2307
Views & Citations1307
Likes & Shares
Methods: We conducted a cross sectional and analytical study over ten years at the Douala General Hospital (DGH), Central Africa. Women of childbearing age, sexually active and suffering from infertility, who consulted the DGH during the study period and who were diagnosed with tubal infertility on the basis of HSG and laparoscopy were included in our study. We excluded any woman whose cause of infertility was related to the male partners, as well as those who had not undergone HSG or laparoscopy.
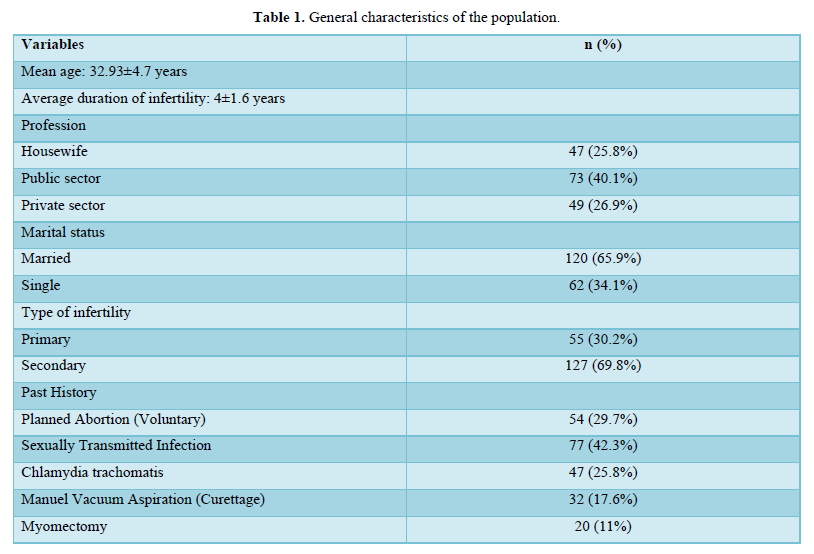
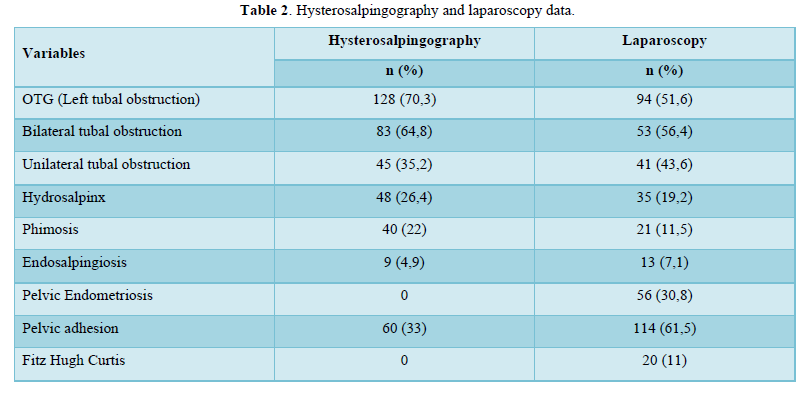
Results: We recruited 182 patients: the mean age was 32.9±4.7 years; married women were the most represented (65.9%); women working in the public sector represented 40.1%; secondary infertility was the most common type of infertility in 69.8% of cases; the mean duration of infertility was 4 years; the sensitivity (Se), specificity (Sp), Positive Predictive Value (PPV), Negative Predictive Value (NPV) of hysterosalpingography and kappa coefficient were respectively: (Se 66.04%, Sp 61.24%, PPV 48.8%, NPV 84.44, Kappa 0.23) in bilateral tubal obstruction; (Se 41.46%, Sp 81.56%, PPV 39.53%, NPV 82.73%) in unilateral tubal obstruction; (Se 35.71%, Sp 71; 43%, PPV 66.7%, NPV 41.0%, Kappa 0.063) in pelvic adhesions; (Se 46.15%, Sp 98.21%, PPV 66.7%, NPV 95.9%, Kappa 0.517) in endosalpingiosis. Laparoscopy also allowed the diagnosis of 11% of pelvic adhesions (Fitz Hugh Curtis syndrome) and endometriosis lesions that could not be identified by hysterosalpingography. It also helped to define a therapeutic strategy in each case.
