Research Article
Clinical Presentation, Comorbidities and Outcomes among COVID-19 Patients Admitted at The Isolation and Treatment Centre, Amachara, Abia State, Nigeria.
3121
Views & Citations2121
Likes & Shares
Introduction: Corona virus; the organism causing COVID-19 was discovered in Wuhan China in 2019. It was declared a pandemic by the World Health Organization on March 11, 2020. The spread, severity and mortality cut across countries of the world. Nigeria reported cases of COVID-19 in varying degrees with recorded mortalities. All 36 states in Nigeria have cases and deaths though the overall deaths in the country is low. The objectives of this study were to describe the patterns of clinical presentation, co-morbidities and outcomes of COVID-19 among patients that presented at the isolation and treatment center, Amachara- Abia state, Nigeria.
Materials and Methods: This was a descriptive cross-sectional study using existing data of 337 patients admitted at the isolation and treatment center, Amachara in Abia state, Nigeria between May to December, 2020. Data was collected on age, sex, occupation, clinical signs and symptoms, co-morbidities and outcomes. Data was analyzed using SPSS version 23.0 and presented in tables.
Results: Ninety-six (28.5%) patients were 21-30 years of age, 10 (3.0%) were between 1-10 years while 5 (1.5%) were more than 80 years of age. Two hundred and ten patients (62.3%) were males while 127 (37.7%) were females. One hundred and fifty-seven patients (46.6%) lived in the rural areas of the state. Out of the 337 patients, 150 (44.5%) presented with symptoms while 187 (55.5%) were asymptomatic. Clinical presentations of patients included; weakness (100%), loss of taste and smell, 20 (5.9%), fever 125 (37.1%), catarrh 48 (14.2%), cough 114 (33.8%), difficulty in breathing 66 (19.6%), headache 37 (11.0%). Patients with co-morbidities were 28 (8.3%) for hypertension and 7 (2.1%) diabetics. There were 3 (0.9%) deaths of whom all had hypertension and diabetes.
Conclusion: COVID-19 affected all age groups from this study. Symptoms of COVID-19 are non-specific presenting like malaise and respiratory infections. Two out of the three deaths were above 50 years, lived in rural areas.
Keywords: COVID-19, Clinical presentation, Co-morbidities, Outcomes, Isolation center, Abia state
INTRODUCTION
COVID-19 infection caused by the virus- severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first discovered in Wuhan China in December 2019 [1]. The virus spread across regions and countries of the world [2] and within three months of discovery it spread to 113 countries (WHO, 2020). It was declared a pandemic by the World Health Organization on March 11, 2020. Globally, as of 2021, the virus had spread to 216 countries with 221,648,869 confirmed cases and 4,582,338 confirmed deaths [3]. The first confirmed case of coronavirus disease in Nigeria as declared by the Nigeria Centre for Disease Control (NCDC) was on 27 February 2020 [4]. Rapid urbanization and increase in international travel were attributed to be one of the causes of wide spread of SARS-CoV-2 globally [5]. International travels into Nigeria were banned during the country’s lock down to reduce travelers into the Nigeria. This was eased after five weeks and restrictions put in place to check flow of international travels. Symptoms of COVID-19 are not specific, presenting like symptoms of malaria and respiratory infections. SARS-CoV-2 is similar to severe acute respiratory syndrome virus (SARS-CoV) by 80%, the Middle East respiratory syndrome virus (MERS-CoV) by 50% and 96% similar to bat coronavirus (RaTG13) [6]. Transmission is airborne from person to person. Spread of the virus was thought to be from only symptomatic carriers but asymptomatic carriers have shown possibility of transmission [7,8]. Time of spread from one person to another cannot be determined as the virus is known to be contained in droplets from nose and mouth even when a person is asymptomatic [9,10]. Severe symptoms are more with underlying comorbidities as hypertension, cardiovascular disease and diabetes mellitus [2,11]. The effect of the virus is seen in all systems of the body; the central nervous system, the circulatory system resulting in septic shock in some patients and the respiratory system most especially [12]. COVID-19 outcome is dependent on the severity of infection. Definitive diagnosis of COVID-19 by molecular method using RT-PCR is the most specific and sensitive. Other laboratory techniques such as protein testing, rapid antigen test, cell culture and computed tomography also exist for diagnosis of COVID-19 [13,14]. The control of COVID-19 has been challenging to the global