2382
Views & Citations1382
Likes & Shares
Aim: To identify the prevalent organism in cellulitis and offer antibiotics as per antibiotic sensitivity pattern.
METHODOLOGY
Type of study: Observational study.
Study Population: Cases diagnosed clinically as cellulitis.
Definition: Cellulitis was defined as an acute, spreading inflammation of the skin and subcutaneous tissues, characterized by three or more of the following clinical findings: tenderness, erythema, swelling or increased warmth.
Inclusion criteria: All patient 16 year or older admitted in surgical wards were included in the study.
Exclusion criteria: Patients with evidence of inflammation due to intravenous catheter or phlebitis, edema, diabetes, vascular disease and patients who received prior antibiotic therapy were excluded from the study.
Needle aspiration was done with a 2ml syringe and a 22G needle. The needle was removed and the syringe brought to the microbiological laboratory and analyzed according to standard procedures.
The organism isolated was tested for sensitivity and resistance to Amikacin, Gentamycin, Linezolid, Ciprofloxacin.
RESULTS
Out of 48 patients, Staph aureus was grown in 20 patients (41.66%), MSSA was grown in 10 patients (20.83%), no growth occurred in 14 patients (29.16%), E Coli in 2 patients (4.16%), MRSA in 1 patient (2.08%) and likely to be skin contaminated in 1 patient (2.08%) (Table 1).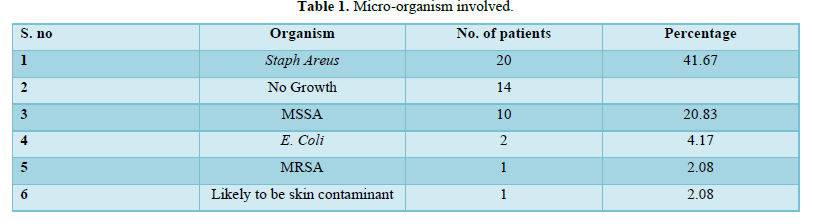
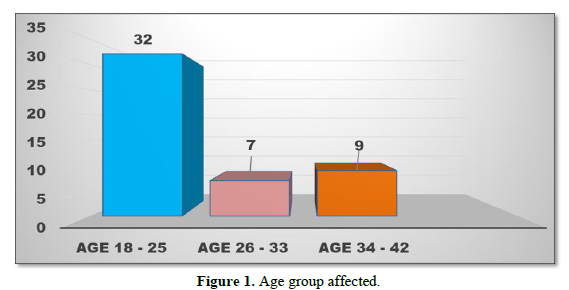
The most common age group affected was 18-25 years in which 32 patients (66.66%) had cellulitis. The age bracket between 26-33 years involved 7 patients (14.58%) whereas 9 patients (18.75%) were affected in the age group between 34-42 years (Figure 1).
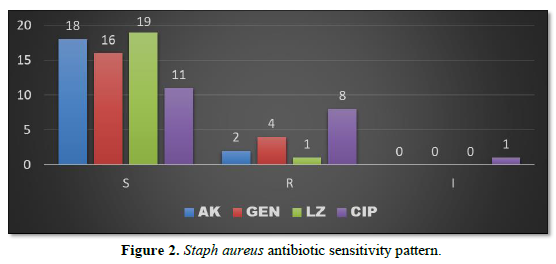
Staph aureus when isolated was sensitive to Linezolid in 19 patients (39.58%), Amikacin in 18 patients (37.50%), Gentamycin in 16 patients (33.33%) and Ciprofloxacin in 11 patients (22.91%). The organism was resistant to Ciprofloxacin in 8 patients (16.66%), resistant to Gentamycin in 4 patients (8.33%), resistant to Amikacin in 2 patients (4.16%) and resistant to Linezolid in 1 patient (2.08%) (Figure 2).