Conclusion: Although these two examinations are complementary essentially in the evaluation of the tube, laparoscopy should be associated whenever possible.
Keywords: Tubal infertility, Hysterosalpingography, Laparoscopy, Sub-Saharan Africa
METHODS
We conducted a cross-sectional analytical study over a period of 10 years with retrospective data collected from 1 January 2008 to 31 December 2017 and prospective data from 3 February to 30 May 2018. This study took place in the Gynecology and Obstetrics Department of the Douala General Hospital (DGH). All patients or records of patients suffering from infertility who consulted the DGH during the study period and in whom the diagnosis of tubal infertility had been made on the basis of laparoscopy and HSG were included. All patients had undergone HSG followed by laparoscopy.
Administrative authorization to conduct the study was obtained from the DGH and informed consent was obtained from each patient at the time of prospective collection. Interpretation of HSG images was done in a collegial manner in the radiology department to minimize inter-observer bias. The data collected at HSG were documented: normal tubal patency, bilateral or unilateral proximal or distal tubal obstruction, tubal phimosis, hydrosalpinx, endosalpingiosis lesions, pelvic adhesions and uterine anomalies. The patients then underwent diagnostic and possibly therapeutic laparoscopy in the operating theatre of the DGH after a conclusive pre-operative work-up. All the pathologies were noted during laparoscopy and hysterosalpingography; tubal patency was assessed on laparoscopy by methylene blue test.
Data were recorded and analyzed with SPSS version 20.0 software; illustrations of the results were designed using Microsoft Office Excel 2016 software; HSG results were compared with laparoscopy results. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of HSG were determined considering laparoscopy as the 'gold standard'; the Kappa statistical test was used to determine the degree of agreement between the results of hysterosalpingography and laparoscopy.
RESULTS
A total of 182 patients were recruited. All were suffering from infertility and had undergone HSG and laparoscopy for the etiological investigation of infertility. The characteristics of the population are shown in Table 1. The average age of the population was 32.9±4.7 years; women working in the public sector were the most represented (40.1%) as well as married women (65.9%); secondary infertility was the most common (69.8%); the average duration of infertility was 4 ±1.6 years. 70.3% of the patients had a tubal obstruction at HSG compared to 51.6% at laparoscopy. Table 2 compares the results of HSG with those of laparoscopy: HSG had moderate sensitivity (66.04%), moderate specificity (61.24%), low PPV (41.8%), good NPV (84.44%) in the diagnosis of bilateral tubal obstruction which means that 66% of the patients with bilateral tubal obstruction could be diagnosed on hysterosalpingography and 61% of the patients with bilateral tubal patency could be diagnosed on HSG; when HSG revealed bilateral tubal obstruction there was a 42% chance that both tubes were truly occluded and when HSG revealed bilateral tubal patency there was an 84% chance that both tubes were truly patent cy (41,46%); HSG had a high specificity (81.56%), a low PPV (39.53%), a good NPV (82.73%) in the diagnosis of unilateral tubal obstruction which means that only 41% of the patients with unilateral obstruction could be diagnosed by HSG, and 82% of the patients with unilateral tubal patency could be diagnosed by HSG; when the HSG revealed unilateral tubal obstruction, there was a 39% chance that the tube was truly occluded and when it revealed tubal patency there was an 83% chance that the tube was patulous. In the diagnosis of pelvic adhesions, HSG had a low sensitivity (35.7%), moderate specificity (71.43%), moderate PPV (66.7%) and a low NPV (41%). In the diagnosis of endosalpingiosis HSG had low sensitivity (46.15%), high specificity (98.21%), moderate PPV (66.7%) and good NPV (95.9%) (Table 3).
The concordance (matching) between HSG and laparoscopy was very poor for pelvic adhesions, it was also poor in the diagnosis of bilateral tubal obstruction and unilateral tubal obstruction and at least moderate for endosalpingiosis.
DISCUSSION
Exploration of tubal function is an important step in the investigation of an infertile woman. HSG is the most commonly used method and allows assessment of tubal patency and uterine anatomy. Laparoscopy is the gold standard in infertility and provides a comprehensive view of the female pelvis and abdominal cavity, it is both a diagnostic and therapeutic method. Its important role in the diagnosis and management of tubal infertility is well established.
