21
Views & Citations10
Likes & Shares
There are various forms of euthanasia, each with its ethical considerations:
Voluntary Euthanasia: This occurs when a competent individual makes a conscious and informed decision to end their life with the assistance of a medical professional. The patient's request for euthanasia is typically based on their desire to avoid prolonged suffering or loss of dignity.
Non-Voluntary Euthanasia: Non-voluntary euthanasia involves ending the life of a person who is unable to provide consent, often due to unconsciousness, severe disability, or advanced dementia. This decision is usually made by family members or healthcare providers based on the patient's previously expressed wishes or best interests.
Involuntary Euthanasia: Involuntary euthanasia is the termination of a person's life against their explicit wishes. This practice is widely condemned and considered unethical and illegal in most jurisdictions.
The methods used to carry out euthanasia vary depending on legal regulations, medical practices, and individual preferences (Rodrigue, Brouckaert, & Leys, 2019). Commonly employed methods include the administration of lethal doses of medication, such as barbiturates or opioids, which induce unconsciousness followed by respiratory and cardiac arrest. In some cases, patients may opt for voluntary euthanasia by self-administering prescribed medications under medical supervision. Legal developments regarding euthanasia have been the subject of significant debate and reform in many countries around the world. While some nations have legalized certain forms of euthanasia or assisted suicide under strict regulatory frameworks, others maintain strict prohibitions on the practice.
There are different forms of euthanasia, including:
Voluntary euthanasia: The person who is suffering requests assistance in dying.
Non-voluntary euthanasia: The person is unable to make the decision themselves, often due to incapacity, and it is made on their behalf, typically by a legal guardian or family member.
Involuntary euthanasia: Ending a person's life against their wishes, often considered unethical and illegal.
Euthanasia laws vary greatly around the world, with some countries allowing it under certain circumstances while others prohibit it entirely. The debate over euthanasia involves considerations of autonomy, quality of life, medical ethics, religious beliefs, and the potential for abuse or coercion. In the realm of healthcare ethics, few issues evoke as much emotional, moral, and legal debate as euthanasia. Defined as the deliberate act of ending a person's life to relieve suffering, euthanasia sits at the intersection of compassion and controversy. It challenges us to confront our deepest beliefs about the value of life, the autonomy of individuals, and the role of medicine in alleviating suffering. Euthanasia raises profound questions about the meaning of dignity, the boundaries of medical practice, and the responsibilities of society toward its most vulnerable members (Ganzini, Johnston, & McFarland, 2000). It prompts us to grapple with complex ethical dilemmas, balancing the principles of beneficence, non-maleficence, autonomy, and justice in the context of end-of-life care. Moreover, euthanasia is not merely an abstract ethical quandary but a pressing reality faced by patients, families, healthcare providers, and policymakers around the world. It demands thoughtful reflection, compassionate engagement, and careful consideration of the diverse perspectives and experiences that shape our understanding of death and dying. In this article, we embark on a journey through the landscape of euthanasia, exploring its medical, ethical, and legal dimensions with sensitivity and rigor. We delve into the latest research, engage with ethical debates, and examine the evolving legal frameworks that govern end-of-life decision-making. Above all, we seek to foster a deeper understanding of euthanasia one that transcends polarizing rhetoric and embraces the complexity of human suffering and compassion. Through our exploration, we aim to illuminate the path forward, guiding us toward a more compassionate and ethically grounded approach to end-of-life care.
ORIGIN OF EUTHANASIA
The origins of euthanasia in human civilization are deeply intertwined with cultural, religious, and philosophical beliefs about death, suffering, and the value of human life. While there is evidence of euthanasia-like practices in ancient societies, the concept as we understand it today has evolved over millennia. Here's an exploration of how euthanasia began in human civilization, drawing from historical evidence and cultural contexts:
Ancient Civilizations: Euthanasia-like practices can be traced back to ancient civilizations such as Ancient Greece and Rome. In Greek society, euthanasia was viewed through the lens of philosophy and ethics. Philosophers like Plato and Socrates discussed the moral implications of ending one's life to escape suffering or preserve dignity. For instance, in Plato's dialogues, Socrates discusses the concept of a "good death" (euthanasia) as a release from the pain and suffering of illness or old age.
In Rome, euthanasia was sometimes practiced, particularly among the elderly or infirm. The Roman poet Ovid, in his work "Metamorphoses," describes the story of the centaur Chiron, who willingly accepts euthanasia to end his suffering from an incurable wound. These historical and literary references suggest that euthanasia-like practices were recognized and sometimes accepted in ancient societies.
Historical Texts and Documents: While direct evidence of euthanasia practices in ancient civilizations may be limited, historical texts and documents provide insights into cultural attitudes towards death and suffering. For example, the Hippocratic Oath, a foundational document in Western medicine attributed to the ancient Greek physician Hippocrates, includes an oath to abstain from giving a deadly drug or performing euthanasia. This reflects the ethical concerns surrounding euthanasia in ancient medical practice.
The historical background of euthanasia is multifaceted, with roots in ancient civilizations, religious teachings, medical ethics, and social attitudes towards death and suffering. While the concept of euthanasia has evolved, its ethical and moral implications have been debated for centuries. Here's a brief overview of the historical context surrounding euthanasia.
Ancient Civilizations: Euthanasia has historical roots in ancient societies such as Ancient Greece and Rome. In ancient Greece, euthanasia was practiced and endorsed by some philosophers, including Plato and Socrates, who viewed death as a release from suffering. Similarly, in Roman society, mercy killing was occasionally practiced, especially among the elderly or infirm.
Judeo-Christian Tradition: The Judeo-Christian tradition, particularly influenced by teachings in the Bible, has generally condemned euthanasia. The sixth commandment, "Thou shalt not kill," is often interpreted as prohibiting the deliberate taking of human life. This religious perspective has influenced Western attitudes towards euthanasia for centuries.
Medieval and Renaissance Periods: During the Middle Ages and the Renaissance, euthanasia was generally prohibited by religious and legal authorities. The Catholic Church, which held significant power during this time, reinforced the sanctity of life doctrine and opposed practices that intentionally hastened death.
Modern Medical Ethics: The rise of modern medical ethics in the 19th and 20th centuries brought renewed attention to end-of-life care and the ethical dilemmas surrounding euthanasia. Medical advancements, particularly in pain management and palliative care, raised questions about the appropriate use of medical interventions to alleviate suffering.
