INTRODUCTION
Chronic conditions are long-term health conditions which encompass a broad range of chronic and complex health conditions across the spectrum of illness, including mental illness, trauma, disability and genetic disorders [1]. They are also known as non-communicable diseases and have been described as diseases of long duration that follows a slow progression path [2]. Chronic diseases have been recognized as major killers in modern times owing to their high prevalence and mortality rate. This may not be unconnected with the increasing rate of physical inactivity in recent times [3]. Chronic diseases pose significant and rising challenges for nations of the world today. The burden of disease is shifting away from infectious diseases and injury to chronic conditions which thus requires various management techniques in order to mitigate the attendant challenges rising from them [1,4].
The changing pattern of diseases in urban Africa has been attributed to important factors such as poverty, underdevelopment, poor food and nutrition, insecurity, lack of sanitation and safe water, lack of education, lack of access to basic health care, pressures from tropic environment and ecological burden, climate change, human behavior changes, and economic instability [5,2].
Chronic diseases pose significant and rising socio-economic challenges globally. This challenge pervades both developed and developing countries.
Employers of labour have to pay high costs for chronic diseases in staff welfare costs, health insurance costs and reduced productivity often resulting from absenteeism. Chronic diseases lead to multiple death, reduced quality of life and high cost of living among people who have them. These tend to drive up costs and also lead to increased demand for health care.
The burden of chronic diseases can be lessened by integrated approaches targeted at lessening risk factors and conditions. Additionally, important strategies involving epidemiology and surveillance, environmental approaches, health system interventions and community resources that can improve the management of chronic conditions have also been advocated [6].
The onset of chronic diseases is often from lifestyle choices that are common with contemporary society and this explains their high prevalence in the world today. Four main categories of chronic diseases including cardiovascular diseases (CVDs), chronic respiratory diseases, diabetes and cancers have been recognized [7]. The World Health Organization reported that 40 million out of the 56 million global deaths in 2015 were due to non-communicable diseases [8]. Also, about 80% of these deaths occur in low-and middle-income countries while 48% of these deaths occur before the age of 70 [5,8]. Further reports from NASAC (2015) show that two-thirds of people living with hypertension are in low-middle income countries and the condition is estimated to affect one-quarter of the African adult population. The World Economic Forum reported a possible rise in death from chronic/non-communicable diseases over the next decade and the increase is expected to lead to more than 10 million deaths [9].
The burden of chronic diseases has been on an increase, even on a global scale. This is basically due to the incidence and prevalence of chronic conditions and risk factors as well as demographics such as age and health status [6]. The burden of chronic diseases is no less prevalent in Nigeria like other African countries. An approximate of 12% of the Nigerian population has mortality arising from chronic diseases. Nigeria is the most populous country in Africa with population exceeding 200 million with to 50% of which live in the rural areas [10]. Access to health and access to health and quality of healthcare services differ between rural and urban communities. This difference has been demonstrated in several studies [11]. In Nigeria, while there is a general prevalence of insufficient healthcare facilities in many health institutions, the situation is more challenging in the rural areas when compared to the urban areas given that the rural communities not only face more dire need for standardized healthcare facilities, the residents are also often not able to pay for these services.
However, this prevalence of chronic diseases has not been well documented in literature. Hence, this study seeks to examine the morbidity pattern of chronic diseases in an urban community in Rivers State, Nigeria.
METHODS
A descriptive research design was adopted in accomplishing the objectives of this study. The quantitative data was obtained from all the hospital records of patients with chronic diseases from 2013 to 2017 in the University of Port-Harcourt Teaching Hospital, East-West Road, Port-Harcourt, Rivers State, Nigeria. Data collected included the patients’ age, sex, marital status, occupation, religion and diagnosed ailment. Appropriate statistical tools were adopted in presenting the data for the study and also for testing the study hypotheses.
Data collection procedure
Two hospitals were visited and management was presented with the ethical clearance, with the aims and objectives of the project and Cases (hospital records) from 2013 to 2017 was carefully selected from the hospital individually. In the final stage, a proportionate sample of records of chronic diseases were purposely chosen from each of the selected hospitals to adequately represent cases of chronic diseases within the selected area of study. Due to how cumbersome the records were, one in every 10 (ten) cases was picked.
