Research Article
Study of Iron Profile in Repeat Voluntary Blood Donors: An Experience of a Tertiary Care Hospital-Based Blood Centre
4571
Views & Citations3571
Likes & Shares
Background and Objectives: Donating 350-450 mL of blood four times a year is equivalent to loss of 2.2 mg of iron per day which is more than the normal daily absorbed iron for men and women and results in fall of hemoglobin (Hb) after 3 days of donation. Measurement of Hb, though, an easy and inexpensive way, is a poor indicator of reduced iron stores and iron deficient erythropoiesis (IDE) because anemia occurs as the last stage in this sequence. The purpose of this study is to evaluate the iron status of repeat voluntary blood donors using combination of hematological and biochemical parameters and to assess the influence of frequency and duration of inter donation interval on iron stores.
Methods: A prospective cross-sectional study was carried out for assessment of complete blood count (CBC) including Hb estimation, Serum Iron, Serum Ferritin, Total Iron Binding Capacity (TIBC) in human serum/whole blood on all 288 repeat voluntary donations performed from July 2017 to June 2019, fulfilling the donor eligibility criteria for whole blood donations, as an additional test apart from the mandatory transfusion transmitted tests.
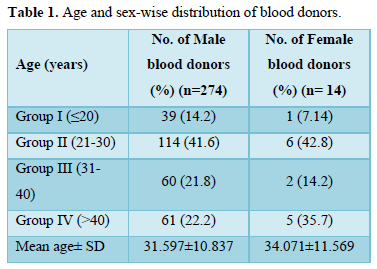
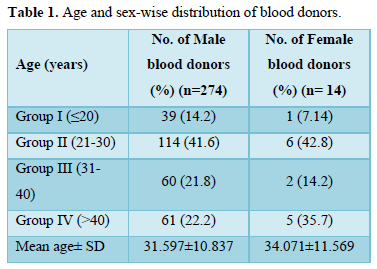
Results: A total of 288 donors were tested during this period with mean age 32.83 years with 95.13% (274) male donors. Reduced iron stores were found in 34 (11.8%), iron depleted erythropoiesis in 20 (6.95%) and iron deficiency anemia in 20 (6.95%) donors, who were sub grouped as per frequency of donation, last donation interval and age distribution.
Conclusion: Donors need to be educated about iron deficiency and those who have donated more than twice should be put on regular iron supplementation to prevent the iron store depletion. A policy for investigation and management of iron deficiency anemia needs to be incorporated as a regular routine procedure in blood transfusion services.
Keywords: Iron stores, Repeat, Voluntary blood donors
Abbreviations: Hb: Hemoglobin; IDE: Iron Deficient Erythropoiesis; CBC: Complete Blood Count; TIBC: Total Iron Binding Capacity; NACO: National AIDS Control Organization; NBTC: National Blood Transfusion Council; MCV: Mean Corpuscular Volume (MCV); MCH: Mean Corpuscular Hemoglobin; MCHC: Mean Corpuscular Hemoglobin Concentration; S. Iron: Serum Iron; S. Ferritin: Serum Ferritin
INTRODUCTION
WHO defines a regular voluntary non-remunerated blood donor as one who has donated at least three times, the last donation being within the previous year, and continues to donate regularly at least once per year. According to the recent recommendations of NACO/NBTC, a healthy individual with hemoglobin (Hb) levels ≥12.5g/dl can donate blood at the interval of 3 months (in case of male donor) and at the interval of 4 months (in case of female donor). It has been seen that iron stores can get depleted if blood is donated more frequently. In developing countries such as India, established blood supplies are limited and donors usually give blood when family or friends need transfusion [1]. Blood donation is the most common cause of iatrogenic iron deficiency among healthy adults [2] and iron deficiency is the most common cause of anemia and one of the main factors in the clinical deferral of blood donors and hence results in shrinkage of donor pool. Measurement of Hb, though, is an easy and inexpensive way to rule out anemia in donors, is a poor indicator of reduced iron stores and IDE because anemia occurs as the last stage in this sequence [3]. Such routine methods do not reflect on the status of iron stores of an individual and provide no indication of the development of iron depletion. Therefore, more specific tests like serum ferritin, serum iron, TIBC, Transferrin saturation are required to identify the iron status of the donors [4]. The purpose of this study is to evaluate the iron status of repeat voluntary blood donors using combination of hematological and biochemical parameters and assess the influence of frequency and duration of inter donation interval of blood donation on iron stores of the donor.