health system, individuals and the global economy. Health systems of countries have been crippled resulting in overwhelming burden to human, material and financial resources [15]. Strategies instituted by countries in the control of spread of COVID-19 such as lockdowns disrupted social, education and economic activities. This affected individuals and families [16] as well as placing huge economic costs on government and institutions [17]. Preventive measures in the spread of COVID-19 as recommended by the World Health Organization (WHO) [3] are intended to limit spread of the virus. Compliance to non-pharmacological preventive measures such as limiting physical contact, maintaining a 1-2-meter distance, handwashing, wearing of facemasks depend on behavioral and cultural conditions [18]. Nigeria’s health system was not spared by the pandemic. The Federal Government constituted a Presidential Task Force on COVID 19 (PTF) which coordinated responses both at national and regional levels. There were regular updates through the Nigeria Centre for Disease Control (NCDC) on cases, deaths and rising issues including efforts made in sourcing for vaccines. As of September 5th, 2021 a total of 5,001,836 vaccine doses have been administered in Nigeria [19]. As part of efforts to suppress the spread of the virus, all suspected cases were tested, confirmed cases isolated in various isolation centers across the country and tracing contacts of confirmed cases. Each state established an Emergency Operations Centre from where activities were coordinated and reports submitted to the Federal Ministry of Health and the NCDC. Contrary to predictions, there has been low morbidity and mortality of COVID-19 compared to other regions of the world [19]. Factors associated with this low data have been posited to several hypotheses such as demographic age structure of sub-Saharan Africa, lack of long-term care facilities, prior exposure to Coronavirus infection, limited access to adequate testing, genetic risk factors and effective government public health response [20]. Studies conducted on clinical presentations of COVID-19 have been from other states in Nigeria with scarce reports from Abia state. This study therefore adds to the body of literature on clinical presentations, comorbidities and outcomes of COVID-19 patients as documented in Abia state.
MATERIALS AND METHODS
Study site
This study was conducted at the COVID-19 isolation and treatment center, Amachara, Umuahia- Abia state, Nigeria. Abia state has three isolation centers established during the pandemic. These are located in the two major cities of Abia state- Aba and Umuahia. Umuahia is Abia state’s capital. Abia is a state in the south eastern part of Nigeria. It is located along the rail road that lies between Port Harcourt to its south and Enugu to its north. Umuahia has a population of 359,230 according to 2006 census [21]. The language in Umuahia is predominantly Igbo. Residents of Umuahia are a mix of civil servants, traders, businesses and farmers. Umuahia has two major seasons in the year- raining and dry season. The raining season ushers in agricultural activities and at this time, there is usually increase in waste generation from various activities. The treatment and isolation center Amachara are managed by a team of medical and non-medical personnel. The non-medical are technicians who managed the machines and equipment in the center. Patients’ admittance was strictly in compliance with the guidelines of the NCDC. Diagnosis and treatment were in accordance to international guidelines as published by the World Health Organization.
Study design
This was a descriptive cross-sectional study using retrospective data from the facility.
Study population
A total of three hundred and thirty-seven (337) case folders of patients admitted at the isolation and treatment center, Amachara between May and December, 2020 were retrieved and used for data collection.
Inclusion criteria
All cases tested and confirmed positive by the facility laboratory.
Method of data collection
Three research assistants were trained for data collection bearing in mind objectives of the study and parameters of interest. Variables of interest were socio-demographics; age, sex, residence, marital status, occupation. Other variables of interest included; comorbidities, presenting complaints, drug regimen and treatment outcomes.
Data Analysis
Data was analyzed using SPSS version 23.0 software and presented in tables.
Ethical Clearance
Ethical clearance was obtained from the research and ethics committee of Abia state University Teaching Hospital and the Department of Community Medicine, Abia state University Teaching Hospital.