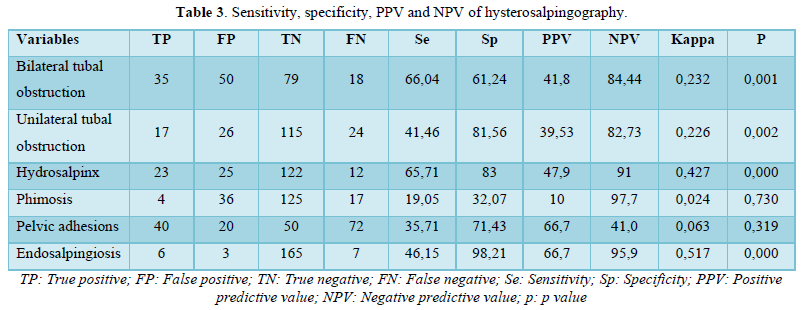
HSG had moderate sensitivity, moderate specificity, low PPV and good NPV for the diagnosis of bilateral tubal obstruction; low sensitivity, high specificity, low PPV and good NPV for the diagnosis of unilateral tubal obstruction. These results differ from the literature [13,14]; the false positives observed could be explained firstly by the tubal spasm caused by pain when HSG was performed without analgesia, secondly when the contrast medium was weakly injected, protein debris and/or mucus could also obstruct the tube [15], and thirdly when the cervical cannula was poorly placed, this could lead to reflux of the contrast medium into the vagina and make it appear to be a tubal obstruction [15]. The presence of pelvic adhesions could also lead to a false positive. False negatives could be explained by a long period between the HSG and laparoscopy, laparoscopy would therefore reveal lesions that were not present when the HSG was performed.
In this study, HSG had a low sensitivity (46.15%), high specificity (98.21%), moderate PPV (66.7%) and good NPV (95.9%) in the diagnosis of endosalpingiosis. We found 4.9% of cases of endosalpingiosis on HSG versus 7.1% on laparoscopy. This differs from the literature which found no endosalpingiosis on HSG and laparoscopy [13,16-17]. HSG is the only imaging test to determine the existence of proximal tubal involvement in endometriosis (mistletoe ball diverticular image or proximal tubal obstruction) and laparoscopy is the gold standard for accurate diagnosis of endosalpingiosis. Endosalpingiosis can cause tubal infertility by obstructing the tube but also by promoting the secretion of biological factors that can lead to infertility [18]. In the diagnosis of pelvic adhesions, HSG had a low sensitivity (35.7%), moderate specificity (71.43%), moderate PPV (66.7%) and low NPV (41%); 29.7% of patients had pelvic adhesions at HSG compared to 48.4% at laparoscopy, the false negatives observed here can be explained by the presence of fine endoluminal adhesions not identified at HSG but which may compromise fertility [19-21]. Laparoscopy allowed the diagnosis of 30.8% of cases of pelvic endometriosis compared to zero at HSG, these cases not identified at HSG could be the cause of infertility most often labelled as unexplained [22-24]. In this study, the tubal mucosa could not be assessed due to the absence of data. Neither HSG nor laparoscopy reports were specific about the condition of the tubal mucosa.
CONCLUSION
The study revealed limitations of HSG in the diagnosis of endosalpingiosis, pelvic endometriosis and pelvic adhesions; t has a good negative predictive value in the diagnosis of bilateral or unilateral tubal obstruction. We believe that although these two examinations are complementary, essentially in the evaluation of the tube, for which the assessment of the mucosa by HSG is the examination of choice, laparoscopy should be associated whenever possible.
- Meheus A, Reniers J, Colletet M (1986) Determinants of infertility in Africa. Afr J Sex Transmi Dis 2(2):31-5.
- Audebert AJM, Laru CS, Emperaire JC (1980) Coelioscopie et infertilité: évolution des indications à propos d'une série de 1055 cas. Revue Française de Gynécologie et d'Obstétrique 75(8-9): 427-435.
- Gironnet I, Monier V, Bron G (1987) Les obstructions tubaires fonctionnelles. Revue Française de Gynecologie et d'Obstetrique 82(6-7): 415-417.
- Pambou (1984) Facteurs étiologiques de la stérilité conjugale au Congo. Thèse de Médécine. Brazza.