MATERIALS AND METHODS
A prospective cross-sectional study was conducted at a blood center attached with a tertiary care hospital in western India between July 2017 to June 2019, among healthy repeat voluntary blood donors of 18 to 65 years of age and in good health, fulfilling the eligibility criteria for whole blood donation in accordance to the D&C Act 1940 and rules 1945 therein (as amended on 11th March 2020). Donors were further sub grouped on the basis of frequency of donation into four groups (A to D)
- Group A: who donated 1 to 5 times in last 2 years
- Group B: who donated 6 to 10 times in last 3 years
- Group C: who donated 11 to 15 times in last 4 years
- Group D: who donated more than 15 times
The time period of 2 years, 3 years, 4 years in Group A, B and C respectively was taken to compare period-matched donors and avoid any bias. On the basis of inter donation interval into four groups (1 to 4); Group 1: inter donation interval of 3 months; Group 2: inter donation interval of >3-6 months; Group 3: inter donation interval of >6-9 months; Group 4: inter donation interval of >9 months. On the basis of age distribution into four groups (I to IV); Group I: ≤ 20 years; Group II: age between 21-30 years; Group III: age between 31-40 years; Group IV: age >40 years. After obtaining consent from the donors, venous blood sample was collected in tube containing anticoagulant K3EDTA for the analysis of Hb and other hematological parameters i.e., MCV, MCH and MCHC and in tube containing clot-activator for blood chemistry analysis related to iron profile. All the samples were tested within 12 hours of collection. For CBC including Hb estimation, a fully automated cell counter analyzer (Sysmex KX-21 Cell Counter®) was used. Assessment of S. Iron, by TPTZ method, and TIBC by saturation/precipitating method, was done using a fully automated analyzer (BECKMEN COULTER AU480 Chemistry Analyzer®). S. Ferritin levels were screened on automated analyzer (BECKMEN COULTER UniCel Dxl 800 Access Immunoassay