Research Article
A Clinical Study on Socio Demographic Co-Factors in Cancer Cervix in Women of Rural Haryana, North India
2950
Views & Citations1950
Likes & Shares
Cervical cancer is the commonest cancer of female genital tract in India with profound impact on the morbidity and mortality. This study was undertaken to understand the socio demographic factors affecting occurrence of cancer cervix among the rural population of Haryana, North India.
The study showcased a surprising lack of knowledge of cancer cervix and those many modifiable socio demographic factors were present which act as cofactors in cervical carcinogenesis.
Keywords: Cervical cancer, Carcinoma, HPV, Screening, Pap smear, Sociodemographic, Epidemiological
Abbreviations: CIN: Cervical Intraepithelial Neoplasia; CIS: Carcinoma in Situ; HPV: Human Papilloma Virus; HIV: Human immune Virus; AIDS: Acquired Immunodeficiency Syndrome
INTRODUCTION
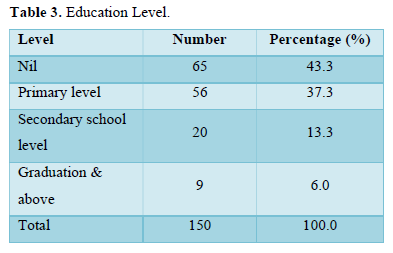
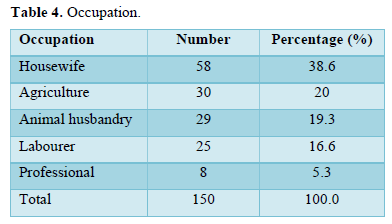
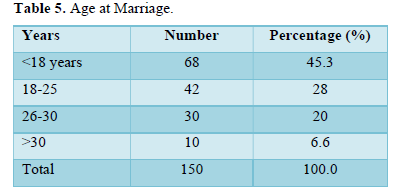
India is the second most densely populated country in the world. Cervical cancer is the most common cancer of female genital tract and fourth most common cancer in females overall after breast, colorectal and lung [1,2]. Many sociodemographic factors like poverty, lack of education and health awareness, early age at marriage, repeated childbirths, lack of proper hygiene and proper education have been linked to the high incidence of cancer and morbidity and mortality associated with the same [1,3,4]. It has been established that incidence of cervical cancer increases with increasing age, number of childbirths and prolonged period of sexual intercourse [1,3,4]. Cancer cervix is often referred to as a cancer of the poor, uneducated and undeserved [4], mostly because women coming from poor and uneducated social background often have no or less awareness about health education, wellbeing and less likely to avail routine checkup and screening [1,9-11].
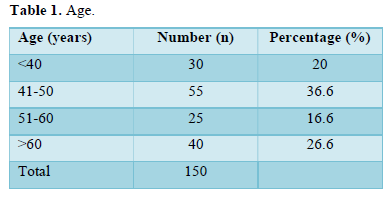
Early age at first sexual intercourse and prolonged duration of sexual intercourse is directly proportional to development of cervical cancer [1]. Environmental co-factors depend on the socioeconomic condition of the patient e.g., early age at marriage and first childbirth and multiple childbirths, poverty, poor hygiene, active and passive smoking, oral contraceptive pills use is important in cervical carcinogenesis. Other factors e.g., multiple sexual partners, HIV/AIDS, HPV infections.
MATERIALS AND METHODS
- Aim of the study: To evaluate the sociodemographic co factors on cervical cancer in the rural population of Haryana, in North India.
- Study Period: Jan 2018- Jan 2021
- Study Duration: 3 years
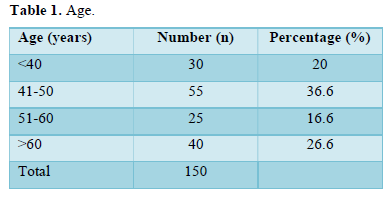
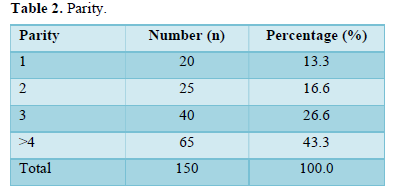
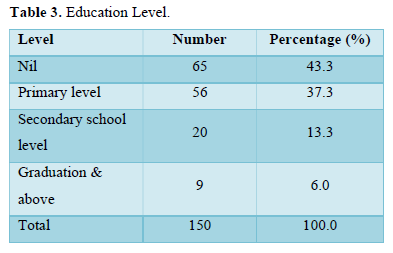
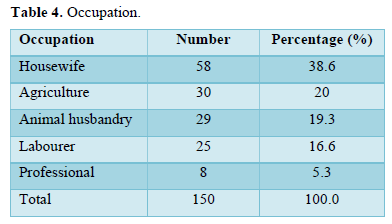
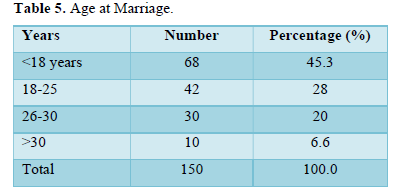
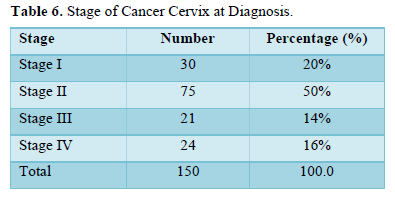
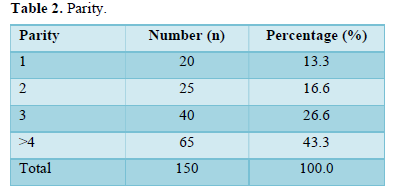
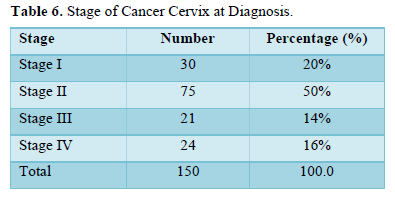
A total of 150 patients of histopathologically diagnosed carcinoma cervix were encountered in the said study period. All the data regarding the patients’ particulars especially the socio-demographic factors eg age, parity, socio-economic status, education, age at marriage and first pregnancy, occupation and stage of the disease at diagnosis were collected, tabulated and statistically analyzed.
