Case Report
Variants of Uterus Didelphys with Obstructed Hemivagina and Ipsilateral Renal Agenesis (Ohvira Syndrome)
3104
Views & Citations2104
Likes & Shares
Introduction: We have present two cases of Obstructed Hemivagina with Ipsilateral Renal Agenesis (OHVIRA), that commonly known as Herlyn-Werner-Wunderlich syndrome, with transabdominal ultrasonography and Magnetic Resonance Imaging (MRI) findings. The patient with surgery and their imaging results were verified. The use of MRI has proven to be quite useful in determining the accurate diagnosis and avoiding the need for surgical operations or laparoscopy, which were previously required to diagnose this unusual defect.
Case Series: Case 1: An unmarried female was admitted to our casualty with complaints of acute pain in lower abdomen. A mass was palpable in left iliac fossa. Patient was sent to Radio diagnosis Department for transabdominal ultrasonography and based on its findings MRI of abdomen and pelvis was advised.
Case 2: A young female with complaints of amenorrhea for 2 months and acute pain in lower abdomen was admitted in our hospital. In view of negative pregnancy test, she was sent for transabdominal ultrasonography and then patient was advised for MRI abdomen and pelvis based on its findings.
Conclusion: OHVIRA Syndrome is a rare congenital urogenital anomaly. It has variable presentation and imaging plays a crucial role in its diagnosis and management. MRI plays a crucial role in diagnosis as it is difficult to diagnose this case and its complications clinically. MRI also disposes the use of surgical interventions or laparoscopy otherwise needed for diagnosis.
Keywords: Uterus didelphys, Hemivagina, Renal agenesis, Congenital, OVHIRA
INTRODUCTION
OHVIRA is a rare Mullerian duct anomaly characterized by uterus didelphys, unilateral obstructed hemivagina, and ipsilateral renal agenesis. After menarche, patients with this disease typically suffer pelvic pain and/or a mass and primary infertility is uncommon in later years. A patient usually appears with nonspecific symptoms following menarche& identification is often delayed until acute complications occur [1]. For a proper diagnosis, a thorough understanding and awareness of this unusual condition is required. The prevalence of common uterine abnormalities has been estimated to be between 7% and 10% in the overall female population [2]. In the general population, the incidence ranges from zero-point one percent to three-point eight percent, with 2/3rd of the subjects having uterine duplication along with complete vaginal septum [3]. Complex urogenital abnormalities, on the other hand, are frequently overlooked and misdiagnosed, resulting in delayed treatment. The Herlyn-Werner-Wunderlich (HWW) syndrome is an uncommon & underdiagnosed female urogenital tract developmental defect that comprises uterus didelphys and OHVIRA [1,3]. Only a few OHVIRA variations are known, including septate uterus or uterus didelphys, as well as ipsilateral renal anomalies [4].
OVHIRA disease is one of the less well-known urogenital anomalies, with a high rate of misdiagnosis. Infertility, repeated pregnancy loss, and poor pregnancy outcomes are all common symptoms [2]. Diagnostic imaging is used to guide treatment, reduce acute problems& restore fertility [3]. Diagnosis is difficult and crucial. The key to recognizing the anomaly quickly and avoiding problems is to have a high level of clinical suspicion. This uncommon congenital condition should be known by gynecologists and radiologists, and “OHVIRA” should always be considered as a differential diagnosis. We provide a case series of unusual OHVIRA syndrome variations with a clinical and radiological spectrum comparable to OHVIRA syndrome, who presented with primary infertility, abdominal pain, and a tumor palpable in the vaginal canal on examination. This is the first time a case series like this has been described in this area.