System®) using Chemiluminescent Immunoassay. Statistical calculations were performed using the SPPS 16.0. In order to detect differences between subject’s student’s t-test was used for continues variables, while, for categorical variables, the χ² test (Chi-square) was used. A p-value of less than 0.05 was considered statistically significant.
RESULTS
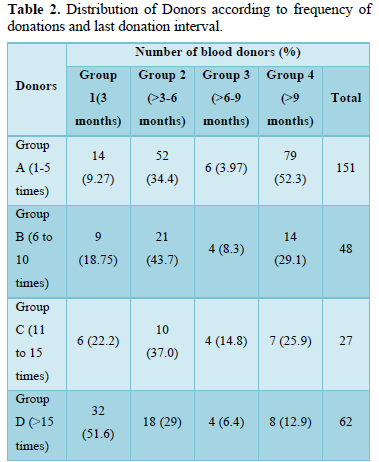
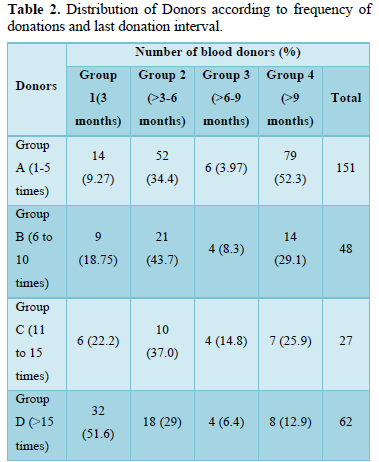
Between July 2017 to June 2019, 288 repeat voluntary blood donors were recruited for the study, 274 (95.13%) of whom were male and 14 (4.861%) were female. The Age and sex-wise distribution of blood donors is shown in Table 1. The donors were further sub grouped on the basis of frequency of donations and last donation interval, as shown in
Table 2. The results of the tests for iron profile were compared against the following values:
- Ferritin: 21.81-274.66 ng/mL (for male)
4.63-204 ng/mL (for female)
Evaluation of iron stores is done as below:
Reduced at S. Ferritin values: Between 15-20 ng/mL
IDE at S. Ferritin values: 12 ng/mL
Iron Deficient Anemia at S. Ferritin values:
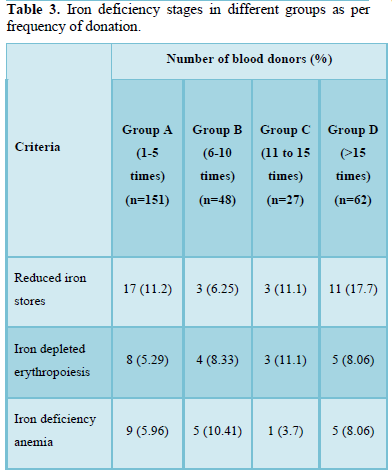
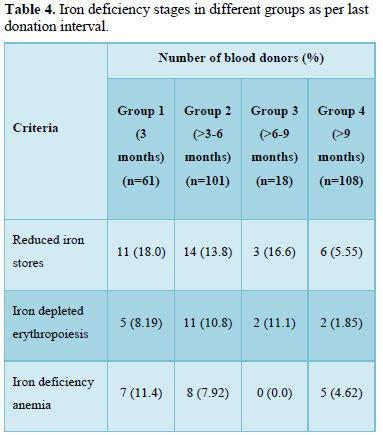
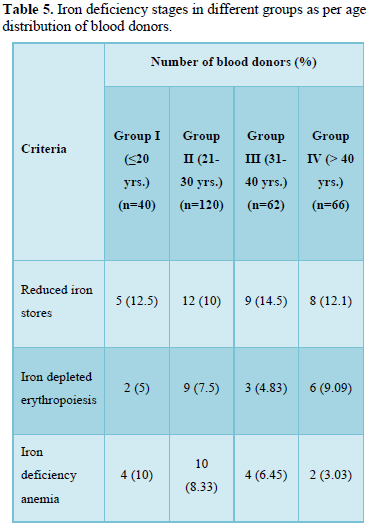
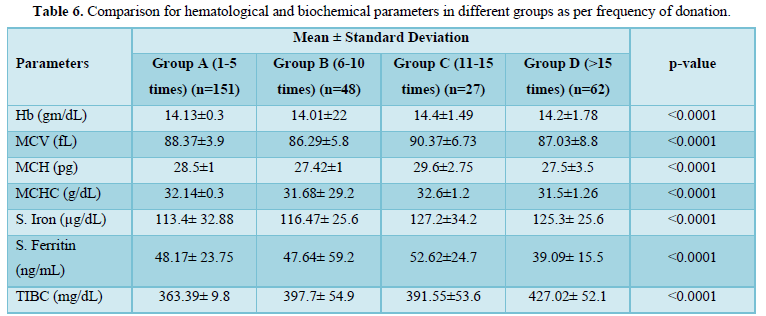
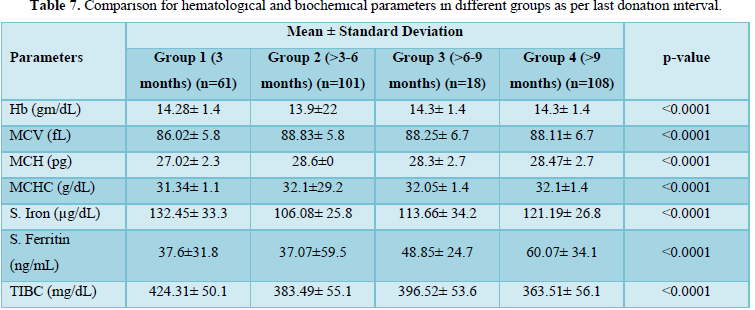
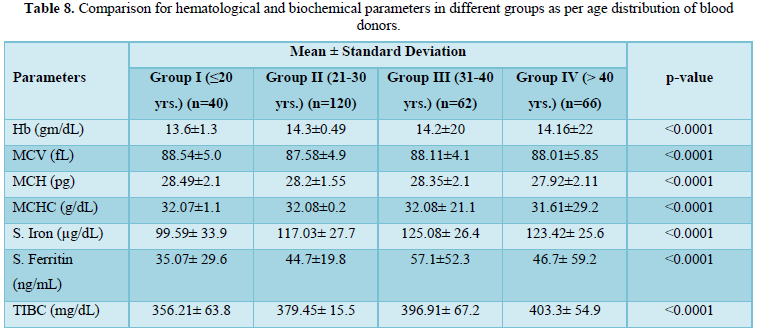
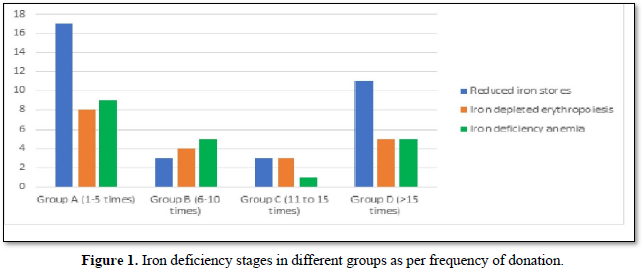
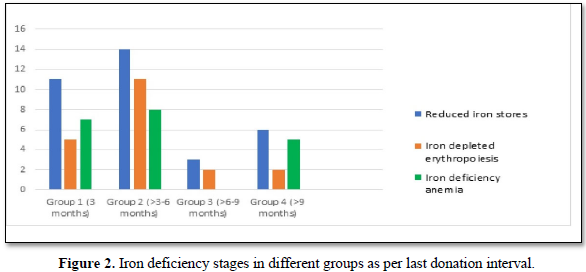
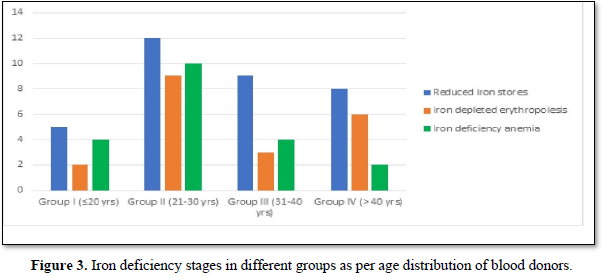
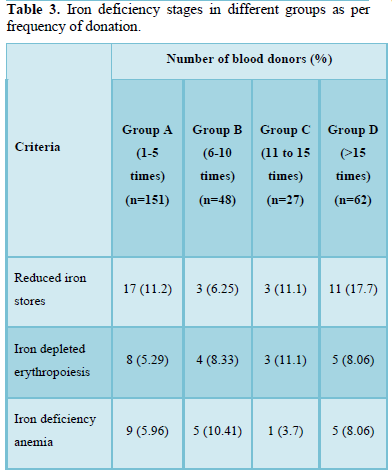
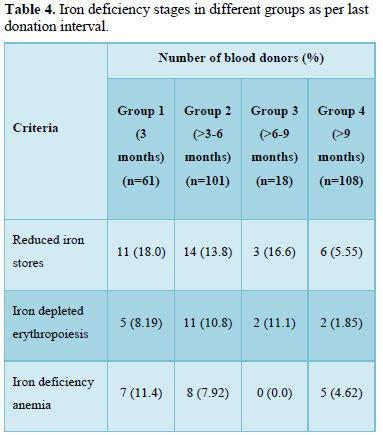
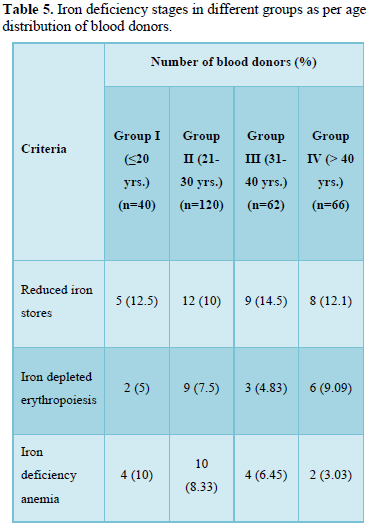
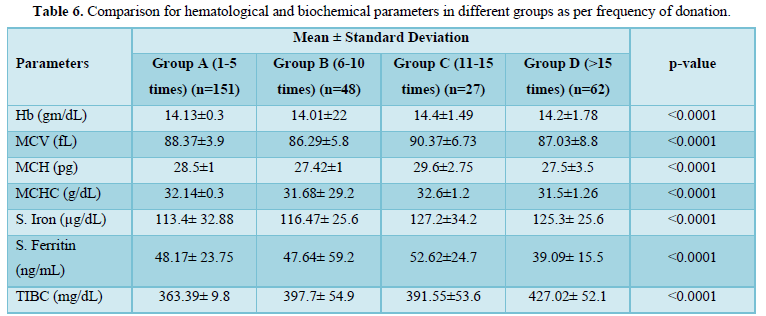
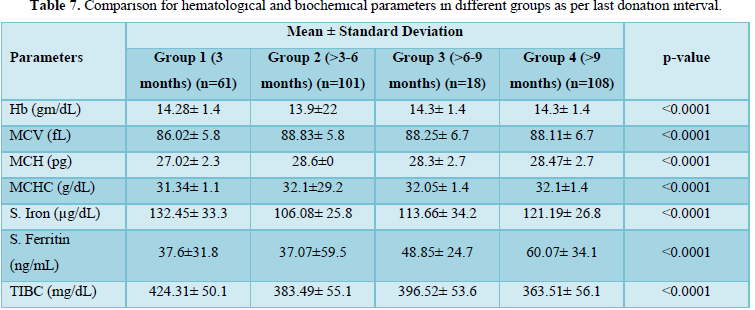
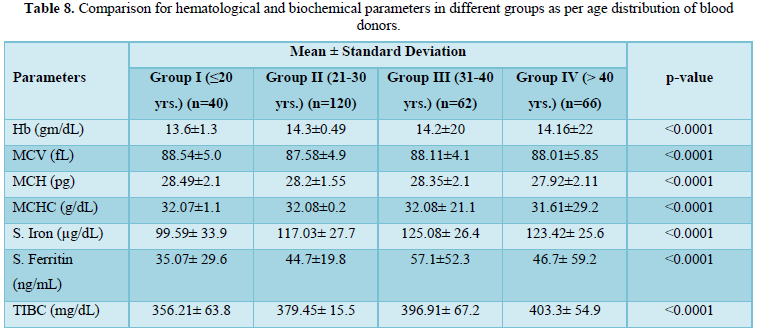
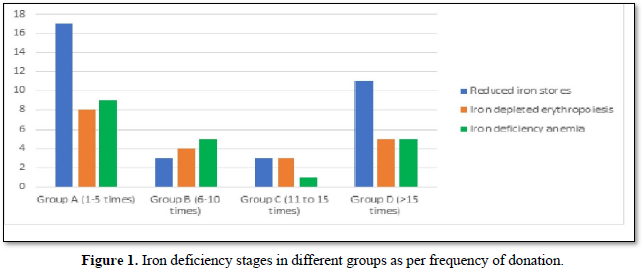
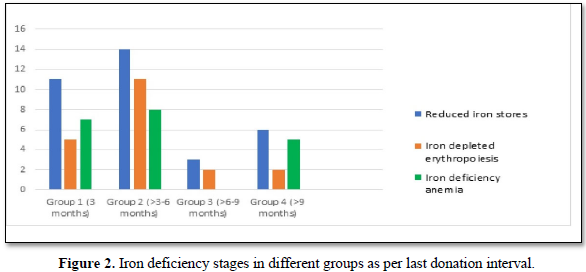
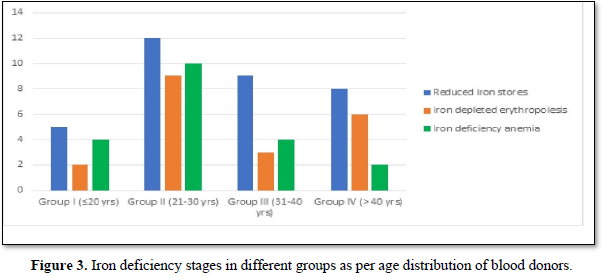