RESULTS AND OBSERVATION
The results and observations were as follows (Tables 1-6):
- Socio Demographic Variables
Table 1. Age.
DISCUSSION
Globally Cancer Cervix accounts for 12% of all female cancers, but is the commonest female genital cancer in India [1,2]. Cancer Cervix has a prolonged precancerous stage which gives us a golden opportunity to use for screening for the disease even before the frank cancer has occurred. Also, diagnosis at an early-stage results in better prognosis and 5-year survival rate of the patients. In our study we observed most of the patients belonged to lower and lower middle-income group, rural population, uneducated, married at early age (4), had active and passive smoking exposure with tobacco, used no contraception, didn’t undergo screening tests for cancer cervix. These observations tallied with those from various other studies from the Indian sub-continents, India, Bangladesh, Nepal and Pakistan [1-3,6,7,9,10]. Cancer cervix is rightly referred to as the ‘cancer of poor, uneducated and undeserved’. Most cases were diagnosed at advanced stages of the disease (III and IV). This can be attributed to the lack of health awareness and proper and easy access to screening methods and health facilities [11,15-19]. Often it is seen that incomplete and improper knowledge about the disease leads to improper diagnosis and treatment especially in the hands of inexperienced, underqualified and unqualified practitioners increasing the likelihood of mistreatment and undertreatment of the disease so that in the meantime crucial time is lost and most of the patients came at advanced stages of cancer cervix with poor prognosis.
CONCLUSION
This study helped us in understanding many sociodemographic factors which have an important bearing in cervical carcinogenesis. Some of these factors are easily modifiable and if addressed at the grass root level, will help in prevention, early diagnosis of cervical cancer which will ultimately help in reducing the burden of morbidity and mortality due to cervical cancer.
CONFLICT OF INTEREST
Nil.
FUNDING
None.
- Hussain M, Nigar T (2021) Socioeconomic factors in cervical cancer in Bangladesh. Sch Int J Obst Gynecol 4(3): 58-62.
- Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. (2015) The Global Burden on cancer 2013. JAMA Oncol 1(4): 505-227.
- Rajarao P, Kumar HB (2012) Study of Socio Demographic Profile of Cancer cervix patients in Tertiary Care Hospital, Karimnagar (Andhra Pradesh). Int J Bio Med Res 3(4): 2306-2310.
- Chauhan R (2016) A hospital-based study on clinical profile of cervical cancer patients in Bihar. 4: 21-23.
- Bhattacharya SK, Basu S, Banerjee S, Dastidar AG, Bagchi SR (2020) An epidemiological survey of Cancer Cervix in North Bengal Zone. J Indian Med Assoc 98(2): 60-61.
- Prakash KVB (2018) Cervical cancer in tertiary care center in Mysuru Karnataka. Int J Med Sci Public Health 4(9): 1187-1191.
- Young SD, Ramalingam HS (2020) Clinicopathological study of cervical cancer in Northeast India. 6: 64-66.
- Papri FS, Khanam Z. Ara S, Panna MB (2016) Adolescent Pregnancy: Risk Factors, Outcome and Prevention. Chattagram Maa-O-Shishu Hosp Med College J 14(2): 57-61.
- Juneja A, Sehgal A, Mitra AB, Pandey A (2013) A survey on risk factors associated with cervical cancer. Indian J Cancer 40(1): 15-22.
- Hammouda D (2015) HPV and lifestyle risk factors in genesis of cervical cancer. Int J Cancer 113(3): 483-489.
- Bosch FX, Lorincz A, Muñoz N, Meijer CJLM, Shah KV (2012) The casual relation between HPV & Cancer Cervix. J Clin Pathol 55(4): 244-265.
- Brinton LA, Hamman RF, Huggins GR, Lehman HF, Levine RS, et al. (2017) Sexual & Reproductive risk factors for invasive squamous cell cervical cancer J Natl Cancer Inst 79(1): 23-30.
- Muñoz N, Franceschi S, Bosetti C, Moreno V, Herrero R, et al. (2012) Role of parity and human papillomavirus in cervical cancer: The IARC multicentric case-control study. Lancet 359(9312): 1093-1101.
- Deacon JM, Evans CD, Yule R, Desai M, Binns W, et al. (2010) Sexual behavior & smoking as determinants of cervical HPV infection& CIN-3 among those infected: A case control study nested within the Manchester cohort. Br J Cancer 83(11): 1565-1572.
- Hicks ML (2019) Demographic differences in stage at diagnosis & cervical cancer survival in New Zealand. 1995-2015. J Women Health 18(7): 955-963.
- Brewer N (2016) Disparities in cervical cancer screening, Rx and outcomes. Ethnicity Dis 16(2): 53.
- Berraho M, Obtel M, Bendahhou K, Zidouh A, Errihani H, et al. (2012) Sociodemographic factors and delay in the diagnosis of cervical cancer in Morocco. Pan Afr Med J 12: 14.
- Ibrahim A, Rasch V, Pukkala E, Aro AR (2011) Predictors of cervical cancer being at an advanced stage at Dx in Sudan. Int J Womens Health 3: 385-389.
- Mayor S (2016) A quarter of patients with cancer see their GP several times before being referred. BMJ 352: i1198.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)