CASE SERIES
Case I:
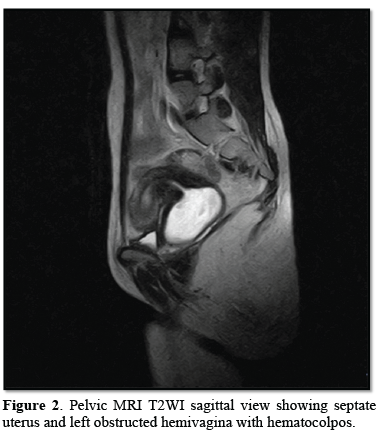
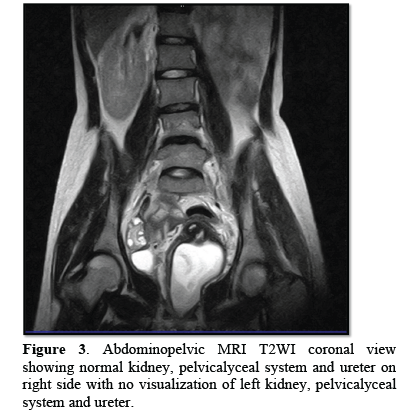
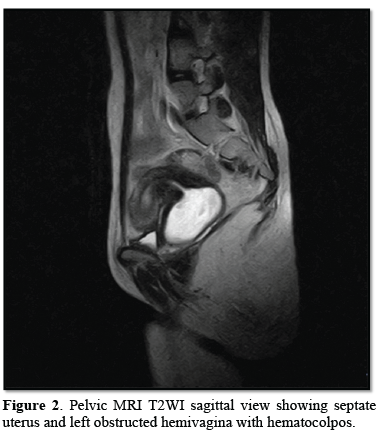
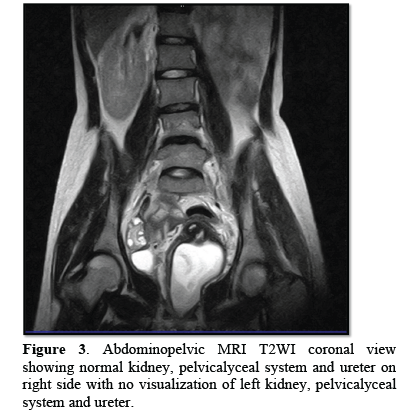
18 year’s old unmarried female was admitted in our casualty with complaints of acute abdomen. Acute onset in pain which was moderate in intensity, continuous without any relieving or aggravating factors mainly localized in the lower abdomen and associated with vomiting. Her previous menstrual cycle was 3-4/28-30 days with complaints of dysmenorrhea and LMP was two weeks back. She was stable and there was no pallor. Her pulse was 84 bpm, BP- 110/80 mmHg, RR- 20/min. On examination, there was slight tenderness and an ill-defined mass felt in left iliac fossa with rebound tenderness. On speculum examination, cervix was flushed with vagina; bulge is seen right vaginal wall. A cystic non-tender mass felt in right fornix with restricted mobility projecting in vagina on bimanual examination. So, possibility of appendicular lump or left TO mass was kept. Blood investigations were normal. Urine pregnancy test (UPT) was negative. Transabdominal ultrasonography showed septated uterus, cervix and vagina with non-visualization of left kidney. A cystic mass showing internal echoes on the left side of vagina and a septate uterus with blood in the cavity was noted. On MRI abdomen and pelvis, a complete septate uterus with haematocolpus of left hemivagina with absent left kidney and solitary right kidney showing hypertrophy was noted i.e., OHVIRA syndrome (Figures 1-3).