Iron deficiency stages in blood donors sub grouped on basis of frequency of donation is shown in Table 3. As shown in Figure 1, 34 (11.8%) donors were found to have reduced iron stores, 20 (6.94%) were having IDE and 20 (6.94%) were found to have Iron deficiency anemia. Iron deficiency stages in blood donors sub grouped as per last donation interval is shown in Table 4 and Figure 2. Table 5 and Figure 3 shows iron deficiency stages in donors sub grouped on basis of age distribution. Comparison for hematological and biochemical parameters of blood donors sub grouped as per frequency of donation is shown in Table 6, as per last donation interval is shown in Table 7 and as per age distribution is shown in Table 8.
DISCUSSION
The adequate and quality supply of blood depends on the health status of blood donors. Although, repeated regular blood donation is considered a good donation and in order to fulfill the necessities, blood centers find it more effective to collect blood from existing donors than to recruit new donors but this strategy leads to iron depletion of these donors [5]. In our study, the Hb level was above the normal cut off value for blood donation in all the blood donors, including the ones who were later found to have reduced iron stores. In our study, the mean Hb level in all the donors was 14.178 g/dL. However, the Hb levels varied significantly among the donors depending on the duration of last donation. All our results have been compared with the data from other published articles from India and abroad. It is clear from the Table 6 that the donors of Group C have higher levels of Hb, MCV, MCH, MCHC, S. Iron and S. Ferritin as compared to donors of other groups. The mean value of S. Iron and TIBC increased as the frequency of donation increased. The highest levels with respect to all the biochemical parameters except TIBC are seen in donors of Group C followed by donors of Group A and Group D having lowest level of S. Iron and S. Ferritin respectively. TIBC is seen to show inverse relation with frequency of donation. The variation of parameters among the group is statistically significant as the p value is less than 0.0001. The data presented in the Table 7 