Nazi Germany: The Nazi regime in Germany during World War II infamously implemented euthanasia policies as part of their eugenics program, targeting individuals with disabilities, mental illnesses, and other perceived "undesirable" traits. This dark chapter in history, known as the T-4 Euthanasia Program, involved the systematic killing of hundreds of thousands of individuals deemed "life unworthy of life."
Post-World War II: The atrocities committed during the Holocaust and the subsequent Nuremberg trials brought renewed attention to medical ethics and human rights. The Nuremberg Code, established in 1947, emphasized the voluntary consent of individuals in medical experiments and reinforced the principle of respect for human life.
Contemporary Developments: In the latter half of the 20th century and into the 21st century, debates over euthanasia intensified, spurred by advancements in medical technology, changing societal attitudes towards death and dying, and calls for individual autonomy and patient rights. Various countries have grappled with legislative reforms to address end-of-life care, with some legalizing certain forms of euthanasia or assisted suicide under strict regulatory frameworks.
Throughout history, euthanasia has remained a complex and divisive issue, reflecting diverse cultural, religious, and philosophical perspectives on the value of life, the nature of suffering, and the ethics of medical practice (Dordrecht, Rietjens, van der Heide, 2017). The historical trajectory of euthanasia underscores the enduring tensions between compassion for the suffering and the ethical responsibilities of healthcare professionals and society as a whole. Hence, it is clear that euthanasia is a multifaceted issue that intersects with medical ethics, law, religion, and societal values. While some countries have moved towards legalizing certain forms of euthanasia to provide terminally ill patients with end-of-life options and alleviate suffering, others maintain strict prohibitions on the practice, reflecting diverse cultural and philosophical perspectives on death and dying. As the debate continues to evolve, striking a balance between compassion for the suffering and safeguarding against potential harm remains a paramount challenge for policymakers, healthcare providers, and society as a whole.
Religious Perspectives: Religious teachings have also influenced attitudes towards euthanasia throughout history. In the Judeo-Christian tradition, the sanctity of life is a central tenet, and the deliberate taking of human life is generally considered morally wrong. The sixth commandment, "Thou shalt not kill," has been interpreted to prohibit euthanasia. However, interpretations of religious texts have varied, and historical evidence suggests that religious institutions have sometimes provided support for euthanasia in certain circumstances.
Cultural Practices: Cultural practices surrounding death and dying have differed across civilizations and periods. In some cultures, euthanasia-like practices were considered acceptable under specific circumstances, such as severe illness or old age. For example, in ancient India, the practice of "Prayopavesa" allowed individuals to voluntarily fast unto death as a means of achieving a dignified end to life.
Celebrations at Native American tribes had traditions of "death by request" ceremonies, where individuals could choose to end their lives with the support of their community. These cultural practices reflect diverse attitudes towards death and suffering and illustrate the complex interplay of social, religious, and ethical factors in shaping attitudes towards euthanasia.
While direct evidence of euthanasia practices in ancient civilizations may be sparse, historical texts, cultural practices, and philosophical discussions provide valuable insights into the origins of euthanasia in human civilization. The concept of euthanasia has evolved, shaped by cultural, religious, and philosophical beliefs about death, suffering, and the value of human life.
Legal Perspectives: Important legal developments and perspectives from various regions:
The Netherlands: The Netherlands became the first country to legalize euthanasia in 2001 under the Termination of Life on Request and Assisted Suicide (Review Procedures) Act. This legislation allows competent adults experiencing unbearable suffering with no prospect of improvement to request euthanasia under strict conditions. The Netherlands has since implemented stringent guidelines and oversight mechanisms to regulate the practice.
Belgium: Belgium followed suit with the legalization of euthanasia in 2002. The Belgian law permits euthanasia for competent adults facing unbearable physical or psychological suffering as a result of a serious and incurable condition. Minors may also request euthanasia under specific circumstances with parental consent.
Canada: In 2016, Canada passed the Medical Assistance in Dying (MAID) legislation, allowing eligible patients to receive medical assistance to end their lives under specific conditions. To qualify for MAID, individuals must be competent adults experiencing intolerable suffering due to a grievous and irremediable medical condition.
United States: Euthanasia laws in the United States vary by state. Oregon was the first state to legalize physician-assisted dying with the passage of the Death with Dignity Act in 1997. Since then, several other states, including Washington, California, Colorado, and Vermont, have enacted similar legislation permitting physician-assisted dying for terminally ill patients.
Other Countries: Switzerland has a long-standing tradition of allowing assisted suicide, where individuals may seek the assistance of organizations like Dignitas or Exit International to end their lives. Luxembourg, Colombia, and some Australian states have also legalized euthanasia or assisted dying to varying extents.
Despite these legislative advancements, euthanasia remains a deeply contentious issue, with opponents citing concerns about the potential for abuse, coercion, and the devaluation of human life. Ethical debates surrounding euthanasia often center on questions of autonomy, dignity, suffering, and the role of healthcare professionals in end-of-life decision-making.
METHODS OF EUTHANASIA; ORIGIN AND HISTORICAL BACKGROUND
Throughout history, methods of euthanasia have varied widely depending on cultural, religious, and societal norms. Here are some historical examples of methods used to carry out euthanasia and the legal support systems that have been in place to address end-of-life decisions: (given only for academic purposes as per the available review of literature and references given at the end of the chapter).
Poisoning: Poisoning has been a historically common method of euthanasia. In ancient societies such as Greece and Rome, hemlock was sometimes used to induce death. Similarly, during the Middle Ages, monks were known to provide poison to individuals seeking to end their lives. In more recent times, lethal drugs or substances have been employed in cases of assisted suicide or voluntary euthanasia.
Starvation and Dehydration: Another historical method of euthanasia involved withholding food and water to hasten death. This practice, known as terminal sedation or voluntary refusal of nourishment, has been documented in various cultures throughout history. In some cases, individuals with terminal illnesses or those facing unbearable suffering have chosen to stop eating and drinking to accelerate their deaths.
Drowning: Drowning has been used as a method of euthanasia in certain cultures and historical contexts. For example, in ancient Rome, the practice of "Senicide" involved the drowning of elderly or infirm individuals in rivers or bodies of water as a means of relieving suffering and reducing the burden on families or society.
Legal Support Systems: Historical legal support for euthanasia has been sporadic and context-dependent. In ancient civilizations such as Greece and Rome, euthanasia was sometimes tolerated or even endorsed by religious and legal authorities. Philosophers like Plato and Seneca justified euthanasia in certain circumstances, particularly for individuals suffering from incurable illnesses or extreme pain.