RESULTS
Table 1 shows the socio-demographic characteristics of patients. Majority of patients; 96 (28.5%) were between 21-30 years, 10 (3.0%) were 1-10 years of age while the least age group were those above 80 years; 5(1.5%). Two hundred and ten patients (62.3%) were males. Out of the 337 patients, 180 (53.4%) lived in the urban area while 157 (46.6%) lived in the rural area. Majority of the patients, 204 (60.5%) were married.
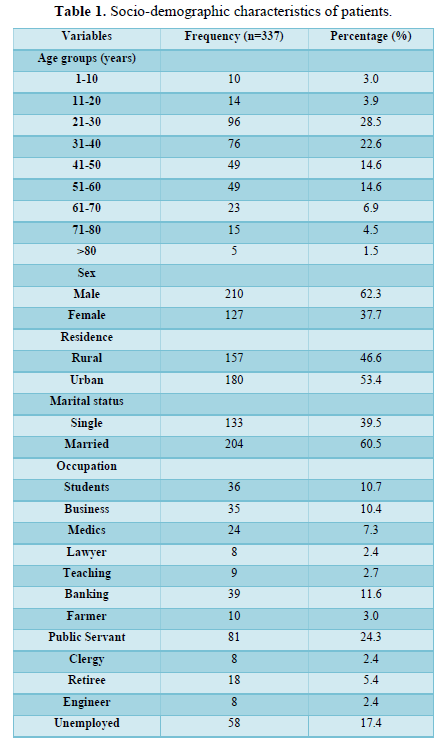
Table 2 shows the presenting signs and symptom of patients. One hundred and fifty patients (44.5%) had symptoms while 187 (55.5%) did not have symptoms. All patients presented with weakness at the point of admission, 125 (37.1%) patients had fever while 20 (5.9%) patients had loss of taste and smell. Difficulty in breathing was recorded in 66 (19.6%) patients.
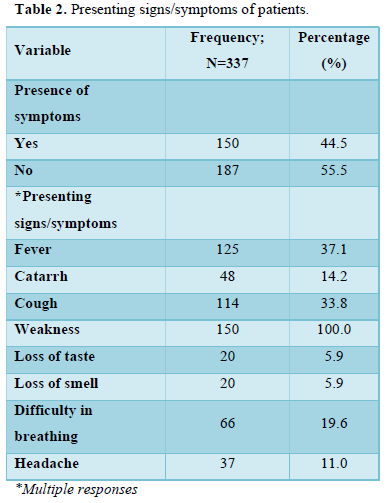
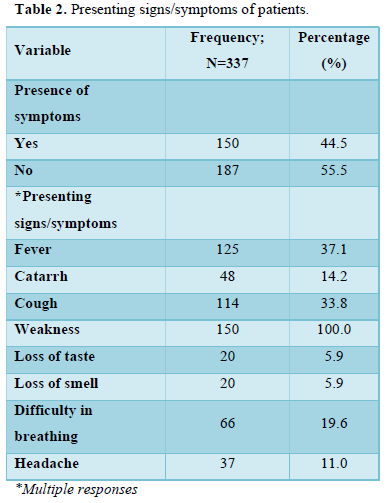
Table 3 shows the associated co-morbidities of the patients. Twenty-eight (8.3%) patients were hypertensive, 7 (2.1%) had Diabetes mellitus, 15 (4.5%) had peptic ulcer.
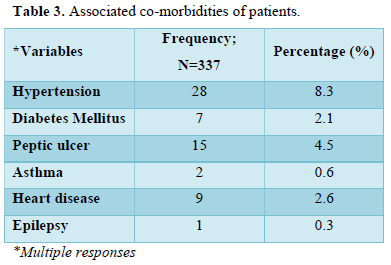
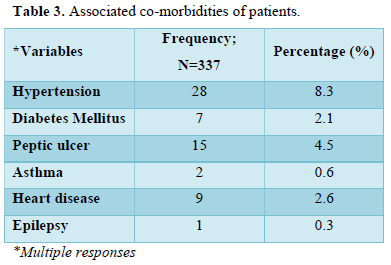
Table 4 shows oxygen saturation of the patients. More than half of the patients, 196 (58.2%) had 96-100% of oxygen saturation. Forty-seven (13.9%) patients presented with 66-70% oxygen saturation capacity.