shows the mean Hb, MCV, MCH, MCHC, S. Iron, S. Ferritin, and TIBC in different groups as per last donation interval. It is clear from Table 7 that the donors of Group 4 have higher levels of Hb, MCV, MCH and S. Ferritin as compared to donors of other groups. The variation of parameters among the group is statistically significant as the p value is less than 0.0001. The data presented in the Table 8 shows the mean Hb, MCV, MCH, MCHC, S. Iron, S. Ferritin, and TIBC in different groups as per age distribution of the blood donors. It is clear from Table 8 that the donors of Group III have higher levels of S. Iron and S. Ferritin as compared to donors of other groups. The mean value of S. Iron, S. Ferritin and TIBC increased as the age distribution of donors increased. The highest levels with respect to all the biochemical parameters except TIBC are seen in donors of Group III followed by donors of Group IV and Group II, and Group I having lowest level of S. Iron and Ferritin respectively. The variation of parameters among the group is statistically significant as the p value is less than 0.0001. There is a significant relation of hematological parameters including MCV, MCH with increased frequency of donation, consistent with other study from North India [6] in which MCV, MCH dropped significantly in relation to annual donation frequency. Among the biochemical tests for iron stores, S. Ferritin is considered as a reliable indicator of iron status in blood donors. S. Ferritin alone or in combination with other tests are helpful in assessing the iron status of the blood donors [7]. In the present study, mean S. Ferritin concentration of 46.54 ng/mL was recorded amongst donors. As clearly seen from Figure 4, the mean value of S. Ferritin dropped significantly in donors as the frequency of donation increased proving the influence of the number of donations on serum ferritin levels. The result of our study showed 34 (11.8%) of repeat blood donors had reduced iron stores (S. Ferritin 15-20 ng/mL), 20 (6.94%) of