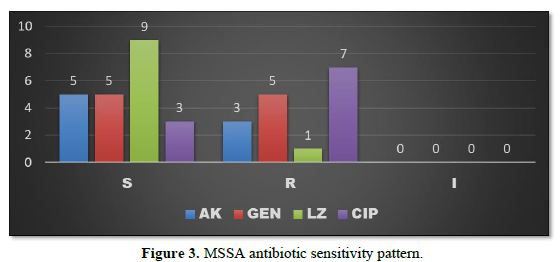
MSSA when isolated was found to be sensitive to Linezolid in 9 patients (18.75%), sensitive to Amikacin and Gentamycin in 5 patients each (10.41%) and to Ciprofloxacin in 3 patients (6.25%). The organism was resistant to Ciprofloxacin in 7 patients (14.58%), resistant to Gentamycin in 5 patients (10.41%), resistant to Amikacin in 3 patients (6.25%) and resistant to Linezolid in 1 patient (2.08%) (Figure 3).
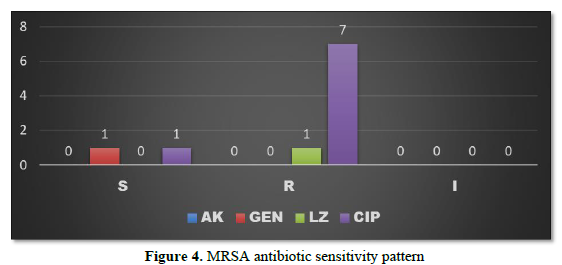
MRSA was found to be sensitive to Gentamycin and Ciprofloxacin in 1 patient each (2.08%) and resistant to Ciprofloxacin in 7 patients (14.58%) whereas resistance to Linezolid was observed in 1 patient (2.08%) (Figure 4).
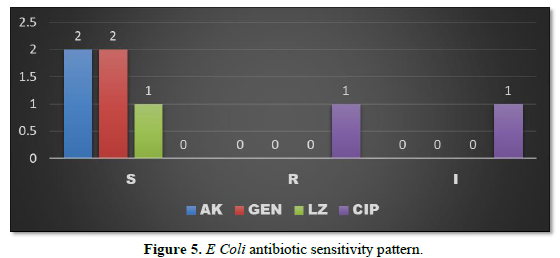
E Coli was sensitive to Amikacin and Gentamycin in 2 patients each (4.16%) and sensitive to Linezolid in 1 patient (2.08%). It was found resistant to Ciprofloxacin in 1 patient (2.08%) (Figure 5).
DISCUSSION
Cellulitis was defined as an acute, spreading inflammation of the skin and subcutaneous tissues, characterized by three or more of the following clinical findings: tenderness, erythema, swelling or increased warmth. Cellulitis may be seen in diabetic foot infections. Erysipelas is defined as cellulitis of the face or extremities with lymphatic involvement. Cellulitis presents with fever and inflammation lasting for 72 h and management includes limb elevation and narrow spectrum antibiotics. Pain out of proportion to the clinical signs accompanied by rapid progression may lead to necrotizing fasciitis [1].
The most common causative organisms are Staphylococcus aureus and Streptococcus [2]. Wound or tissue cultures are negative in up to 70% cases [3]. Our study showed no growth in 29.16% cases. Careful clinical examination may reveal a portal of entry of micro-organisms such as ulcers, trauma, eczema or cutaneous mycosis [4]. Dupuy et al in a study observed that skin breach, lymphedema, venous insufficiency, tinea pedis and obesity are associated with an increased risk of lower limb cellulitis [5].
Diagnosing and treating cellulitis correctly is of immense value as it is often misdiagnosed. A study shows that approximately 30% of cellulitis patients are misdiagnosed as eczema, lymphoedema and lipodermatosclerosis [6]. Under or overtreatment with antimicrobials is often associated while managing lower limb cellulitis and it has been observed that 85% of patients with cellulitis did not require hospital admission and 92% received unnecessary antibiotics [7].
Eron classification of cellulitis is commonly used to grade the severity of cellulitis and is as below [8].
Class I: No signs of systemic toxicity. No uncontrolled co-morbidity (e.g. diabetes mellitus)
Class II: Systemically unwell or systemically well but with a comorbidity
Class III: Significant systemic upset (e.g. tachycardia, tachypnoea), unstable co-morbidities or limb-threatening infection due to vascular compromise.
