268
Views & Citations10
Likes & Shares
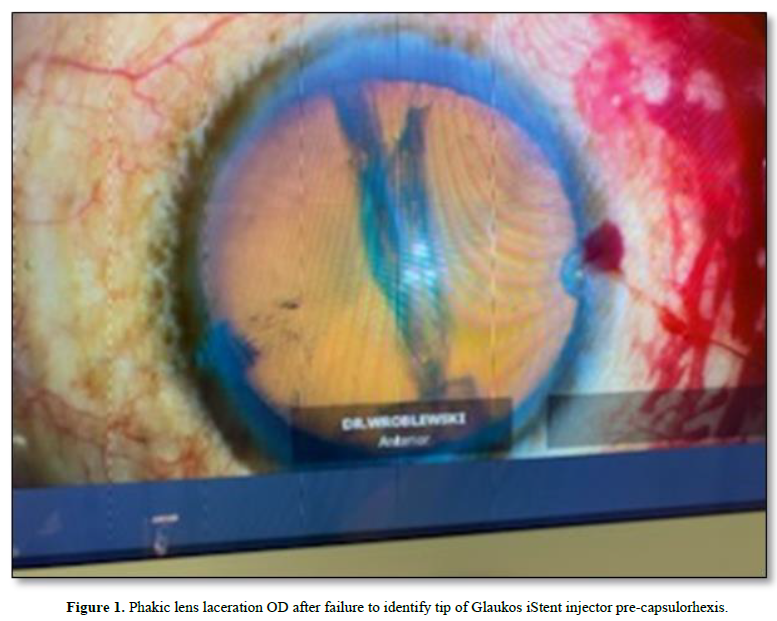
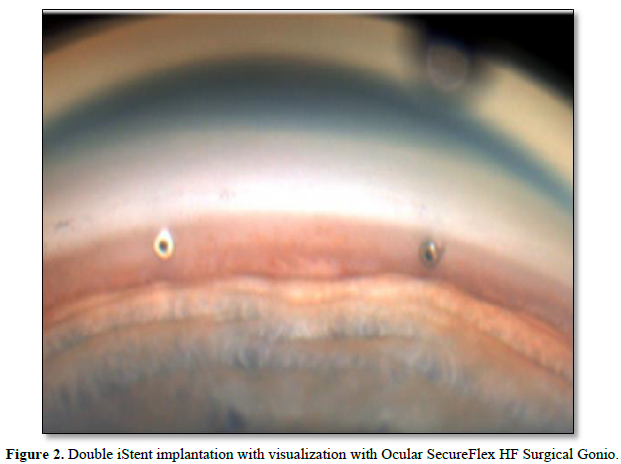
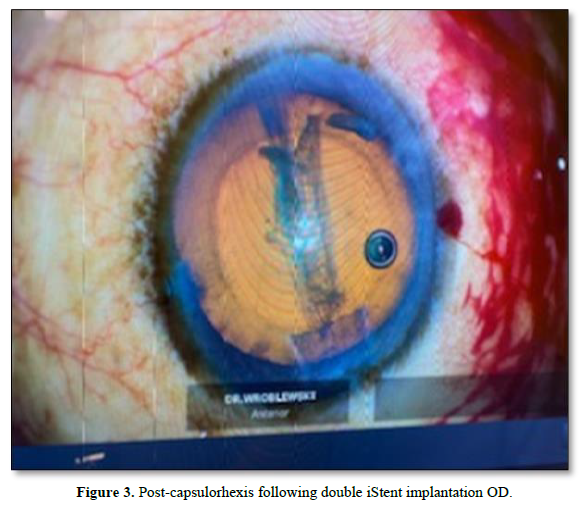
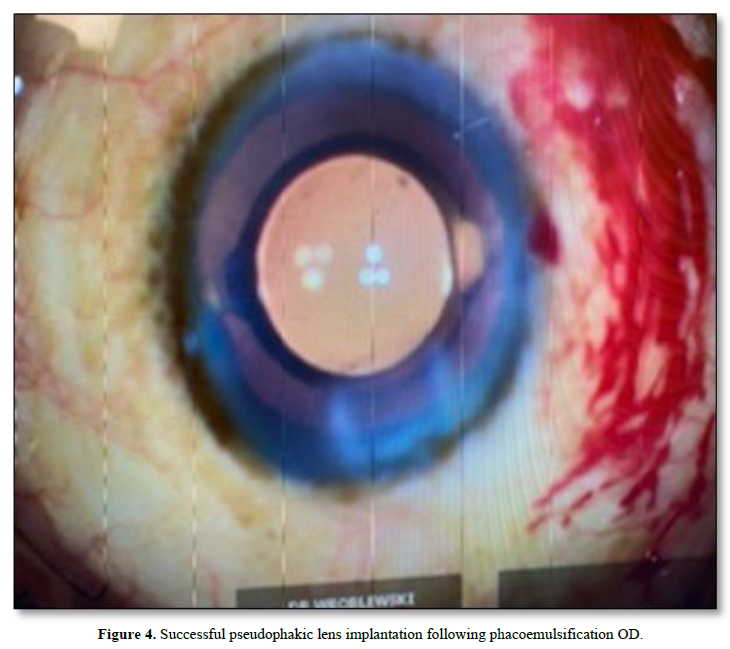
Diagnosis, Intervention, and Outcomes: Repeated efforts to identify the iStent applicator tip failed, resulting in the use of the Ocular SecureFlex HF Surgical Gonio to successfully implant two iStent devices. Successful phacoemulsification and intraocular lens implantation for cataract resolution followed iStent implantation.
Conclusion: Resident inexperience with surgical instruments such as Gonio Lenses may lead to iatrogenic lens injuries during MIGS for POAG. In this case, the patient’s lens and capsule was lacerated during iStent implantation preceding cataract removal. Performing the iStent implantation before phacoemulsification for cataract removal may be beneficial, as a lacerated phakic lens can be removed following iStent insertion.
Keywords: Cataract surgery, Micro-Invasive glaucoma surgery, Primary open-angle glaucoma, Medical education
CASE REPORT
A 76 y/o African-American male patient with moderate primary open-angle glaucoma (POAG) and cataracts presented for planned cataract extraction/intraocular lens implementation and two iStent implantations OD. Visual acuity prior to surgery was 20/400 and 20/60 with pinholes OD. Preoperative IOP was 17 mmHg. A 2.4 mm main wound was constructed temporally at 180° followed by Vision Blue injection into the angle. Following patient preparation and draping, the patient was angled 30° away from the surgeon with the scope angled 30° toward the surgeon. Prior to iStent implantation, gonioscopy with a Volk Gonio Lens was performed in appropriate fashion. A forehand grip was applied to the Glaukos second generation iStent injector, and the tip was inserted through the main wound. Repeated attempts were made to carefully identify the tip of the injector; however, the tip was unable to be visualized. The iStent injector tip was removed from the anterior chamber. There was subsequent discovery of anterior capsular and lenticular damage by the iStent tip (Figure 1). The Volk Gonio Lens was removed and replaced with an Ocular Secure Flex HF Surgical Gonio. The two iStent implantations were successfully inserted with the second gonio insertion OD (Figure 2). A continuous curvilinear capsulorhexis was performed around the site of capsule injury. There was concern that the posterior capsule has been violated, therefore, a gentle hydro dissection and phacoemulsification were performed (Figure 3). No violation was noted upon posterior capsule inspection. An intraocular lens was inserted within the capsular bag (Figure 4). Following surgery, the patient recovered with no complications. The patient’s POAG and cataract were resolved with iStent implantation followed by cataract removal and intraocular lens insertion OD.