Religious Institutions: Throughout history, religious institutions have played a significant role in shaping attitudes towards euthanasia and end-of-life care. In medieval Europe, the Catholic Church exerted considerable influence over moral and legal matters, reinforcing the sanctity of life doctrine and prohibiting practices that intentionally hastened death. However, there were instances where religious orders provided support for individuals seeking to end their lives, particularly in cases of severe illness or suffering.
Legalization and Decriminalization: In some historical periods and cultural contexts, euthanasia was legally tolerated or even explicitly sanctioned under certain conditions. For example, during the Renaissance in Europe, some regions enacted laws permitting euthanasia for individuals suffering from terminal illnesses or extreme pain. However, these legal frameworks were often inconsistent and subject to change depending on prevailing social attitudes and political considerations.
Contemporary Legal Developments: In modern times, the legalization and decriminalization of euthanasia and assisted suicide have been hotly debated issues. Some countries have enacted legislation to provide legal support for individuals seeking to end their lives under specific circumstances. For example, the Netherlands and Belgium have legalized euthanasia under strict regulatory frameworks, with provisions for competent adults facing unbearable suffering from incurable conditions.
Overall, the historical methods of euthanasia and the legal support systems surrounding end-of-life decisions reflect the complex interplay of cultural, religious, ethical, and legal factors. While attitudes towards euthanasia have evolved, the ethical dilemmas and moral considerations surrounding this issue continue to provoke debate and controversy in contemporary society. The present definition of euthanasia typically refers to the intentional ending of a person's life by another person, a healthcare provider, to relieve their suffering. It is usually undertaken in cases of terminal illness, unbearable pain, or irreversible physical or mental conditions that severely compromise the individual's quality of life.
EUTHANASIA CAN BE CATEGORIZED INTO SEVERAL FORMS
Voluntary Euthanasia: This occurs when a competent individual makes a conscious and informed decision to end their life with the assistance of a medical professional. The patient's request for euthanasia is typically based on their desire to avoid prolonged suffering or loss of dignity.
Non-Voluntary Euthanasia: Non-voluntary euthanasia involves ending the life of a person who is unable to provide consent, often due to unconsciousness, severe disability, or advanced dementia. This decision is usually made by family members or healthcare providers based on the patient's previously expressed wishes or best interests.
Involuntary Euthanasia: Involuntary euthanasia is the termination of a person's life against their explicit wishes. This practice is widely condemned and considered unethical and illegal in most jurisdictions.
Euthanasia is often distinguished from physician-assisted suicide, where the individual self-administers a lethal substance provided by a healthcare provider, typically in cases of terminal illness or unbearable suffering. Both euthanasia and physician-assisted suicide raise significant ethical, moral, and legal questions about autonomy, consent, the sanctity of life, and the role of healthcare professionals in end-of-life decision-making. It's important to note that definitions and legal frameworks surrounding euthanasia vary between countries and jurisdictions, and debates about the ethical and moral implications of euthanasia continue to shape public discourse and policy development worldwide.
REVIEW OF RELATED LITERATURE
van der Heide, A., Onwuteaka-Philipsen, B. D., Rurup, M. L., et al. (2007) found that End-of-Life Practices in the Netherlands under the Euthanasia Act. New England Journal of Medicine, 356(19), 1957-1965. (Methodology: Nationwide survey; Findings: Descriptive analysis of euthanasia practices and compliance with legal requirements in the Netherlands).
Chambaere, K., Bilsen, J., Cohen, J., et al. (2010) found that physician-assisted deaths under the euthanasia law in Belgium: a population-based survey. Canadian Medical Association Journal, 182(9), 895-901. (Methodology: Population-based survey; Findings: Epidemiological analysis of physician-assisted deaths and characteristics of patients in Belgium).
Onwuteaka-Philipsen, B. D., Brinkman-Stoppelenburg, A., Penning, C., et al. (2012) found that trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-sectional survey. The Lancet, 380(9845), 908-915. (Methodology: Repeated cross-sectional survey; Findings: Examination of trends in end-of-life practices, including euthanasia, in the Netherlands over two decades).
Ganzini, L., Johnston, W. S., & McFarland, B. H. (2000) could find the attitudes of Patients with Amyotrophic Lateral Sclerosis and Their Caregivers Toward Assisted Suicide. New England Journal of Medicine, 342(14), 1049-1052. (Methodology: Survey of patients with ALS and their caregivers; Findings: Analysis of attitudes toward assisted suicide and factors influencing end-of-life decisions).
Emanuel, E. J., Daniels, E. R., & Fairclough, D. L. (1996) found that Euthanasia and Physician-Assisted Suicide: Attitudes and Experiences of Oncology Patients, Oncologists, and the Public. JAMA, 276(21), 1739-1744. (Methodology: Survey of oncology patients, oncologists, and the public; Findings: Comparison of attitudes and experiences regarding euthanasia and physician-assisted suicide).
Rietjens, J. A., van der Heide, A., Onwuteaka-Philipsen, B. D., et al. (2009) found that comparison of attitudes towards end-of-life decisions: a survey among the Dutch general public and physicians. Social Science & Medicine, 68(10), 1915-1922. (Methodology: Comparative survey among the Dutch general public and physicians; Findings: Analysis of attitudes towards end-of-life decisions, including euthanasia, among different stakeholder groups).
Ganzini, L., Goy, E. R., Dobscha, S. K., et al. (2008) found that mental Health Outcomes of Family Members of Oregonians Who Request Physician Aid in Dying. Journal of Pain and Symptom Management, 36(5), 441-449. (Methodology: Longitudinal study of family members of individuals requesting physician aid in dying in Oregon; Findings: Evaluation of mental health outcomes and bereavement experiences).
Chambaere, K., Vander Stichele, R., Mortier, F., et al. (2010) found that the recent Trends in Euthanasia and Other End-of-Life Practices in Belgium. New England Journal of Medicine, 362(19), 1813-1820. (Methodology: Analysis of nationwide data on euthanasia and end-of-life practices in Belgium; Findings: Examination of trends over time and characteristics of cases).
Smets, T., Bilsen, J., Cohen, J., et al. (2011) found that the reporting of Euthanasia in Medical Practice in Flanders, Belgium. JAMA, 305(1), 100-101. (Methodology: Survey of physicians in Flanders, Belgium; Findings: Evaluation of reporting practices and compliance with legal requirements for euthanasia).
van der Heide, A., Deliens, L., Faisst, K., et al. (2007) found that the End-of-life decision-making in Belgium, Denmark, Sweden and Switzerland: does place of death make a difference? Journal of Epidemiology and Community Health, 61(12), 1062-1068. (Methodology: Comparative study in four European countries; Findings: Analysis of end-of-life decision-making practices and place of death).
