mainstay of treatment is surgical resection. The aim should be to resect the lesion with an adequate margin and an intact pseudo capsule. These tumors generally do not metastasize to regional lymph nodes thus making the regional lymphadenectomy unnecessary [4]. The behavior of the tumor and further adjutant treatment with Imatinib which is an oral kinase inhibitor will depend on histological characteristics of the tumor [4]. In this patient the tumor was spindle cell type positive for CD117 with a very low Ki 67 proliferative index indicating a low risk lesion.
Our case was an extremely rare presentation of a mid ileal GIST where the patient presented with prolonged fever. Pyrexia was due to the central ischemic degeneration of the GIST as it was nearly 10 cm in size. Systematic evaluation of the patient with relevant investigation are needed to arrive in a diagnosis in a patient with pyrexia of unknown origin. Careful planning and the use of laparoscopic approach was associated with a good surgical outcome in our patient. This case also highlights the importance of the multidisciplinary team involvement in the patient management with the valuable input from the radiology and pathology services with the immunohistochemistry facilities.
LEARNING POINTS
- Gastrointestinal stromal tumors (GISTs) are rare tumors of mesenchymal origin with varied presentations
- Most of the present literature is about tumors presenting with bleeding, intussception and obstruction. Prolong fever is an extremely rare presentation.
- High degree of suspicion and multidisciplinary involvement is needed for diagnosis and management.
- Minimal invasive surgery offers excellent surgical outcome with proper patient selection.
- Giestas S, Almeida N, Martins R, Canhoto A, Oliveira P, et al. (2016) Small Bowel GIST: Clinical Presentation as Intussusception and Obscure Bleeding; GE Port J Gastroenterol. 23(5): 279-281
- Saad MK, El Hajj I, Saikaly E (2020) Jejunal gastrointestinal stromal tumor (GIST): A case report presenting as life threatening emergency. Gastrointest Stromal Tumor 3: 3.
- Jumniensuk C, Charoenpitakchai M (2018) Gastrointestinal stromal tumor: Clinicopathological characteristics and pathologic prognostic analysis. World J Surg Onc 16: 231.
- Ahmed M (2020) Recent advances in the management of gastrointestinal stromal tumor. World J Clin Cases 8 (15): 3142-3155.
- El-Menyar A, Mekkodathil A, Al-Thani H (2017) Diagnosis and management of gastrointestinal stromal tumors: An up-to-date literature review. J Cancer Res Ther 13: 889-900.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of AIDS (ISSN: 2644-3023)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)