Ethical considerations
Ethical approval was obtained from the Rivers State Ministry of Health and from the Ethics Committee of the respective hospitals with proper explanation of the purpose of the research.
RESULTS
Characteristics of patients
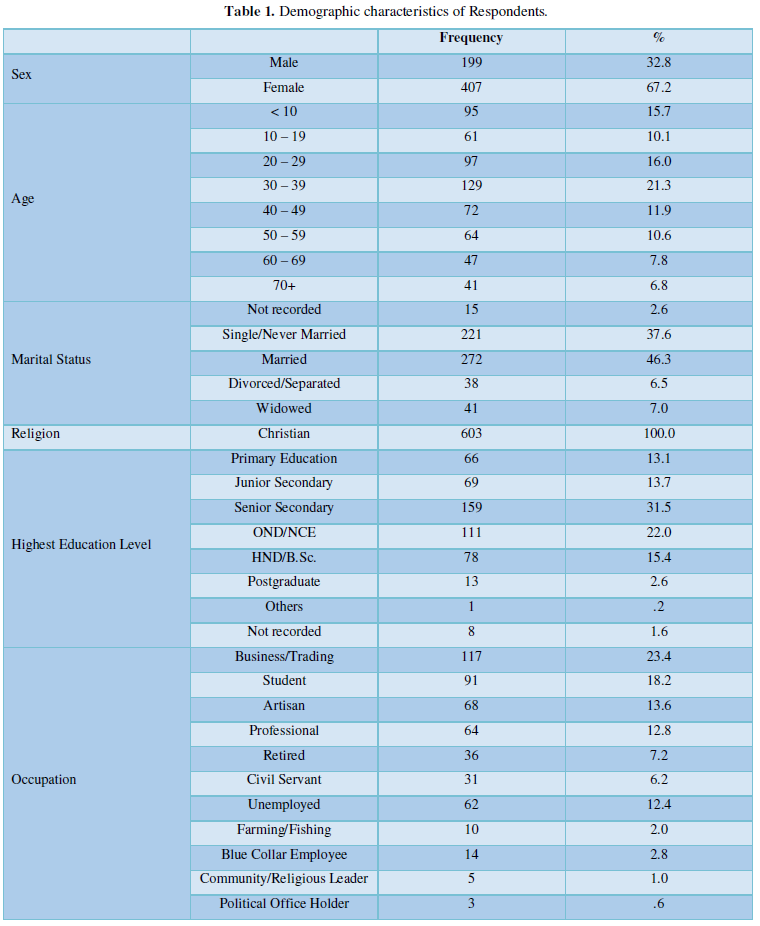
Majority of the patients were female (67.2%) and were either single/never married (37.6%) or married (46.3%). The distribution of age showed that most of the patients were aged 30 – 39 years followed by those who were 20-29 years. All the patients were Christian while they were educated mostly up to senior secondary school level (31.5%) or OND/NCE (22.0%). Majority of the patients were engaged in business/trading (23.4%) or they were students (18.3%) (Table 1).