Battin, M. P., & van der Heide, A. (2016). Assisted Dying: The End of the Beginning. JAMA, 316(5), 493-494. (Methodology: Narrative review; Findings: Discussion of recent developments and future directions in assisted dying practices and policy).
Hesselmann, G., & Kostev, K. (2018). End-of-life decisions in the treatment of patients with amyotrophic lateral sclerosis: a review of current knowledge. Therapeutic Advances in Neurological Disorders, 11, 1756286418770061. (Methodology: Literature review; Findings: Summary of current knowledge on end-of-life decisions in the treatment of patients with ALS).
Cohen, J., van Wesemael, Y., Smets, T., et al. (2011). Nationwide survey of decisions concerning life‐sustaining treatment in the end‐of‐life phase in ICUs in Belgium. Intensive Care Medicine, 37(10), 1623-1630. (Methodology: Nationwide survey of ICUs in Belgium; Findings: Examination of end-of-life decision-making practices, including withholding or withdrawing life-sustaining treatment).
Boer, T. A., & Seyfert, M. (2002). Voluntary Euthanasia Under Control? Further Empirical Evidence from The Netherlands. Journal of Medical Ethics, 28(5), 283-286. (Methodology: Analysis of empirical data on euthanasia practices in the Netherlands; Findings: Evaluation of compliance with legal requirements and oversight mechanisms).
Smith, K. A., Harvath, T. A., & Goy, E. R. (2006). Grief and Physician-Assisted Death: Ethical Considerations. Journal of Palliative Medicine, 9(6), 1361-1371. (Methodology: Literature review; Findings: Exploration of ethical considerations surrounding grief and physician-assisted death).
Gevers, S., van der Heide, A., de Vogel-Voogt, E., et al. (2016). Is a written advance euthanasia directive sufficient to guarantee a patient's autonomy? An analysis of The Dutch Euthanasia Act. Medicine, Health Care and Philosophy, 19(3), 439-447. (Methodology: Analysis of written advance euthanasia directives in the Netherlands; Findings: Examination of legal and ethical implications for patient autonomy).
Rodrigue, C., Brouckaert, B., & Leys, M. (2019). Characteristics and practical aspects of physician-assisted death requests in a Belgian tertiary care hospital: a review of 235 consecutive cases. BMJ Supportive & Palliative Care, 9(3), e25. (Methodology: Retrospective review of physician-assisted death requests in a Belgian hospital; Findings: Description of characteristics and practical aspects of cases).
Battin, M. P., & van der Heide, A. (2017). What European healthcare can learn from Oregon's Death with Dignity Act? BMJ, 359, j5379. (Methodology: Comparative analysis; Findings: Discussion of lessons learned from Oregon's Death with Dignity Act for European healthcare systems).
Rurup, M. L., Onwuteaka-Philipsen, B. D., van der Heide, A., et al. (2005). Physicians' Experiences with Dying Patients in Dutch Hospitals. Social Science & Medicine, 60(2), 273-282. (Methodology: Survey of physicians in Dutch hospitals; Findings: Exploration of experiences and attitudes towards end-of-life care, including euthanasia).
OBJECTIVES
To provide a comprehensive overview of the medical, ethical, and legal dimensions of euthanasia, allowing readers to develop a nuanced understanding of the topic.
To explore the latest research findings and scholarly perspectives on euthanasia, shedding light on its prevalence, patient experiences, healthcare provider attitudes, and societal implications.
To examine the ethical dilemmas inherent in euthanasia, including questions related to patient autonomy, beneficence, non-maleficence, and justice, fostering critical reflection on the moral principles at stake.
To analyze the evolution of legal frameworks governing euthanasia in different jurisdictions, identifying key criteria, procedural safeguards, and regulatory mechanisms designed to ensure ethical and lawful practices.
To facilitate informed dialogue and thoughtful discourse on euthanasia, encouraging readers to consider diverse viewpoints, engage with ethical complexities, and contribute to ongoing discussions surrounding end-of-life care and decision-making.
METHODOLOGY
Comprehensive Overview, and a thorough literature review of peer-reviewed articles, books, reports, and other scholarly sources spanning medical, ethical, and legal aspects of euthanasia.
Synthesize the findings to provide a holistic overview that addresses the complexities and nuances of euthanasia, incorporating insights from diverse perspectives.
Exploration of Research Findings by identifying empirical studies and surveys that investigate various aspects of euthanasia, including prevalence rates, patient preferences, healthcare provider attitudes, and societal attitudes.
Critically evaluate the quality and relevance of the research findings, considering factors such as sample size, methodology, and geographic location.
Present the research findings in a clear and accessible manner, highlighting key trends, disparities, and areas of consensus or controversy.
Examination of Ethical Dilemmas in ethical analysis and discourse, drawing upon established ethical frameworks such as principles, consequentialism, deontology, and virtue ethics.
Explore case studies and hypothetical scenarios to illustrate the complexities of ethical decision-making in the context of euthanasia.
Analysis of Legal Frameworks and review of legislation, regulations, and legal precedents about euthanasia in different jurisdictions, including countries where euthanasia is legal, illegal, or subject to specific regulations.
Compare and contrast legal frameworks, examining criteria for eligibility, procedural requirements, safeguards against abuse, and mechanisms for oversight and accountability.
References of the literature from videos of legal experts and analyses to gain insights into the interpretation and application of euthanasia laws in practice.
Synthesized Information from the video dialogues and discussion through interactive forums, seminars, workshops, or online platforms where stakeholders can share perspectives, exchange ideas, and engage in respectful debate.
Opinions expressed by diverse stakeholders, including healthcare professionals, ethicists, legal experts, policymakers, patients, families, and advocacy groups.
Summaries of key arguments, case studies, and policy briefs, to support informed decision-making and dialogue on euthanasia-related issues.
By employing the above comprehensive methodology, researchers and practitioners can effectively address the objectives related to euthanasia, contributing to a deeper understanding of the topic and facilitating constructive dialogue and decision-making.
UNDERSTANDING THE MEDICAL ETHICS
Medical ethics is a complex field that encompasses principles, values, and guidelines to guide healthcare professionals in making ethical decisions in patient care. The acceptance of euthanasia within medical ethics is a subject of ongoing debate and varies among different ethical frameworks, cultures, and individual healthcare providers.