repeated blood donors had IDE (S. Ferritin 12-15 ng/mL) and 20 (6.94%) of the donors had iron deficiency anemia (S. Ferritin Table 3 and Figure 1 shows the iron deficiency stages in different donor groups as per frequency of donation. From the data obtained it is evident that amongst all four groups, maximum number of donors, who had reduced iron stores (17), iron depleted erythropoiesis (8) and iron deficiency anemia (9) belong to Group A followed by donors of Group D where donors had reduced iron stores (11), iron depleted erythropoiesis (5) and iron deficiency anemia (5). Iron deficient erythropoiesis was seen in donors who donated blood 1-5 times (n= 17) and was more than in donors who donated more than 15 times (n=62). Analysis of the data presented in Table 4 and Figure 2 shows the iron deficiency stages in different donor groups as per last donation interval. From the data obtained it is evident that amongst all four groups, maximum number of donors, who had reduced iron stores (14), iron depleted erythropoiesis (11) and iron deficiency anemia (8) belong to Group 2 followed by donors of Group 1 where donors had reduced iron stores (11), iron depleted erythropoiesis (5) and iron deficiency anemia (7). Analysis of the data presented in Table 5 and Figure 3 shows the iron deficiency stages in different donor groups as per age distribution of blood donors. From the data obtained it is evident that amongst all four groups, maximum number of donors, who had reduced iron stores (12), iron depleted erythropoiesis (9) and iron deficiency anemia (10) belong to Group II followed by donors of Group III and IV where donors had reduced iron stores (9; 8), iron depleted erythropoiesis (3; 6) and iron deficiency anemia (4; 2). Iron depletion is the earliest stage of iron deficiency, and signifies that iron stores are decreased or absent, but the serum iron concentration and blood hemoglobin levels are normal. Iron deficiency without anemia is somewhat more advanced stage of iron deficiency, characterized