Research Article
The Experience and Results of Cytoreductive Surgery and Hipec Using in Advanced Ovarian Cancer
4626
Views & Citations3626
Likes & Shares
The research object was life quality of patients with ovarian cancer after complex treatment Nowadays cytorective surgery and HIPEC is the mainstay of management of advanced stages ovarian cancer. Study was conducted to assess the effectiveness of combined treatment in IIIA-IIIC ovarian cancer, its impact on quality of life. 37 patients of main group (CRS + HIPEC) were compared with 25 patients of control group (surgery + systemic chemotherapy). The quality of life was assessed with Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). Comparative analysis of quality of life 6 months after treatment completion did not show significant statistical difference. Combination of cytoreduction with HIPEC improves quality of life in patients with ovarian cancer, is tolerated better and has less systemic toxicities than systemic chemotherapy.
Keywords: Ovarian cancer, Treatment, HIPEC, Cytoreduction, Chemotherapy
INTRODUCTION
The research objects
Life quality of patients with ovarian cancer after complex treatment.
Description of the problem
Ovarian cancer remains a complicated medical issue. According to worldwide statistics, 1-year, 3-year and 5-year survival rates are 63%, 41%, 35% respectively [1]. In the last decade a modest decrease of 5-year survival was caused by more common use of platinum-based chemotherapy for disseminated ovarian cancer [1].
More than 70% cases of ovarian cancer are revealed at late stages, that accounts for poor prognosis. Contemporary treatment standards include combination of surgical cytoreduction and platinum-based chemotherapy. However, even after complete cytoreduction with adjuvant first-line systemic treatment, that achieved complete clinical regression, 5-year survival rates for III and IV stages are 20% and 10% respectively [2].
Suggested way to solve the problem
Most patients respond well to first-line therapy, although 30% may have a platinum-resistant or platinum-refractory tumor. In such cases other cytostatic drug combinations, target therapy and immunotherapy are recommended [3]. To sum up, despite absence of clinical signs, one third of patients after first-line chemotherapy will have relapse in 2-3 years. Objective response rate is 10-25%, median survival time is 7-18 months [4]. Most studies share an opinion, that optimal cytoreduction is crucial for effective treatment. However, only 10-15% of performed surgeries achieve optimal extent. That’s why it is still relevant to improve methods of surgical and adjuvant methods of ovarian cancer treatment [5].
Purpose of the research
The study was conducted to assess the effectiveness of cytoreductive surgery in combination with hyperthermic intraperitoneal chemoperfusion (HIPEC) in advanced stages ovarian cancer management. The article displays the experience of University clinic of Odessa National Medical University.
MATERIALS & METHODS
37 cases of ovarian cancer treated with cytoreduction, HIPEC and 4-6 courses of adjuvant chemotherapy were analyzed. Study has been conducted in the Department of Surgery No 4 with the Course of Oncology (Odessa National Medical University) since 2016 and is continued now. All patients had serosal papillary ovarian cancer FIGO IIIA-IIIC. Patient’s age was 31-59 years, the middle age was 43±7 years old. Control group included 25 patients after surgical treatment and convenient systemic chemotherapy. All patients received suboptimal cytoreduction.
Before including patients in the study protocol, personal written voluntary consents were obtained to participate in the study in accordance with the Helsinki Declaration of the World Medical Association.
Criteria of exclusion were age more than 70 years, extensive carcinomatosis with peritoneal carcinomatosis index more than 20, unresectable small bowel involvement, distant metastasis, retroperitoneal lymphadenopathy, unresectable retroperitoneum invasion, severe concomitant pathology. Previous surgeries with massive adhesions were considered as relative contraindication.
Cytoreduction included visceral resections and peritonectomy. Hysterectomy with bilateral adnexectomy, omentectomy and selective parietal peritonectomy was performed.
In the University clinic of Odessa National Medical University, we perform HIPEC with Performer LRT (Rand, Italy). Its main components are two pumps, heater, infusion lines and digital integrational system. The apparatus controls the procedure automatically and allows fine tuning and monitoring of different parameters like temperature, volume speed, target volumes and timing.
All patients in the main group received HIPEC with cisplatin and doxorubicin. Drugs are dissolved in 5000-6000 ml of isotonic perfusate. We use a closed technique, that is after wound closure 5-6 silicone drains are placed into abdominal and pelvic cavity. Procedures lasted 60-90 min with target intraperitoneal temperature 40-41ºC and volume speed 800-900 ml/min. Mean filling volume is 2500-3000 ml depending of patient’s constitution. The washout phase takes 10-15 min until clear outflow and normothermia is achieved.
All patients received cytoprotection with thiosulfate during HIPEC and 6 h after to prevent systemic toxicity of cisplatin. Usually, patients stayed for one day in the intensive care unit. Perioperative medications include dexamethasone, 5-HT blockers, adequate analgesics and infusional therapy. Antibiotic prophylaxis s protracted for 1-3 days if needed.