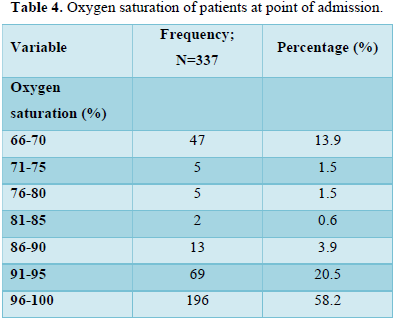
Table 5 shows treatment outcomes of the patients. Only 3 (0.9%) died while 334 (99.1%) recovered.
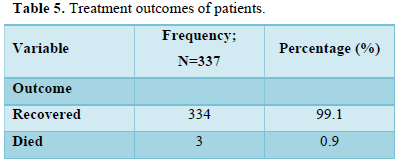
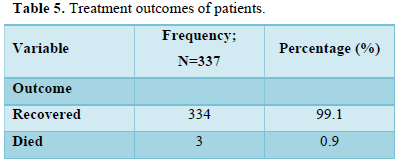
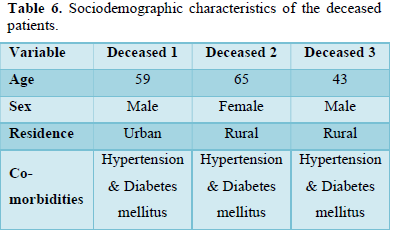
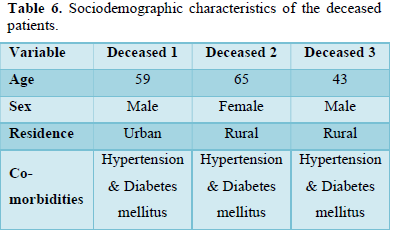
Table 6 shows socio-demographic characteristics of the deceased patients. There were two (2) males and one (1) female. They were all hypertensive and diabetic.
DISCUSSION
This study reviewed the clinical presentation of COVID-19 among patients in Abia state. Clinical presentations of COVID-19 range from asymptomatic to varying degrees of mild, moderate and severe symptoms resulting in death of some patients [22,23]. Symptoms may develop within 2-14 days of exposure to the virus. Symptoms such as fever, cough, sore throat, weakness, breathlessness are suggestive of COVID-19 infection [24]. In this study, slightly above half of the patients, 187 (55.7%) did not have symptoms on presentation to the isolation and treatment center. They were contacts of symptomatic patients. This result was different from a study conducted in Federal Medical Centre Asaba where 24% of patients didn’t have symptoms [25]. This could be attributed to the number of patients in the study and the fact that Amachara isolation center where this study was carried out received patients from all over Abia state. Also, the isolation center conducted its own laboratory tests attracting people from outside Abia state to access the facility. Symptoms of patients in this study were fever, cough, headache, breathlessness, weakness, loss of taste and smell. The commonest complaint was weakness while only 5% complained of loss of taste and smell at some point in the course of the illness. These symptoms are similar complaints reported in previous studies as indicative of COVID-19 [24, 26-28]. Spread of COVID-19 is not dependent on age as seen in this study. From this study, all age groups; children, middle aged and the elderly were infected with the virus. This was similar to other studies reported elsewhere [25,29]. This study result showed a higher concentration of infection between ages 21-30 years. This finding could be attributed to the fact that this age group being youths are students or workers who travel from one place to the other. It can also be argued that they are less likely to adhere to preventive measures against COVID-19. In contrast, a study conducted in China [30] reported a higher age exposed to the virus. Severity and mortality of COVID-19 infection have previously been documented to be higher with increased age, in males than females and in patients with medical conditions such as hypertension and diabetes mellitus [31]. This study finding showed three deaths (0.9%) out of 337 patients. Out of these, two were males and a female. They all were both hypertensive and diabetic. Another finding from this study similar to other studies is increasing age documented to be significantly associated with higher mortality [32,33]. In this study, 53.4% of patients reside in the urban area as against 46.6% residing in the rural communities. This is expected with the high density of activities in the urban cities resulting in movement in and out of the city. Movement of people makes it possible for rapid spread of infection. Association of population density with spread of COVID-19 was demonstrated by Bhadra A et al in their study [34]. They discovered a moderate association between increase infection and mortality of COVID-19 with population density. In contrast to Bhadra A et al, two out of the three patients that died lived in rural areas. This finding could be attributed to delay in arriving at the isolation centre located in the city. This study also showed the deceased