Here are some perspectives on how euthanasia is approached within medical ethics:
Principle of Autonomy: Autonomy, or the right of individuals to make decisions about their own lives and bodies, is a fundamental principle in medical ethics. Proponents of euthanasia argue that respecting a patient's autonomy includes respecting their decision to end their life if they are experiencing unbearable suffering or have a terminal illness with no hope of recovery. From this perspective, euthanasia can be seen as an extension of patient autonomy and self-determination.
Principle of Beneficence: The principle of beneficence emphasizes the obligation of healthcare professionals to act in the best interests of their patients and to alleviate suffering. In cases where a patient is experiencing extreme pain or distress with no prospect of relief, proponents of euthanasia argue that ending the patient's life may be the most compassionate and humane course of action to fulfil the principle of beneficence.
Principle of Non-Maleficence: The principle of non-maleficence, or "not harm," cautions against actions that may cause harm or suffering to patients. In the context of euthanasia, opponents argue that intentionally ending a patient's life contradicts the principle of non-maleficence by directly causing harm. They argue that healthcare professionals must provide palliative care and alleviate suffering through means other than euthanasia.
Legal and Regulatory Considerations: In jurisdictions where euthanasia is legalized, healthcare professionals may face legal and regulatory requirements to adhere to specific guidelines and protocols when considering euthanasia requests. These regulations often include requirements for patient competency, informed consent, multiple medical assessments, and documentation of the decision-making process. Healthcare professionals must navigate the tension between legal obligations, ethical principles, and personal beliefs when considering euthanasia requests.
Professional Codes of Ethics: Many medical associations and professional organizations have codes of ethics that provide guidance on ethical standards and conduct for healthcare professionals. These codes may address the issue of euthanasia and provide guidelines or prohibitions based on the organization's stance on the practice. Healthcare professionals are expected to adhere to these codes of ethics while navigating complex ethical dilemmas, including euthanasia.
Overall, the acceptance of euthanasia within medical ethics is a nuanced and contentious issue, with divergent perspectives and considerations. While some healthcare professionals may support euthanasia as a compassionate response to unbearable suffering and respect for patient autonomy, others may oppose it on ethical, religious, or moral grounds. Ethical debates surrounding euthanasia highlight the complexity of end-of-life care and the need for thoughtful consideration of the principles, values, and responsibilities involved in patient care.
SOCIO-PSYCHOLOGICAL OUTLOOK AND ATTITUDES TOWARDS THE EXISTING PRACTICES OF EUTHANASIA
Certainly, here are a few more examples from history that illustrate attitudes and practices related to euthanasia-like concepts:
Ancient Egypt: Ancient Egyptian culture held a belief in an afterlife, where the soul continued its journey after death. Death was viewed as a transition to another realm, and there is evidence that euthanasia-like practices were employed to facilitate a smooth passage into the afterlife. For example, the "Opening of the Mouth" ceremony was performed on the deceased to ensure their well-being in the afterlife, and in some cases, it may have included hastening death to end suffering or preserve dignity.
Samurai Culture in Japan: In feudal Japan, the samurai code of honor, known as Bushido, included principles of loyalty, bravery, and honor in life and death. Samurai warriors who faced terminal illness, severe injury, or loss of honor sometimes chose to perform "seppuku" or ritual suicide rather than endure shame or suffering. While seppuku was not strictly euthanasia, it reflects a cultural acceptance of death as a means of preserving dignity and honor.
Hinduism and Buddhism: In Hindu and Buddhist traditions, the concept of "ahimsa" or non-violence is central to ethical principles. While both traditions generally uphold the sanctity of life, there are philosophical discussions about the permissibility of ending life in cases of extreme suffering or incurable illness. In certain texts and commentaries, there are references to the idea of "Prayopavesa" or fasting unto death as a means of achieving liberation from suffering.
Medieval Europe: In medieval Europe, attitudes towards death and suffering were heavily influenced by Christian theology and teachings. The Catholic Church exerted significant influence over moral and legal matters, reinforcing the sanctity of life doctrine and prohibiting practices that intentionally hastened death. However, there were instances where religious orders provided support for individuals seeking to end their lives, particularly in cases of severe illness or suffering, through acts of mercy or the provision of poison.
Traditional Indigenous Cultures: Various indigenous cultures around the world have had their customs and beliefs surrounding death and dying. In some indigenous societies, elders or individuals facing terminal illness might be afforded the option to end their lives through natural means or with the assistance of their community. These practices reflect cultural understandings of death as a natural part of life and the importance of maintaining dignity and autonomy in the face of suffering.
EUTHANASIA IN INDIA: UNDERSTANDING, ACCEPTANCE AND APPLICATION IN INDIA MEDICAL SYSTEM
In India, the understanding, acceptance, and application of euthanasia within the medical system are influenced by a combination of cultural, religious, legal, and ethical factors. Here's an overview of the situation in India:
Legal Status: Euthanasia, also known as "mercy killing" or "physician-assisted death," is not legal in India. However, there have been significant legal and ethical debates surrounding the issue. The Supreme Court of India has addressed the concept of euthanasia in several landmark cases, including the Aruna Shanbaug case in 2011 and the Common Cause case in 2018.
Passive Euthanasia: While active euthanasia (directly administering lethal substances to end a patient's life) remains illegal, the Supreme Court of India has recognized the concept of "passive euthanasia." In its judgment in the Common Cause case in 2018, the court ruled that passive euthanasia, which involves withdrawing or withholding life-sustaining treatment from terminally ill patients or those in a persistent vegetative state, can be permitted under certain circumstances. This decision provided legal clarity on end-of-life care decisions in India.
Cultural and Religious Perspectives: Cultural and religious beliefs play a significant role in shaping attitudes towards euthanasia in India. Hinduism, the predominant religion in India, generally emphasizes the sanctity of life and the concept of karma and rebirth. However, there are diverse interpretations within Hinduism, and some individuals and religious leaders may have varying views on end-of-life issues.
Medical Ethics and Professional Guidelines: The Medical Council of India, which sets standards for medical education and practice in the country, has provided guidelines on end-of-life care and ethical considerations for healthcare professionals. These guidelines emphasize the importance of respecting patient autonomy, providing compassionate care, and adhering to legal requirements when making decisions about end-of-life treatment and care.