Patients were assessed intraoperatively according to peritoneal carcinomatosis index, previous surgical score, cytoreduction completeness score. The quality of life was analyzed with Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). Adverse effects and toxicities were secondary outcomes of the study. Time series statistics were used to analyze the obtained data. To assess the significance of these changes, we used the Mann-Whitney parametric test. SPSS Statistics was used as software for estimating statistics.
RESULTS
Among the main group (n=37) IIIA, IIIB, IIIC stages were revealed in 5, 3 and 29 patients respectively. In the control group (n=25), 10 patients had IIIA, 2 patients - IIIB, 13 patients - IIIC. Carcinomatosis index in the main group was LS-1 (28,0%) and LS-2 (72,0%). It didn`t differ significantly in control group: LS-1 - 36,0%, LS-2 - 64,0%. Cytoreduction completeness score had no statistical difference (CC-1 and CC-2 was 28,0%, 72,0% in main group, 36,0%, 64,0% in control group).
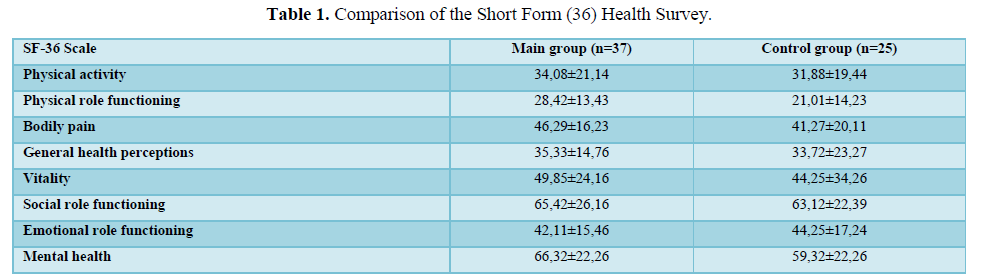
Comparative analysis of quality of life 6 months after treatment completion didn’t showed nonsignificant statistical difference (Table 1).
No allergic and idiosyncratic drug reactions were observed in the main group. 9 patients had temporary hyperthermic reaction, controlled with NSAIDs.
Few patients (n=5, 13,5%) complained about pain around drain contrapertures.
Toxicities comparison of treatment regimens is shown in the Tables 2 and 3.
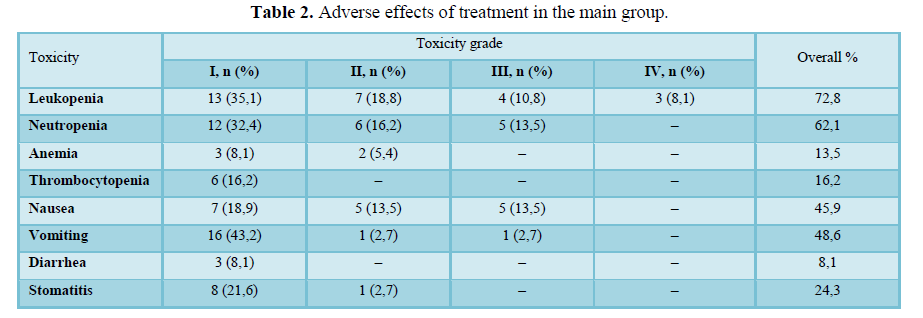
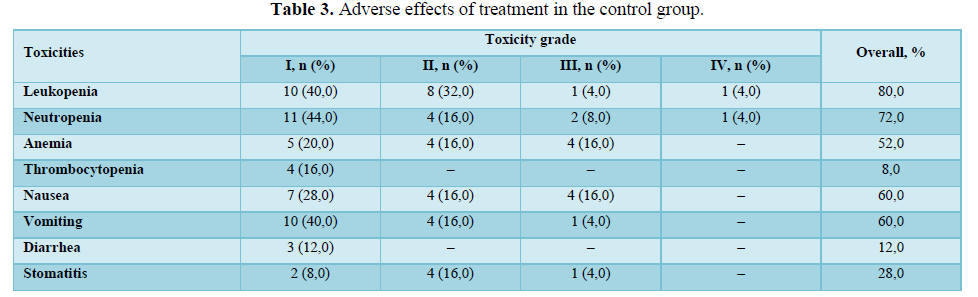
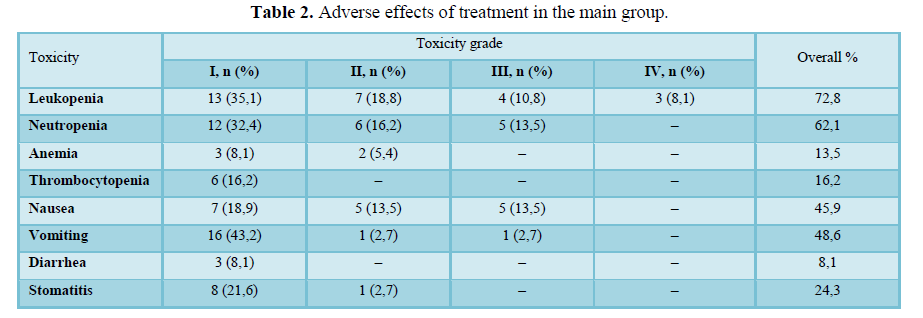
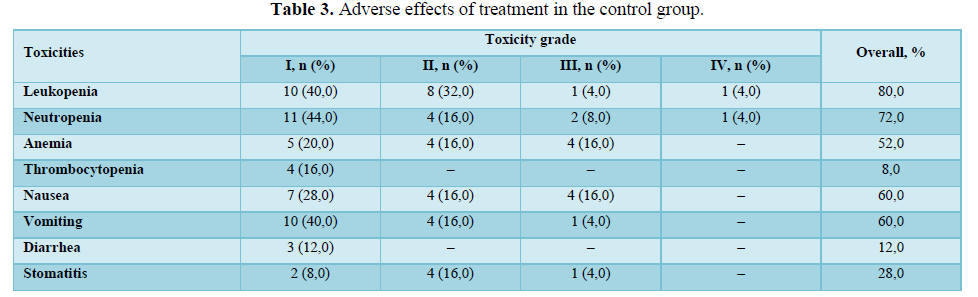
Hematological, gastrointestinal adverse effects were comparable in both groups. Less nephrotoxicity was observed in the control group. Mean hospital stay was 8,9 days in the main group and did not differ significantly from control group.
DISCUSSION
Cytoreduction and HIPEC have a reasonable rationale. Several tumors (ovarian cancer, malignant mesothelioma, colorectal and gastric cancer), that evolve into peritoneal carcinomatosis, in some stages of development are locally contained within serosal lining without giving distant metastases [6]. Macroscopic tumor removal with surgical cytoreduction and microscopic with HIPEC achieves locoregional control.