were all hypertensive and diabetic as reported in earlier studies [31-34]. Patients with both hypertension and diabetes mellitus have higher mortality rate than those with one or no underlying health condition [33]. Morgan et al in their study revealed poor diabetic control in patients with COVID-19 resulting in reduced immunity and hence death in those patients [35]. As against high mortality predictions in Sub-Saharan Africa, Nigeria has recorded 3124 deaths as of January 2022 since the start of the pandemic [36]. In Abia state, Nigeria, this isolation centre has the lowest mortality of patients. This finding could be attributed to government commitment to reducing effects of the virus in the state. The staff of the centre were also fully committed to ensuring patients received the best care during their stay at the centre. The government placed in check modalities for contact tracing with continuous public sensitization on early presentation to the isolation and treatment centre as a way to quick recovery. From observation, patients who presented early to the isolation centre recovered faster than late presenters.
STUDY LIMITATIONS
Data used was hospital-based which might not be a total representation of COVID-19 in Abia state considering patients who did not get to hospital and those not tested.
CONCLUSION
This study showed clinical presentation and distribution of COVID-19 in Abia. Results revealed, all age groups were affected by the virus. Recovery from the infection was observed to depend on early presentation to the isolation and treatment centre. Two of three patients that died were above 50 years, lived in rural areas while all three had co-morbidities.
- Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global concern. Lancet 395: 470-473.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 395: 507-513.
- World Health Organization (WHO) (2021) Coronavirus disease (COVID-19) pandemic Emergencies. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Nigeria Centre for Disease Control (2020) First case of coronavirus disease confirmed in Nigeria. Available online at: http://www.ncdc.gov.ng
- Wilder SA, Chiew CJ, Lee VJ (2020) Can we contain the COVID-19 outbreak with the same measures as for SARS. Lancet Infect Dis 20(5): e102-e107.
- Zhou P, Yang XL, Wang XG (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579: 270-273.
- Lechien JR, Chiesa-Estomba CM, De-Siati DR, Horoi M, Le-Bon SD, et al. (2020) Olfactory and gustatory dysfunctions as a clinical presentation of mild-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur Arch Otorhinolaryngol 6: 1-11.
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR (2020) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019, (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 55(3): 105924.
- Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104: 246-251.
- Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, et al. (2020) Transmission of 2019-nCoV infection from asymptomatic contact in Germany. N Engl J Med 382: 970-971.
- Fei Z, Ting Y, Ronghui D, Ghouhui F, Ying L, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395 (10229): 1054-1062.
- Wan S, Xiang Y, Fang W, Zheng Y, Li B, et al. (2020) Clinical features and treatment of COVID 19 patients in northeast Chongqing. J Medi Viro 92(7): 797-806.
- Loeffelholz MJ, Tang YW (2020) Laboratory diagnosis of emerging human coronavirus infections-the state of the art. Emerg Microbes Infect 9: 747-756.
- Carter LJ, Garner LV, Smoot JW, Li Y, Zhou Q, et al. (2020) Assay techniques and test development for COVID-19 diagnosis. ACS Cent Sci 6: 591-605.
- Maia ChA, Molloy JC, Prieto-Godino LL, Baden T (2020) Leveraging open hardware to alleviate the burden of COVID-19 on global health systems. PLoS Biol 18(4): e3000730.