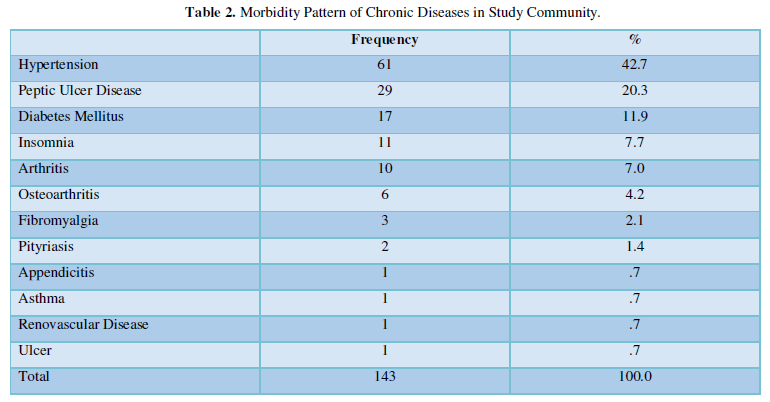
Pattern of chronic diseases
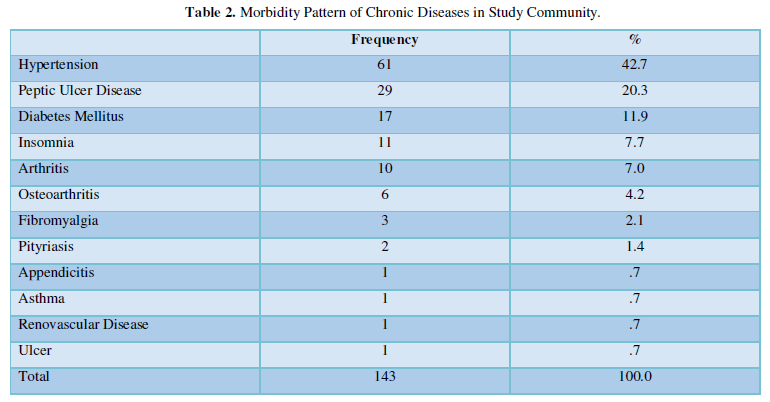
Hypertension (42.7%) was the most prevalent chronic disease in the community, followed in order by Peptic Ulcer disease (20.3%) and Diabetes Mellitus (11.9%) Insomnia (7.7%), Arthritis (7.0%), and osteoarthritis (4.2%), Fibromyalgia (2.1%), Pityriasis (1.4%), Appendicitis (0.7%),Asthma (0.7%), Renovascular disease (0.7%) and Ulcer (0.7%) (Table 2).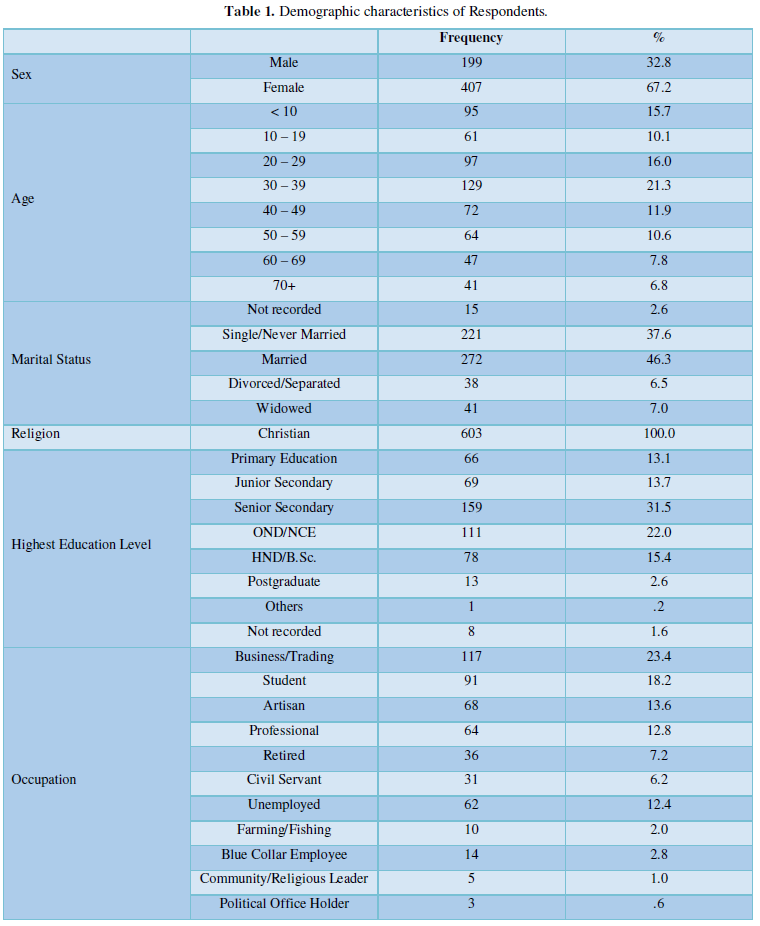
Sex and chronic diseases
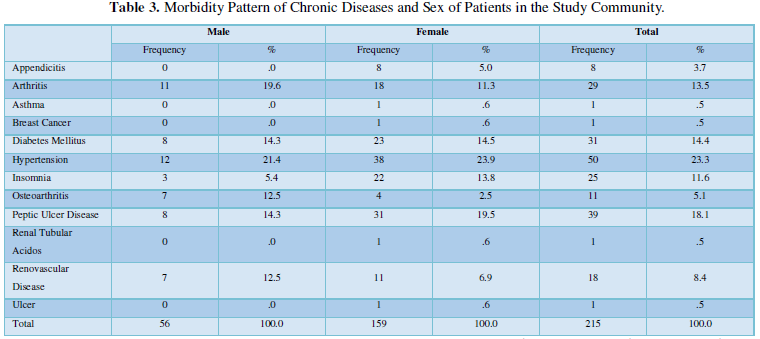
Among the male patients, diseases such as Hypertension (21.4%), Arthritis (19.6%), Diabetes Mellitus (14.3%), Peptic Ulcer Disease (14.3%), Osteoarthritis (12.5%), Renovascular disease (12.5%) and Insomnia were prevalent among the male patients. On the other hand, female patients had higher prevalence of Hypertension (23.9%), Peptic Ulcer Disease (19.5%), Diabetes Mellitus (14.5%), Insomnia (13.8%), and Arthritis (11.3%), as well as Renovascular disease (6.9%), appendicitis (5.0%), asthma (0.6%), breast cancer (0.6%), renal tubular acidosis (0.6%), and ulcer (0.6%) (Table 3).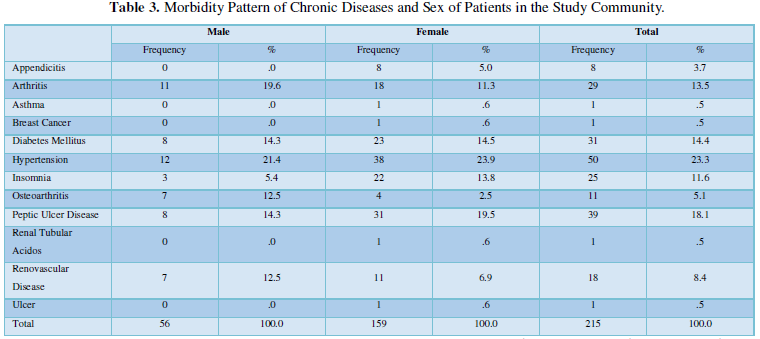
Age and chronic diseases
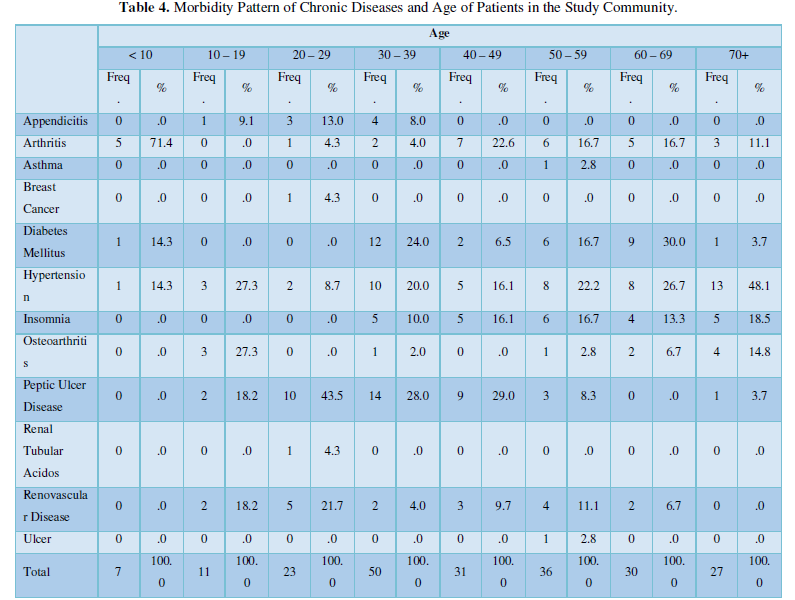
The most prevalent chronic diseases among patients less than 10 years were arthritis (71.4%), diabetes mellitus (14.3%) and hypertension (14.3%) (Table 4).