Public Discourse and Advocacy: Euthanasia remains a topic of public discourse, ethical debate, and advocacy in India. Various organizations, medical professionals, and civil society groups have engaged in discussions about the need for legal reforms to address end-of-life care and the rights of patients to make decisions about their own lives and deaths. However, there are also voices opposing euthanasia on ethical, religious, and moral grounds.
These examples illustrate the diverse historical and cultural contexts in which attitudes towards euthanasia-like practices have emerged. While specific practices may vary, they all reflect human efforts to grapple with the ethical and moral complexities of death, suffering, and the value of life. Overall, the understanding, acceptance, and application of euthanasia within the Indian medical system are complex and evolving. While passive euthanasia has been recognized by the courts under certain conditions, active euthanasia remains illegal. The issue continues to spark debates about patient autonomy, medical ethics, religious beliefs, and legal reforms in India.
LEGAL AND REGULATED FORMS OF EUTHANASIA: REAL-LIFE EXAMPLES FROM ACROSS THE COUNTRIES IN THE WORLD
Euthanasia, especially in its legal and regulated forms, is a highly sensitive and private matter. As such, specific real-life examples may be limited in availability due to privacy concerns and ethical considerations. However, I can provide some general scenarios and cases from countries where euthanasia or assisted dying is legally permitted:
Netherlands: The Netherlands is one of the few countries where euthanasia is legalized under strict regulations. Dutch law permits euthanasia for competent adults who are experiencing unbearable suffering with no prospect of improvement. One example is the case of a woman named Aurelia Brouwers, who was granted euthanasia in 2018 due to her severe psychiatric conditions, including borderline personality disorder, depression, and psychosis.
Belgium: Belgium also allows euthanasia under specific conditions. In 2015, twin brothers Marc and Eddy Verbessem, who were born deaf and feared going blind, were euthanized after discovering they would also develop a genetic condition causing progressive vision loss. Their case raised ethical questions about euthanasia for non-terminal conditions.
Canada: Canada legalized medical assistance in dying (MAID) in 2016, allowing eligible patients to receive assistance in ending their lives under specific conditions. One well-known case is that of Audrey Parker, a woman with terminal cancer who chose to end her life with medical assistance in 2018. Parker advocated for changes to Canada's assisted dying laws, arguing that the requirement of a natural death being "reasonably foreseeable" was too restrictive.
Oregon, USA: Oregon was the first state in the United States to legalize physician-assisted dying through the Death with Dignity Act in 1997. One notable case is that of Brittany Maynard, a young woman with terminal brain cancer who moved to Oregon in 2014 to access medical aid in dying. Maynard's public advocacy for the right to die on one's terms brought national attention to the issue.
Switzerland: Switzerland has a long-standing tradition of allowing assisted suicide under certain conditions. Organizations like Dignitas and Exit International assist individuals who wish to end their lives. One example is the case of Marieke Vervoort, a Belgian Paralympic athlete who chose to end her life through euthanasia in Switzerland in 2019 due to her progressive degenerative condition and constant pain.
It's important to recognize that each of these cases involves complex medical, ethical, legal, and personal considerations. They illustrate the diversity of situations in which individuals may seek assistance in dying and the various legal frameworks and support systems in place in different countries.
METHODS USED FOR EUTHANASIA ACROSS THE WORLD
The specific methods used for euthanasia can vary depending on legal regulations, medical practices, and individual preferences. Listed below are the general overview of how euthanasia may be performed by medical practitioners in jurisdictions where it is legally permitted:
Patient Evaluation and Consent: Before proceeding with euthanasia, medical practitioners must conduct a thorough evaluation of the patient's medical condition, prognosis, and mental capacity. The patient must be deemed competent to make an informed decision about ending their life and must provide explicit, voluntary consent to undergo euthanasia.
Administration of Medication: In most cases, euthanasia involves the administration of a lethal dose of medication, typically by a healthcare provider. The medication is carefully selected to induce unconsciousness followed by respiratory and cardiac arrest, resulting in a peaceful and painless death.
Preparation and Monitoring: Before administering the medication, the medical team will prepare the necessary equipment and medications by established protocols. The patient may be provided with the opportunity to say goodbye to loved ones and make any final arrangements. Throughout the process, the medical team will closely monitor the patient's vital signs and provide emotional support as needed.
Administration of Anesthetic: The first step in the euthanasia process often involves administering a powerful anesthetic or sedative to induce unconsciousness. This ensures that the patient remains unaware and does not experience any discomfort during the subsequent steps of the procedure.
Administration of Lethal Medication: Once the patient is unconscious, the healthcare provider will administer the lethal medication, typically in the form of an intravenous injection. This medication acts quickly to stop the heart and respiratory function, leading to death within minutes.
Confirmation of Death: After the administration of the lethal medication, the medical team will confirm the patient's death through standard medical procedures, such as checking for vital signs and performing any necessary examinations. The patient's death is then documented following legal and medical requirements.
It's important to note that euthanasia is a highly regulated and carefully controlled procedure in jurisdictions where it is legal. Healthcare providers involved in euthanasia must adhere to strict guidelines and protocols to ensure that the procedure is carried out ethically, safely, and with the utmost respect for patient autonomy and dignity. Additionally, patients may have the option to undergo euthanasia at home or in a healthcare facility, depending on their preferences and medical needs.
PATIENT PREPARATION OF THE PATIENT, THE MODALITIES INVOLVED, AND THE ACTUAL PROCESS OF EUTHANASIA
Patient Preparation
Counselling and Support: Before undergoing euthanasia, patients often receive extensive counselling and support from healthcare professionals, including physicians, nurses, social workers, and psychologists. This support aims to ensure that patients fully understand their medical condition, prognosis, and treatment options, including the option of euthanasia. It also provides an opportunity for patients to express their wishes, concerns, and emotions in a supportive environment.
Informed Consent: In jurisdictions where euthanasia is legal, patients must provide informed consent to undergo the procedure. This involves receiving detailed information about the risks, benefits, and alternatives to euthanasia, as well as the legal and ethical implications. Patients may also be required to confirm their consent multiple times to ensure that it is voluntary and well-informed.
Advance Directives: Some patients may have previously expressed their wishes regarding end-of-life care through advance directives or living wills. These documents guide healthcare providers and family members about the patient's preferences for medical treatment, including the option of euthanasia, if they become incapacitated and unable to communicate their wishes.
MODALITIES INVOLVED
Administration Route: Euthanasia is typically administered through intravenous injection, allowing for rapid and precise delivery of the lethal medication. In some cases, alternative administration routes may be used, such as oral ingestion or intramuscular injection, depending on patient preferences and medical considerations.