Class IV: Sepsis or severe life-threatening infection (e.g. development of necrotizing fasciitis)
Marwick et al used a modified version of the Eron classification (the Dundee classification) to separate patients into distinct groups based on the presence or absence of defined systemic features of sepsis.
Dundee class I and class II patients are treated with oral antibiotics and Dundee class III and class IV usually require injectable antibiotics. Early surgical consultation and wound debridement is required in patients with deep or necrotizing infection [9].
Antibiotics
As Staph aureus and Streptococcus are the most commonly involved causative organisms, UK CREST guidelines recommend that an antibiotic with both anti-streptococcal and anti-staphylococcal activity, such as Flucloxacillin be used [10]. A study by Stevens et al suggests that Clindamycin or Linezolid should be used in patients with severe or necrotizing infections [11]. Eron [3] recommends that most patients with uncomplicated cellulitis can be safely switched to oral antibiotics after 1-4 days of parenteral therapy [3]. CREST guidelines to recommend switching over to oral antibiotics on observing settling pyrexia, stable comorbidities, less intense erythema and falling inflammatory markers [10].
Duration of Antibiotics use
Most cases of uncomplicated cellulitis are treated with 1-2 weeks of antibiotics [3]. A study by Hepburn [12] has found that 5 days antibiotic course may be sufficient in cases of uncomplicated cellulitis [12].
CONCLUSION
The most common causative organism causing cellulitis is Staph aureus. The most common age group affected is 18-25 years. Staph aureus was found to be most sensitive to Linezolid, Amikacin and Gentamycin and was found most resistant to Ciprofloxacin. Cellulitis should be diagnosed correctly and differentiated well from eczema, lymphedema and lipodermatosclerosis. Most cases of cellulitis can be managed conservatively with oral antibiotics on outpatient basis and respond well in 5 to 7 days of antibiotic therapy. Ciprofloxacin, Linezolid, Amikacin and Gentamycin are the commonly used antibiotics for treatment of cellulitis.
- Borschitz T, Schlicht S, Siegel E, Hanke E, von Stebut E (2015) Improvement of a clinical score for necrotizing fasciitis: ‘Pain out of proportion’ and high CRP levels aid the diagnosis. PLoS One 10: e0132775.
- Bennett JE, Dolin R, Blaser MJ, Mandell GL (2010) Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 7th Philadelphia: Churchill Livingstone/Elsevier.
- Eron LJ, Lipsky BA (2006) Use of cultures in cellulitis: when, how, and why? Eur J Clin Microbiol Infect Dis 25: 615-617.
- Eriksson B, Jorup-Rönström C, Karkkonen K, Sjöblom AC, Holm SE (1996) Erysipelas: Clinical and bacteriologic spectrum and serological aspects. Clin Infect Dis 23: 1091-1098.
- Dupuy A, Benchikhi H, Roujeau JC, Bernard P, Vaillant L, et al. (1999) Risk factors for erysipelas of the leg (cellulitis): Case-control study. BMJ 318: 1591-1594.
- Weng QY, Raff AB, Cohen JM, Gunasekera N, Okhovat J-P, et al. (2017) Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol 153: 141-146.
- Levell NJ, Wingfield CG, Garioch JJ (2011) Severe lower limb cellulitis is best diagnosed by dermatologists and managed with shared care between primary and secondary care. Br J Dermatol 164: 1326-1328.
- Eron LJ, Lipsky BA, Low DE, Nathwani D, Tice AD, et al. (2003) Managing skin and soft tissue infections: Expert panel recommendations on key decision points. J Antimicrob Chemother 52(1): i3-i17.
- Stevens DL, Bisno AL, Chambers HF, Dellinger EP, Goldstein EJC, et al. (2014) Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 59: e10-e52.
- Fulton R, Doherty L, Gill D (2005) Guidelines on the management of cellulitis in adults. Northern Ireland: CREST.
- Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, et al. (2004) Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med 164: 1669-1674.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Allergy Research (ISSN:2642-326X)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Rheumatology Research (ISSN:2641-6999)