by decreased or absent iron storage, usually a low serum iron concentration and low blood hemoglobin concentration, but without anemia [8]. Our study showed direct relationship of serum iron, ferritin with number of blood donation and direct relation with TIBC levels i.e., TIBC levels are increased with increasing donation number. There was a significant correlation between inter-donation and last donation interval with serum ferritin levels. This finding was consistent with previous studies [9,10] in which the S. Ferritin levels were significantly lower in regular donors and female donors. In a similar study, reviewing of screening criteria used at the time of donation and inclusion of S. Ferritin measurement in the assessment of regular blood donors to secure adequate iron reserves in the donor population was recommended [11]. A study recommends measurement of S. Ferritin levels after five donations to help identify iron deficient individuals [12]. In a study, it was concluded that the introduction of routine S. Ferritin analysis resulted in an increase of mean Hb levels in blood donors particularly in women of childbearing age. The incidence of pre donation anemia and donation ineligibility due to a low Hb concentration decreased significantly. The return intervals of donors rejected on account of low Hb levels were also shortened. Therefore, early detection of iron deficiency and anemia among blood donors would allow appropriate re-adjustment of donation intervals and would guide the use of iron supplementation to prevent the development of iron deficiency anemia in the donors thereby preventing shrinking of donor pool [13]. In fact, a study demonstrated that only 25% of first-time donors return to the blood donation facility after rejection, while 47% of first-time donors come back within 6 months when accepted at their first visit [14]. One promising approach involves administration of carbonyl iron rather than ferrous sulfate, a formulation that is well tolerated by most individuals [15].