DISCUSSION
The combination of iStent implantation with cataract surgery has been shown to reduce IOP and decrease the use of medications for patients with primary open-angle glaucoma (POAG) or ocular hypertension (OHT) and cataract for up to five years postoperatively [5]. Although the conventional practice is to perform iStent implantation following cataract extraction, this case report documents the benefit of performing iStent implantation before cataract removal, in the case of phakic capsule and lens injury with the iStent injector. Minimal research has been conducted on the effectiveness or possible complications of beginning with iStent implantation during combined MIGS and cataract surgery. Manning et al. retrospectively analyzed 63 eyes that underwent iStent implantation prior to cataract surgery and found no incidence of capsule indentation, capsule breech, or lens substance injury with combined MIGS and cataract surgery [4]. Although the data is limited, the preliminary research concludes a minimal risk of iatrogenic injury by performing iStent inject implantation before cataract surgery. However, there may be potential complications in conducting iStent implantation preceding cataract removal including diminished view of the anterior chamber (AC) due to bleeding caused by iStent implementation. A way to circumvent this potential complication is with irrigation and AC tamponade during iStent placement, which relieves hyphema and improves visualization during subsequent cataract surgery [4].
Cause analysis of the iatrogenic lens and capsule injury during iStent insertion described in this case includes resident inexperience with the use of the Volk Gonio Lens. The resident performing the surgery was trained in using the Ocular Secure Flex HF Surgical Gonio, the rescue gonio utilized after iStent injector identification initially failed. Therefore, performing iStent implantation before cataract surgery may be beneficial for resident or newly trained physicians with minimal experience with MIGS surgery. Qiu et al. analyzed the case logs from 152 graduating residents in 2018 and found a mean of 5.2 MIGS surgeries (iStent, Cypass, XEN, and Hydrus implants) per resident. Of the responding residents, 98 of 152 residents logged fewer than 5 MIGS surgeries as the primary surgeon and 48 of 152 residents logged 0 MIGS surgeries as the primary surgeon [6]. Furthermore, this study did not specify how many residents performed iStent implantations specifically as this procedure was grouped with the other MIGS implants. Given the extremely limited experience performing MIGS as the primary surgeon many residents receive during their training, it may be beneficial to consider starting combined MIGS and cataract surgeries with MIGS implantation to avoid iatrogenic injury to the capsule and lens.
Given the possibility of iatrogenic phakic lens injury during surgery as discussed in this case, iStent implantation preceding cataract extraction/intraocular lens insertion may be beneficial to minimize pseudophakic lens injury, especially for physicians with minimal experience with utilized surgical tools. This case study proposes the risk of iatrogenic injuries during MIGS when training physicians attempt to utilize surgical devices in which they have minimal experience with.
- Francis BA, Winarko J (2012) Ab interno Schlemm's canal surgery: Trabectome and i-stent. Dev Ophthalmol 50: 125-136.
- Sharma O, Abdulla D, King A, Chakrabarti M, Sharma T (2021) Role of minimally invasive glaucoma surgery in the management of chronic open-angle glaucoma. Sci Rep 11(1): 21432.
- Resende AF, Patel NS, Waisbourd M, Katz LJ (2016) iStent® Trabecular Microbypass Stent: An Update. J Ophthalmol 2016: 2731856.
- Manning DK, Haider A, Clement C, Viswanathan D (2022) Efficacy and Safety of iStent Inject Implantation in Manual and Femtosecond Laser-assisted Cataract Surgery before Lens Extraction. J Curr Glaucoma Pract 16(2): 105-110.
- Villalobos AP, Martinez-de-la-Casa JM, Diaz-Valle D, Morales-Fernandez L, Fernandez-Perez C, et al. (2016) Glaukos iStent inject® Trabecular Micro-Bypass Implantation Associated with Cataract Surgery in Patients with Coexisting Cataract and Open-Angle Glaucoma or Ocular Hypertension: A Long-Term Study. J Ophthalmol 2016: 1056573.
- Qiu M, Woreta FA, Boland MV (2021) Microinvasive Glaucoma Surgery in US Ophthalmology Residency: Surgical Case Log Cross-sectional Analysis and Proposal for New Glaucoma Procedure Classification. J Glaucoma 30(7): 621-628.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Immunology Research and Therapy (ISSN:2472-727X)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Forensic Research and Criminal Investigation (ISSN: 2640-0846)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Alcoholism Clinical Research
- International Journal of AIDS (ISSN: 2644-3023)