Case II:
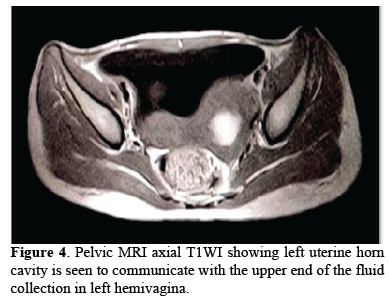
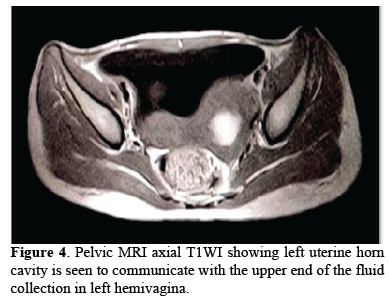
A 17 years old female was admitted in our emergency with acute abdomen complaints. She was unmarried and her previous menstrual cycle was normal. She gave history of amenorrhea for past two months and her UPT was negative. General physical examination was unremarkable. Mild tenderness was noted in lower abdomen without any rigidity or muscle guarding on per abdominal examination. On per vaginum examination, an ill-defined tender, cystic mass was felt in lower abdominal wall with restricted mobility and without cervical motion tenderness. So, possibility of ectopic pregnancy was kept and further investigation was advised. Transabdominal ultrasonography showed separate divergent uterine horns (Figure 4), with left sided hematocolpus (Figure 5) and left renal agenesis suggestive of OHVIRA syndrome. MRI confirmed the diagnosis. Her postoperative period was uneventful. On further follow up she had normal menstrual cycle and on examination there was no evidence of hematocolpus.


DISCUSSION
This syndrome was first described in 1922 and is now known as HWW syndrome or, more recently, OHVIRA. The incidence has been observed to range from 0.1 to 3.8 percent in various case studies [5]. OHVIRA syndrome is most frequently linked with uterine didelphys or, less frequently, a septate uterus [6]. The most prevalent urologic defect in OHVIRA syndrome is renal agenesis, however other anomalies such as renal duplication &multisystem dysplastic kidney was observed too [7,8]. The age at diagnosis in a reported group of 27 individuals ranged from ten-twenty years old (Median: 14) [9]. Menarche is generally accompanied by nonspecific symptoms such as recurrent pelvic discomfort or dysmenorrhea caused by increasing distension of the blocked hemivagina. Timelycorrect diagnosis is critical because quick treatment can alleviate the problem, prevent additional consequences from chronic obstructed hematocolpos and preserve reproductive potential. Improper information of the condition, frequent menstruations in the context of an incomplete vaginal outlet obstruction, and delayed hematocolpos expansion were all cited for the delays in diagnosis. The kidneys and ureters were thought to develop from Zolffin pro/meso/metanephros, while the uterocervical development was thought to be from paired paramesonephric ducts. Various uterine abnormalities were successfully explained by abnormal vertical or horizontal fusion or stoppage of paramesonephric ducts during formation. Complicated uterine defects viz. OHVIRA syndrome, eluded standard urogenital development theories until recently, when the Acien theory of complete vaginal formation from mesonephric channels was proposed [2]. Following Acien's proclamation, vaginal embryonic development has been a heated topic of controversy. The traditional approach was proven to be insufficient in understanding complex defects like OHVIRA, as well as their conjunction with renal anomalies. While the uterus and cervix were developed from the uterus, Acien suggested that the uterus and cervix were derived from the cervi, with fused-paired paramesonephric ducts (2nd part) and divergent distal paramesonephric ducts (3rd part), though it’s lining revealed mullerian cells derived from mullerian tubercle. As a result, paramesonephric ducts do not contribute to the creation of the vagina, however mullerian tubercle does, resulting in mulleria tubercle cells lining the vagina.
Sánchez's findings from his research with female rats utilizing his to immunochemistry techniques have bolstered his theory. Agenesis of the ureteric bud, which leads to agenesis of the ipsilateral ureter and kidney, occurs when the metanephric diverticulum fails to grow (around 5 weeks) from the mesonephric duct. Sonography is frequently utilized as the first imaging modality for suspected Müllerian duct abnormalities. Because of its multiplanar capability, greater tissue characterization, and extensive field of view, MR imaging is a good technique for examining the usually complex Müllerian duct anomalies. The uterine contour, shape of the uterine cavity, and concomitant cervical and vaginal anomalies may all be accurately depicted by MR imaging, which is helpful in the classification of Müllerian duct anomalies and surgical planning. Furthermore, MR imaging can quickly detect any concurrent renal and/or urethral abnormalities, as well as define the contents of occluded cavities (for example, simple fluid vs. blood). The primary treatment for OHVIRA syndrome is surgical intervention in the form of vaginal septum resection to remove blockage. It is possible to perform a one-stage vaginoplasty, which involves total excision of the septum in a single treatment. Due to retrograde menstrual seeding, surgery reduces the risk of pelvic endometriosis. No complaint was found among the subjects w.r.t. coitus.