Medications Used: The medications used for euthanasia typically include a combination of drugs designed to induce unconsciousness, paralysis, and cardiac arrest. Commonly used medications may include barbiturates, opioids, muscle relaxants, and potassium chloride. These medications are carefully selected and dosed to ensure a peaceful and painless death while minimizing the risk of complications.
Monitoring and Support: Throughout the euthanasia process, healthcare providers closely monitor the patient's vital signs, including heart rate, blood pressure, respiratory rate, and oxygen saturation. Supportive measures, such as supplemental oxygen, intravenous fluids, and medication for symptom management, may be provided as needed to ensure the patient's comfort and well-being.
ACTUAL PROCESS
Final Preparations: Before initiating euthanasia, the medical team prepares the necessary equipment, medications, and documentation by established protocols. The patient may have the opportunity to spend time with loved ones, say goodbye, and make any final arrangements.
Administration of Medications: Once the patient is fully prepared and has provided consent, the healthcare provider administers the lethal medication according to the predetermined plan. This typically involves a series of steps, starting with the induction of unconsciousness followed by the administration of medications to stop the heart and respiratory function.
Confirmation of Death: After the administration of the lethal medication, the medical team carefully monitors the patient's vital signs and clinical status to confirm that death has occurred. This may involve assessing for the absence of heartbeat, pulse, and respiratory effort, as well as performing any necessary examinations or tests to verify death.
It's important to emphasize that euthanasia is a highly regulated and carefully controlled procedure, with strict guidelines and protocols in place to ensure that it is carried out ethically, safely, and with the utmost respect for patient autonomy and dignity. The process involves extensive preparation, counselling, and support for both patients and their families, as well as close monitoring and oversight by healthcare professionals throughout the procedure.
THE LEGAL FACTORS VARIATIONS ACCORDING TO THE CULTURE OF DIFFERENT COUNTRIES
The legal aspects related to euthanasia vary significantly depending on the jurisdiction, as laws and regulations surrounding euthanasia differ from country to country and even within regions of the same country. However, there are several common legal considerations and important factors to be learned about euthanasia:
Legalization and Regulation: In jurisdictions where euthanasia is legal, there are typically specific laws and regulations governing the practice. These laws outline the eligibility criteria, procedural requirements, and safeguards that must be followed when considering and carrying out euthanasia. Legalization often involves stringent protocols to ensure that euthanasia is only performed in cases where it is deemed appropriate and justified.
Patient Autonomy and Consent: One of the central legal principles underpinning euthanasia is patient autonomy, which refers to the right of individuals to make decisions about their bodies and lives. In jurisdictions where euthanasia is legal, patients must provide informed consent to undergo the procedure, demonstrating that their decision is voluntary, well-informed, and free from coercion or undue influence. Legal frameworks often require multiple assessments and confirmations of consent to safeguard against potential abuses.
Medical Professional Obligations: Healthcare providers involved in euthanasia must adhere to legal and ethical obligations outlined in professional codes of conduct and regulatory guidelines. This includes ensuring that patients meet the eligibility criteria for euthanasia, providing comprehensive counselling and support, obtaining informed consent, and following established protocols for administering euthanasia medications. Healthcare providers must also document their actions and decision-making processes per legal requirements.
Legal Protections and Immunities: Legal frameworks surrounding euthanasia may include provisions to protect healthcare providers from civil and criminal liability when performing euthanasia in compliance with applicable laws and regulations. These legal protections aim to facilitate access to euthanasia for eligible patients while providing reassurance to healthcare professionals who may be involved in the process.
End-of-Life Care Alternatives: Legalizing euthanasia does not diminish the importance of palliative care, hospice services, and other forms of end-of-life care. Legal frameworks often emphasize the importance of providing comprehensive and compassionate care to patients at the end of life, including options for pain management, symptom control, and emotional support. Euthanasia should be viewed as one option among many for individuals facing terminal illness or unbearable suffering, with a focus on respecting patient autonomy and dignity.
In real-life situations, understanding the legal aspects related to euthanasia is essential for healthcare professionals, patients, families, policymakers, and society as a whole. Some important factors to be learned include:
Understanding the ethical principles and values underlying euthanasia, including considerations of autonomy, beneficence, non-maleficence, and justice.
Recognizing the complexities and nuances of end-of-life decision-making, including the need to balance patient autonomy with protection from harm and exploitation.
Appreciating the cultural, religious, and societal factors that shape attitudes towards euthanasia and end-of-life care in different communities and regions.
Being aware of the legal frameworks, regulations, and procedural requirements governing euthanasia in specific jurisdictions, including eligibility criteria, consent processes, and documentation standards.
Developing communication skills and ethical reasoning abilities to engage in respectful and empathetic discussions about end-of-life issues with patients, families, and colleagues.
In real-life situations, the legal aspects related to euthanasia have significant implications for healthcare delivery, patient care, and public policy. Healthcare professionals must navigate complex legal and ethical considerations when considering and discussing euthanasia with patients and families, ensuring that decisions are made by applicable laws, regulations, and professional standards. Additionally, ongoing dialogue and advocacy efforts are needed to promote awareness, understanding, and responsible implementation of euthanasia laws in a manner that upholds patient rights, safeguards against potential abuses, and respects diverse cultural and ethical perspectives.
THE LEGALITIES OF EUTHANASIA IN VARIOUS COUNTRIES
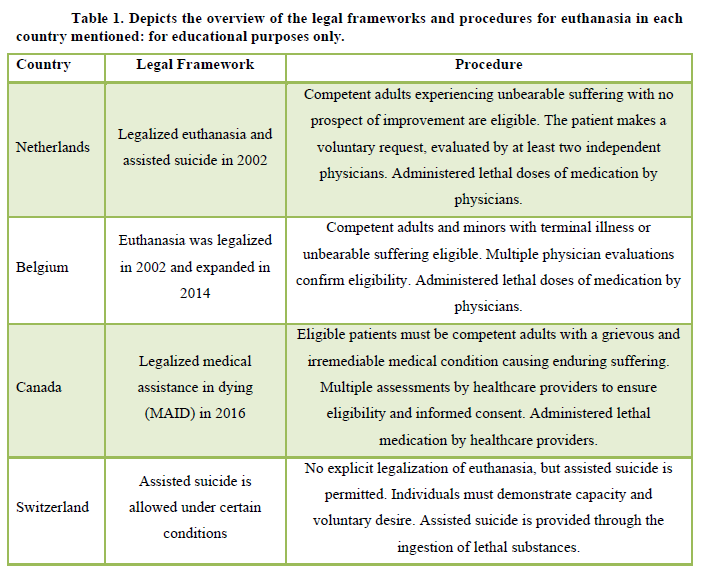
The legal aspects surrounding euthanasia vary significantly from country to country, with different jurisdictions adopting distinct approaches based on cultural, ethical, and legal considerations. Below, I'll describe the legal frameworks and procedures followed in various countries where euthanasia or assisted dying is permitted, along with key aspects of their legal systems:
Netherlands: Legal Framework: The Netherlands legalized euthanasia and assisted suicide in 2002 under the Termination of Life on Request and Assisted Suicide (Review Procedures) Act. The law permits euthanasia for competent adults experiencing unbearable suffering with no prospect of improvement, subject to strict eligibility criteria and procedural safeguards.