- Ornell F, Schuch JB, Sordi AO, Kessler FH (2020) ‘Pandemic fear’ and COVID-19; Mental health burden and strategies. Braz J Psychiatry 42(3): 232-235.
- Amponash R, Frimpong IA (2020) Ghana in the face of COVID-19: Economic impact of Coronavirus (2019-NCOV) outbreak on Ghana. J Busi Manag 8(4): 1404.
- Coroiu A, Moran C, Campbell T, Geller AC (2020) Barriers and facilitators of adherence to social distancing recommendations during COVID-A9 among a large international sample of adults. PLoS One: e0239795.
- World Health Organization (WHO) (2020). Coronavirus (COVID019) Dashboard. Available online at http://covid19.who.int/
- Adams J, Mary J, Mac K, Adeladza KA, Alex E, et al. (2021) The Conundrum of low COVID-19 mortality burden in sub-Saharan Africa: Myth or reality? Global Health: Science and Practice. Available online at: https://doi.org/10.9745/GHSP-D-21-00172
- National Population Commission of Nigeria (NPC) (2006) City Population. Available online at: https://www.citypopulation.de/php/nigeria-adm1id=NGA010
- Symptoms of Coronavirus. CDC (2022) Available online at: www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, et al. (2020) The Incubation period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann Intern Med 172(9): 577-582.
- Hui DS, Azhar I, Madani TA, Ntoumi F, Kock R, et al. (2020) The continuing 2019 -nCoV epidemic threat of novel coronaviruses to global health- The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 91: 264-266.
- Aigbokhade AQ, Orhue NL, Ofili AN, Oseji M, Osiatuma VA, et al. (2021) Patterns of Clinical Presentation of COVID-19 Patients in Federal Medical Centre, Asaba, Nigeria. J Community Med Prim Health Care 33(1): 1-13.
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the Coronavirus disease 2019 outbreak in China: Summary of a report of 72314 cases from the Chinese centre for Disease control and prevention. JAMA 323(13): 1239-1242.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC (2020) Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 324(8): 782-793.
- Burke RM, Killerby ME, Newton S, Ashworth CE, Berns AL, et al. (2020) Symptom Profiles of a Convenience Sample of Patients with COVID-19- United States, January-April 2020. MMWR Morb Mortal Wkly Rep 69(28): 904-908.
- Mohan A, Tiwari P, Bhatnagar S, Patel A, Maurya A, et al. (2020) Clinico-demographic profile and hospital outcomes of COVID-19 patients admitted at a tertiary care centre in north India. J Med Res 152: 61.
- Nanshan C, Zhou M, Xuan D, Jieming Q, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 395: 507-513.
- Williamson EJ, Walker AJ, Bhaskaran K, et al. (2020) Open SAFELY: Factors associated with COVID-19 death in 17 million patients. Nature 584(7821): 430-436.
- Bhandari S, Singh A, Sharma R, Rankawat G, Banerjee S, et al. (2020) Characteristics, Treatment outcomes and role of hydroxychloroquine among 522 COVID-19 hospitalized patients in Jaipur City: An epidemio-clinical study. J Assoc Physicians India 68: 13-19.
- Rivera-Izquierdo M, del Carmen Valero-Ubierna M, R-delAmo JL, Fernandez-Garcia MA, Martinez-Diz S, et al. (2020) Sociodemographic, clinical and laboratory factors on admission associated with COVID-19 mortality in hospitalized patients: A retrospective observational study. PLoS One 15: e0235107.
- Bhadra A, Mukherjee A, Sarkar K (2020) Impact of population density on COVID-19 infection and mortality rate in India. Model Earth Syst Environ 14: 1-7.
- Gold MS, Sehayek D, Gabrielle S, Zhang X, McCusker C, et al. (2020) COVID-19 and co-morbidities: A systematic review and meta-analysis. Postgraduate Medicine 132(8): 749-755.
- Nigeria Centre for Disease Control (2022) COVID-19 Nigeria. Available online at: http://www.ncdc.gov.ng
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)