CONCLUSION
We concluded that OHVIRA syndrome is an uncommon congenital urogenital defect with a wide spectrum of clinical manifestations but having straightforward surgical treatment. Imaging specially MRI is critical in making a diagnosis that is frequently missed clinically. Without the aid of imaging, it has been difficult to appropriately diagnose the intricate Müllerian defects. Appropriate surgery is a single-stage operation that removes or divides the obstructive septum completely. Retrograde menstruation can cause endometriosis and infertility, therefore it's important to get a proper diagnosis as soon as possible to alleviate symptoms and avoid consequences like endometriosis and infertility, as well as protect sexual and conception capacities. It is necessary to be aware; otherwise, misdiagnosis is very likely. To avoid difficulties and obtain a better outcome, a multidisciplinary approach must be led by a gynecologist.
CONFLICT OF INTEREST
No funding for the study was received from any agency. The study was entirely financed by the authors themselves. All the authors declare no interfering conflict of interest.
AUTHOR’S CONTRIBUTIONS
Sachin Khanduri
GROUP 1: Conception and design of the work and Acquisition, analysis and interpretation of data
GROUP 2: Drafting and revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Shivangi Katara
GROUP 1: Conception and design of the work and Acquisition, analysis and interpretation of data
GROUP 2: Drafting and revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Mariyam Fatima
GROUP 1: Acquisition of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Kushagra
GROUP 1: Acquisition of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Sonal Kaushik
GROUP 1: Analysis of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Sana Fatima
GROUP 1: Analysis of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Rahul Kumar
GROUP 1: Analysis of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
ACKNOWLEDGEMENTS
The authors are thankful to Vice Chancellor, Era’s Lucknow Medical College and Hospital, Lucknow for granting permission to carry out this study.
- Piccinini PS, Doski J (2015) Herlyn-Werner-Wunderlich syndrome: a case report. Rev Bras Ginecol Obstet 37: 192-196.
- Acién P, Acién M, Sánchez-Ferrer M (2004) Complex malformations of the female genital tract. New types and revision of classification. Hum Reprod 19: 2377-2384.
- Orazi C, Lucchetti MC, Schingo PM, Marchetti P, Ferro F (2007) Herlyn-Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol 37: 657-665.
- Surya M, Thakur S, Singh K, Soni P, Sood D, et al. (2016) Complete septate uterus with obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) in a young woman-a rare variant of Herlyn-Werner-Wunderlich syndrome. BJR Case Rep 2: 20150241.
- Heinonen PK (2000) Clinical implications of the didelphic uterus: long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol 91: 183-190.
- Smith NA, Laufer MR (2007) Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: Management and follow-up. Fertil Steril 87(4): 918-922.
- Li S, Qayyum A, Coakley FV, Hricak H (2000) Association of renal agenesis and Mullerian duct anomalies. J Comput Assist Tomogr 24: 829-834.
- Wang J, Zhu L, Lang J, Liu Z, Sun D, et al. (2014) Clinical characteristics and treatment of Herlyn-Werner-Wunderlich syndrome. Arch Gynecol Obstet 290: 947-950.
- Zurawin RK, Dietrich JE, Heard MJ, Edwards CL (2004) Didelphic uterus and obstructed hemivagina with renal agenesis: Case report and review of the literature. J Pediatr Adolesc Gynecol 17: 137-141.
- Acién P (1992) Embryological observations on the female genital tract. Hum Reprod 7: 437-445.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Spine Diseases
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Oncology Clinics and Research (ISSN: 2643-055X)
- Journal of Immunology Research and Therapy (ISSN:2472-727X)