- Tembely F (2008) Stérilité du couple dans le centre de santé de référence de la commune v de Bamako à propos de 145 cas. Thèse de Médecine. Université de Bamako.Bamako.
- Choupe TLB (2007) Place de la coeliochirurgie ans le diagnostic et la prise en charge des stérilités féminines. Thèse de Médecine. Université de Bamako. Bamako.
- Traore H (2007) Relation entre les résultats de l'hystérosalpingographie et de la coelioscopie dans le bilan de l'infécondité féminine à propos de 200 cas. Thèse de Med. Université de Bamako. Bamako.
- Traore Y (2008) Prise en charge de la stérilité féminine secondaire dans le service de gyn-obs du centre de santé de référence de la commune du district de Bamako. Université de Bamako. Thèse de médecine. Bamako.
- Wright KL (2004) Définir infertilité. FHI (network en français) 23: 4-12.
- Takpara I, de Souza J, Azilinon DL, Perrin RX, Alihonou E (1998) Assistance médicale à la procréation (AMP) à la clinique universitaire de gynécologie et d'obstétriqque du CNHU de Cotonou: Indication et étude de faisabilité. Le Benin Médical 8: 36-39.
- Balasch J (2000) Investigation of the infertile couple in the area of assisted reproductive technology: A time for reappraisal. Hum Reprod 15(11): 2251-2257.
- Yasbeck C, Le Tohic A, Koskas M, Madelenat P (2010) Pour la pratique systématique d'une coelisocopie dans le bilan d'une infertilité. Gynecol obstet fertile 38(6): 424-427.
- Ngowa KJD, Kasia JM, NGuefack-Tsague G, Nkongo V, Sone C, et al. (2015) Comparison of hysterosalpingograms with laparoscopy in the diagnostic of tubal factor of female infertility at the Yaoundé General Hospital, Cameroon. Pan Afr Med J 22: 264.
- Fatemeh F, Zohreh S (2013) Diagnostic value of Hysterosalpingography and Laparoscopy for tubal patency in infertile women. Nurs Midwifery Stud 2(2): 188-192.
- Risquez F, Confino E (1993) Transcervical tubal cannulation, past, present and future. Fertil Steril 60(2): 21126.
- Tsabu A-C, Ogoudjobi M, Obossou A, King V, Takpara I, et al. (2014) Hysterosalpingography and Laparoscopy in evaluating fallopian tubes in the management of infertility in cotonou, Benin Republics. J West Afr Coll Surg 4(2): 66-75.
- Gandji S, Adisso S, Atrévi N, Dougnon TV, Bankolé HS, et al. (2013) Diagnostic des lésions étiologiques de l’infertilité secondaire à Cotonou: rôle de l’hystérosalpingographie et de l’échographie pelvienne. J Appl Biosci.
- Morcos RN, Gibbons WE, Findley WE (1985) Effect of peritoneal fluid on in vitro cleavage of cell mouse embryos: Possible role in infertility associated with endometriosis. Fertil Steril 44(5): 678-683.
- Abbara A. Lexique de la Médecine de la reproduction.
- Al-Badawi IA, Fluker MR, Bebbington MW (1999) Diagnostic laparoscopy in infertile women with normal hysterosalpingography. J Reprod Med 44(11): 953-957.
- Waheed S, Mazhar R, Klan NH, Rafi M (2007) The comparison of hysterosalpingography and laparoscopy in predicting fertility. Ann King. Edward Med Uni 13(3): 202-205.
- Njamen NT, Nkwabong E, Nguefack TC, Padjip NG, Nana NC, et al. (2017) Epidemiology and hysterosalpingogram findings in tubal infertility: results of a case series in sub-saharan Africa’s setting. J Afr Imag Méd 9(4): 180-186.
- Pritts EA, Taylor RN (2003) An evidence-based evaluation of endometriosis-associated infertility. Endocrinol Metab Clin North Am 32: 653-667.
- Oral E, Arici A, Olive DL, Huszar G (1996) Peritoneal fluid from women with moderate or severe endometriosis inhibits sperm mobility: The role of seminal fluid components. Fertil Steril 66(5): 787-792.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Chemotherapy Research Journal (ISSN:2642-0236)
- Advance Research on Alzheimers and Parkinsons Disease
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)
- Journal of Pathology and Toxicology Research