CONCLUSION
According to the results obtained from our study, a total of 74 (25.69%) repeat voluntary blood donors were found to be having depleted iron stores and thus, it can be concluded that as the blood donation frequency increases, the S. Ferritin and S. Iron decreases significantly. Hb measurement alone is not enough to evaluate donor suitability, especially in regular blood donors. Also, shorter the inter donation interval, greater the chances of iron depletion. Current guidelines for blood donation i.e., Hb levels ≥ 12.5 g/dL does not reflect true iron status of the blood donor. Therefore, more sensitive tests like S. Iron and S. Ferritin in blood donors are important markers. Donors need to be educated about iron deficiency and recommended iron rich diet which can be easily available. Those who have donated more than twice should be put on regular iron supplementation to prevent the iron store depletion. In fact, a policy for investigation and management of iron deficiency anemia needs to be incorporated as a regular routine procedure in blood transfusion services. The results provide an insight into the importance of monitoring the iron status of regular repeat donors, thereby, ensuring best of health care to donors and maintaining a regular pool of donors. Now, that the guidelines lay more stress and emphasis on regular repeated voluntary non-remunerated blood donations, our criteria for donor pre-donation testing needs to be revisited.
- Amilo GI, Ifeanyichukwu MO, Ngwu AM, Obi GO (2014) Iron deficiency in regular blood donors in Enugu (Southeastern Nigeria). Int J Blood Transfus Immunohematol 4: 1-6.
- Nadarajan VS, Eow GI (2002) Anemia and iron status among blood donors in a blood transfusion unit in Malaysia. Malays J Pathol 24(2): 99-102.
- Suominen P, Punnonen K, Rajamäki A, Irjala K (1998) Serum transferrin receptor and transferrin receptor-ferritin index identify healthy subjects with subclinical iron deficits. Blood 92(8): 2934-2939.
- Jeremiah ZA, Koate BB (2010) Anemia, iron deficiency and iron deficiency anemia among blood donors in Port Harcourt, Nigeria. Blood Transfus 8(2): 113-117.
- Popovsky MA (2012) Anemia, iron depletion, and the blood donor: It's time to work on the donor's behalf. Transfusion 52: 688-692.
- Dara RC, Marwaha N, Khetan D, Patidar GK (2016) A Randomized Control Study to Evaluate Effects of Short-term Oral Iron Supplementation in Regular Voluntary Blood Donors. Indian J Hematol Blood Transfus 32(3): 299-306.
- Kiss JE, Brambilla D, Glynn SA, Mast AE, Spencer BR, et al. (2015) Oral iron supplementation after blood donation: A randomized clinical trial. JAMA 313(6): 575-583.
- Alharbi SH, Alateeq FA, Ahmed IB, Alsogair ARAA, Al-Rashdi YDA, et al. (2018) Assessment of levels of awareness towards blood donation in Saudi Arabia. AIMS Public Health 5(3): 324-337.
- Moghadam AM, Natanzi MM, Djalali M, Saedisomeolia A, Javanbakht MH, et al. (2013) Relationship between blood donor’s iron status and their age, body mass index and donation frequency. Sao Paulo Med J 131(6): 377-383.
- Ali BH, Osaro E, Sani I, Wase A, Festus O, et al. (2015) Prevalence of iron deficiency anemia among blood donors in Sokoto, North Western, Nigeria. J Coast Life Med 3(4): 312-316.
- Tailor HM, Patel PR, Pandya AKNP, Mangukiya S (2017) Study of Various Hematological Parameters and Iron Status among Voluntary Blood Donors Int J Med Public Health 7(1): 61-65.
- Alvarez-Ossorio L, Kirchner H, Klüter H, Schlenke P (2000) Low ferritin levels indicate the need for iron supplementation: Strategy to minimize iron-depletion in regular blood donors. Transfus Med 10: 107-112.
- O'Meara A, Infanti L, Stebler C, Ruesch M, Sigle JP, et al. (2011) The value of routine ferritin measurement in blood donors. Transfusion 51(10): 2183-2188.
- Boulton F (2008) Evidence-based criteria for the care and selection of blood donors, with some comments on the relationship to blood supply, and emphasis on the management of donation-induced iron depletion. Transfus Med 18(1): 13-27.
- Reiss RF, Kessler D (2010) Current concerns for blood donor well-being and health. South Med J 103(4): 343-346.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)