Among patients aged 10 – 19 years, the prominent diseases included Hypertension (27.3%), Osteoarthritis (27.3%), peptic ulcer disease (18.2%), Renovascular disease (18.2%) and Appendicitis (9.1%). Among patients aged 20-29 years, the most prominent diseases were Appendicitis (13.0%), Arthritis (4.3%), breast cancer (4.3%) hypertension (8.7%), Peptic Ulcer Disease (43.5%), Renal Tubular Acidosis (4.3%) and Renovascular Disease (21.7%). Also, among patients aged 30-39 years, the most prominent diseases include Appendicitis (8.0%), Arthritis (4.0%), Diabetes mellitus (24.0%), Hypertension (20.0%), Insomnia (10.0%), Osteoarthritis (2.0%), Peptic Ulcer Diseases (28.0%), and Renovascular disease (4.0%).
Among patients aged 40-49 years the most prominent diseases were arthritis (22.6%), Diabetes Mellitus (6.5%), Hypertension (16.1%), Insomnia (16.1%), Peptic Ulcer Disease (29.0%) and Renovascular disease (9.7%). Among patient between the age of 50-59 years, the most prominent disease includes Arthritis (16.7%), Asthma (2.8%), Diabetes mellitus (16.7%), Hypertension (22.2%), Insomnia (16.7%), Osteoarthritis (2.8%), Peptic Ulcer (8.3%), Renovascular disease (11.1%) and Ulcer (2.8%).
Furthermore, among patients aged 60-69 years the following diseases were the most prominent Arthritis (16.7%), Diabetes mellitus (30.0%), Hypertension (26.7%), Insomnia (13.3%), Osteoarthritis (6.7%) and Renovascular Disease (6.7%). However, among patient aged 70 and above the most prominent diseases include Arthritis (11.1%), Diabetes Mellitus (3.7%), Hypertension (48.1%), and Insomnia (18.5%) Osteoarthritis (14.8%) and peptic Ulcer (3.7%).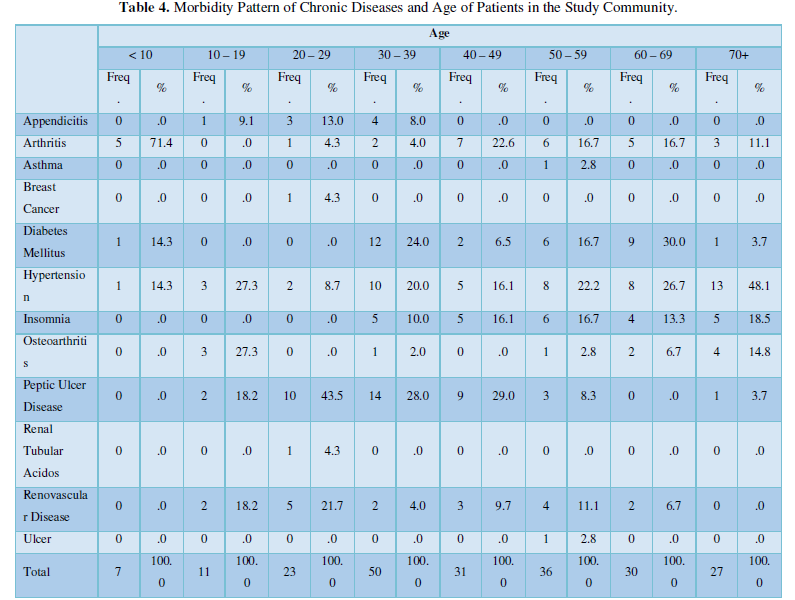
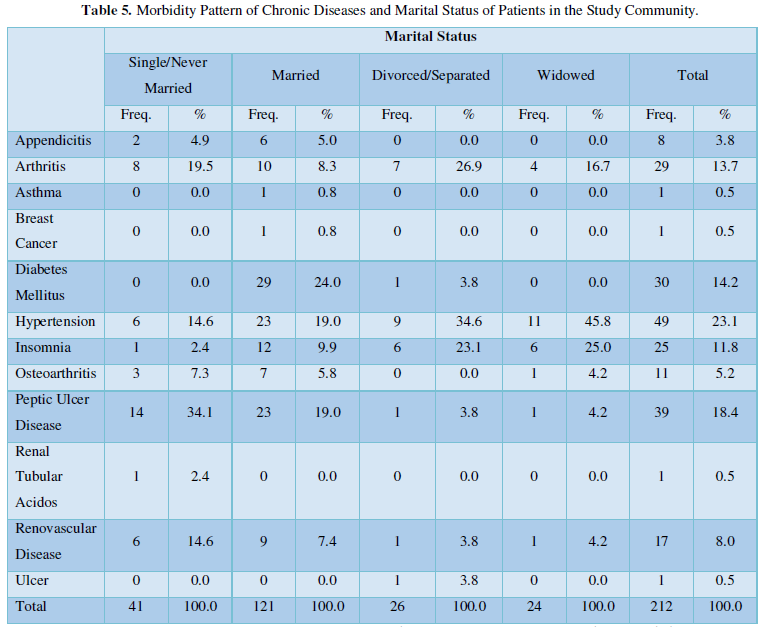
Marital status and chronic diseases