By definition, chemotherapeutic drugs have various grades of systemic toxicities. Their use in high concentrations may cause serious adverse effects. Regional chemotherapy can achieve high local concentrations without systemic leakage into systemic circulation. Hyperthermia has direct selective cytotoxicity and acts synergistically with alkylating agents, like anthracyclines [7]. In addition, it improves drug penetration into tumor deposits [8]. Continuous cavity chemoperfusion supports constant chemotherapeutic agents’ concentration and equal distribution. These features explain better “local” intraperitoneal control after HIPEC comparing to systemic chemotherapy [9].
The research is continued now, and the new results will be published as soon as possible.
CONCLUSIONS
-
Combination of cytoreduction with HIPEC improves quality of life in patients with ovarian cancer.
-
HIPEC is proven to be effective in conjunction with optimal or suboptimal cytoreduction.
-
HIPEC is tolerated better and has less systemic toxicities in comparison with systemic chemotherapy.
- Zoja FP, Youriy MY, Lyudmyla GO, Yevgeniy GL, Anton RY (2019) Bulletin of National Cancer Registry of Ukraine. Vol 21. Available online at: http://www.ncru.inf.ua/publications/BULL_21/index_e.htm
- Global Cancer Observatory (2020) Available online at: https://gco.iarc.fr/
- Cotte E, Glehen O, Mohamed F, Lamy F, Falandry C, et al. (2007) Cytoreductive surgery and intraperitoneal chemo hyperthermia for chemo resistant and recurrent advanced epithelial ovarian cancer: prospective study of 81 patients. World J Surg 31: 1813-1820.
- Parson EN, Lentz S, Russell G, Shen P, Levine EA, et al. (2011) Outcomes after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal surface dissemination from ovarian neoplasms. Am J Surg 202(4): 481-486.
- Di Giorgio A, Naticchioni E, Biacchi D, Sibio S, Accarpio F, et al. (2018) Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer 113(2): 315-325.
- Bakrin N, Classe JM, Pomel C, Gouy S, Chene G, et al. (2014) Hyperthermic intraperitoneal chemotherapy (HIPEC) in ovarian cancer. J Visc Surg 151: 347-353.
- Onda T, Kobayashi H, Nakanishi T, Hatae M, Iwasaka T, et al. (2009) Feasibility study of neoadjuvant chemotherapy followed by interval debulking surgery for stage III/IV ovarian, tubal, and peritoneal cancers: Japan Clinical Oncology Group Study JCOG0206. Gynecol Oncol 113(1): 57-62.
- Hua TC, Yan TD, Saxena A, Morris DL (2019) Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure? A systematic review of morbidity and mortality. Ann Surg 249: 900-907.
- Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ (2016) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: A meta-analysis. J Clin Oncol 20(5): 1248-1259.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- Journal of Alcoholism Clinical Research
- Dermatology Clinics and Research (ISSN:2380-5609)