The result in Table 5 shows that the most prominent disease among patient that were single /Never married include Appendicitis (4.9%), Arthritis (19.5%), Hypertension (14.6%) Insomnia (2.4%), Osteoarthritis (7.3%), Peptic Ulcer (34.1%), Renal Tubular Acidosis (2.4 %) and Renovascular disease (14.6%). Among patient that were married, the most prominent diseases include Appendicitis (5.0%), Arthritis (8.3%), Asthma (0.8%), Breast cancer (0.8%) Hypertension (19.0%) Diabetes mellitus (24.0%) Insomnia (9.9%), Osteoarthritis (5.8%), Peptic Ulcer (19.0%) and Renovascular disease (7.4%). Among patient that were divorced/separated the most prevalent disease include Arthritis (26.9%), Diabetes mellitus (3.8%), Hypertension (34.6%) Insomnia (23.1%), Peptic Ulcer (3.8%), Renovascular disease (3.8%) and Ulcer (3.8%).
Among patients that were widowed, the most prevalent disease includes Arthritis (16.7%), Hypertension (45.8%) Insomnia (25.0%), Osteoarthritis (4.2%), Peptic Ulcer (4.2%) and Renovascular disease (4.2%).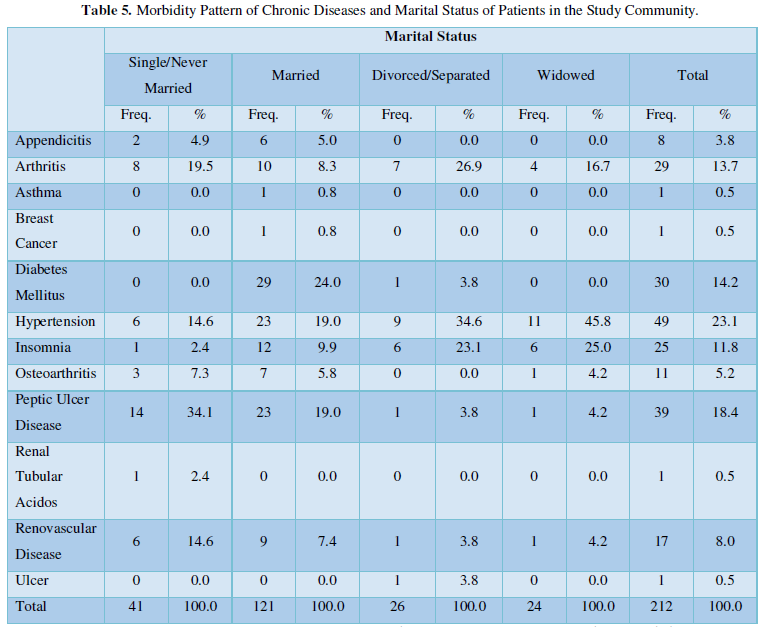
DISCUSSION
There is an increasing prevalence of chronic diseases which has been linked to increasing population of elderly persons on a global scale [2]. The increasing burden of chronic diseases will constitute a major global public health concern since non-communicable diseases are responsible for over two-thirds of global deaths [6]. Additionally, the increasing prevalence has been linked to the health, economic growth and development of nations while causing a terrible strain on social welfare and health systems of most nations of the world [2].
Assessment of the study results revealed that the most prevalent chronic diseases in order of prevalence included hypertension, peptic ulcer disease, diabetes mellitus, insomnia, arthritis, osteoarthritis, fibromyalgia, pityriasis, appendicitis, asthma, renovascular disease and ulcer. These diseases fall within the four main classifications of chronic diseases [8].
An assessment of participants’ sociodemographic characteristics and the morbidity pattern of chronic diseases was made. The first sociodemographic factor assessed was the sex of the patients. The study findings showed that male patients had higher prevalence of hypertension, arthritis, diabetes mellitus, peptic ulcer disease, osteoarthritis, renovascular disease and insomnia. Among the female patients, the most prevent were hypertension, peptic ulcer disease, diabetes mellitus, insomnia, arthritis, renovascular disease, appendicitis, asthma, breast cancer, renal tubular acidosis and ulcer. Overall, hypertension was highly prominent among both males and females in the community. A previous study had reported that the female gender was a major predictor of developing chronic diseases [2].
The second sociodemographic factor that was observed was the age of the respondents. The findings showed that patients aged less than 10 years had arthritis, diabetes mellitus and hypertension while those aged 10–19 years had higher prevalence of hypertension, osteoarthritis, peptic ulcer disease, renovascular disease and appendicitis. Patients aged 20–29 mostly had peptic ulcer and renovascular disease while those aged 30–39 years had prevalence of peptic ulcer disease, diabetes mellitus, hypertension, insomnia, appendicitis, arthritis and renovascular disease. Also, among patients aged 40–49, majority of the patients had peptic ulcer disease, arthritis, hypertension or insomnia. Other diseases included diabetes mellitus, and renovascular disease among the rural dwellers.
Patients aged 50–59 years were mainly afflicted with hypertension, as well as diabetes mellitus, arthritis, diabetes mellitus, insomnia and renovascular disease. Others include asthma, osteoarthritis, peptic ulcer disease and ulcer in the rural community. Patients aged 60–69 years mostly had diabetes mellitus, hypertension, arthritis, insomnia, osteoarthritis and renovascular disease while those aged 70 years and above mostly had hypertension, followed in order by insomnia, osteoarthritis, arthritis, diabetes mellitus and peptic ulcer disease.
Generally, the findings showed that higher prevalence of chronic diseases occur with increasing age of the patients. This finding is comparable to similar studies [12,2]. Given that chronic diseases are associated mostly with unhealthy lifestyle practices, it could therefore be well subsumed that as people get old, the effects of poor lifestyle practices begin to manifest in the emergence of various forms of chronic diseases. By implication, individuals need to take cognisance that seemingly harmless activities in early years or even day to day life, pose risk to future health. Furthermore, as the individuals seem to increase in age, there seem to be increasing similarity in the pattern of chronic diseases among them. The impact of age as well as financial burden has been reported in previous studies as elderly persons with chronic diseases are known to have a higher financial burden relative to those without chronic diseases [2].
The third sociodemographic factor observed was the respondents’ marital status against the morbidity pattern of chronic diseases. The findings showed that peptic ulcer, arthritis, hypertension, and renovascular disease were the prominent ailments of single/never married patients whereas among the married patients, they were mainly diagnosed of diabetes mellitus, hypertension and peptic ulcer disease among some others. Divorced/separated patients were primarily diagnosed with hypertension, arthritis and insomnia among few minor other ailments while widowed patients, primarily had hypertension, peptic ulcer disease and arthritis. The relationship between marital status and health outcomes varies on a gender specific basis. Being unmarried was a significant risk factor for hypertension and mortality in men while being widowed was linked to a reduced risk of type 2 diabetes mellitus in women [13]. However, another study reported no association of marital status with morbidity from chronic diseases [12]. Taken together, the findings of this study are comparable to other previous studies in Vietnamese populations that have reported sex, education and age as important predictors of chronic diseases [14,12,15].
CONCLUSION
This study reports that hypertension, appendicitis, arthritis, breast cancer, diabetes mellitus, insomnia, osteoarthritis, peptic ulcer disease, renal tubular acidosis and renovascular disease are the predominant chronic diseases in the study population. The onset and morbidity of these diseases was associated with socio-demographic characteristics such as sex, age, marital status and level of education. Therefore, this study recommends an urgent public health action through public enlightenment on healthy lifestyle patterns in order to lessen the burden of chronic diseases in the study population.