Procedure: In the Netherlands, euthanasia is carried out through a carefully regulated process involving multiple consultations and assessments. Patients must make a voluntary, well-considered request for euthanasia, which is evaluated by at least two independent physicians. The request must meet specific criteria, including unbearable suffering, lack of alternative options, and informed consent. If the criteria are met, physicians administer a lethal dose of medication to induce death, typically through intravenous injection.
Belgium
Legal Framework: Belgium legalized euthanasia in 2002, allowing competent adults to request euthanasia under certain conditions. The law was later expanded to include minors with terminal illnesses or unbearable suffering. Euthanasia in Belgium is governed by the Euthanasia Act, which establishes eligibility criteria, procedural requirements, and oversight mechanisms.
Procedure: Similar to the Netherlands, euthanasia in Belgium involves a rigorous process of evaluation and assessment. Patients must be evaluated by multiple physicians to confirm their eligibility for euthanasia, including the presence of unbearable suffering, terminal illness, and informed consent. Physicians administer a lethal dose of medication to induce death, adhering to established protocols and guidelines.
Canada
Legal Framework: Canada legalized medical assistance in dying (MAID) in 2016 through the passing of Bill C-14. MAID allows eligible patients to receive assistance in ending their lives under specific conditions, including being competent adults with grievous and irremediable medical conditions causing enduring suffering.
Procedure: In Canada, MAID is governed by strict eligibility criteria and procedural requirements outlined in federal legislation and provincial regulations. Patients must make a voluntary request for MAID, which is assessed by multiple healthcare providers to ensure eligibility and informed consent. If approved, healthcare providers administer a lethal medication to induce death, following established protocols and safeguards.
Switzerland
Legal Framework: Switzerland allows assisted suicide under certain conditions, but euthanasia is not explicitly legalized. Assisted suicide organizations, such as Dignitas and Exit International, assist individuals who wish to end their lives. Swiss law does not criminalize assisted suicide when performed by non-profit organizations or individuals acting out of compassion.
Procedure: In Switzerland, individuals seeking assisted suicide must demonstrate that they are of sound mind and have a rational and voluntary desire to end their lives. They must undergo thorough assessments by physicians and mental health professionals to ensure capacity and informed consent. Assistance in suicide is typically provided through the ingestion of a lethal substance, which the individual administers.
IMPORTANT LEGAL ASPECTS AND DEVELOPMENTS
In countries where euthanasia is legal, procedural safeguards and oversight mechanisms are in place to ensure that the practice is carried out by legal requirements and ethical principles.
Legal frameworks often include criteria for eligibility, procedural requirements for assessment and documentation, and mechanisms for review and oversight by regulatory authorities or ethics committees.
Public awareness, debate, and advocacy efforts continue to shape legal developments and policy reforms related to euthanasia, with ongoing discussions about expanding or refining existing laws to address emerging issues and concerns.
Legal systems play a crucial role in balancing competing interests and values, such as individual autonomy, protection of vulnerable populations, healthcare provider obligations, and societal attitudes towards death and dying.
Overall, the legal aspects surrounding euthanasia are complex and multifaceted, reflecting diverse cultural, ethical, and legal considerations. While euthanasia laws and procedures vary between countries, common themes include stringent eligibility criteria, procedural safeguards, and oversight mechanisms to ensure that euthanasia is carried out ethically, responsibly, and with patient rights and dignity (Table 1).
Psychological Impact: The impact of euthanasia on the psyche of the dependents of individuals who choose euthanasia can vary widely depending on factors such as cultural norms, familial dynamics, and the circumstances surrounding the decision. While some family members may find peace and acceptance in the choice of euthanasia, others may experience complex emotions such as grief, guilt, and conflict.
Here are examples from various countries to illustrate the diverse psychological impacts:
Netherlands: Example: In the Netherlands, where euthanasia is legal, family members may experience a range of emotions when a loved one chooses euthanasia. Some may support the decision as a compassionate choice to end suffering, while others may struggle with feelings of loss, guilt, or conflict about the decision. For example, a family member may feel guilty for not being able to alleviate the loved one's suffering or for questioning the decision to end their life.
Belgium: Example: Similarly, in Belgium, where euthanasia is also legal, family members may have mixed reactions to the decision. While some may find comfort in knowing that their loved one's suffering has ended, others may experience feelings of sadness, regret, or anger. For instance, a family member may struggle with feelings of abandonment or betrayal, wondering if they could have done more to support the loved one or prevent their decision to end their life.
Canada: Example: In Canada, where medical assistance in dying (MAID) is legal, family members may grapple with the emotional impact of the decision. While some may appreciate the opportunity to say goodbye and honor the loved one's wishes, others may experience feelings of grief, uncertainty, or moral conflict. For example, a family member may struggle with feelings of guilt or regret, questioning whether they did enough to support the loved one or if they could have influenced their decision differently.
Switzerland: In Switzerland, where assisted suicide is permitted under certain conditions, family members may face unique challenges in coping with the decision. While some may view assisted suicide as a dignified choice that respects the individual's autonomy, others may struggle with feelings of loss, stigma, or moral ambiguity. For instance, a family member may feel isolated or judged by others for supporting the loved one's decision to end their life.
United States: Example: In states like Oregon and California, where physician-assisted dying is legal, family members may undergo a range of emotional responses to the decision. Some may find solace in knowing that their loved one had control over their end-of-life care, while others may experience feelings of sadness, regret, or ambivalence. For example, a family member may struggle with conflicting emotions, torn between respecting the loved one's autonomy and mourning their loss.
Overall, the psychological impact of euthanasia on dependents can be complex and multifaceted, influenced by factors such as cultural beliefs, personal values, and the nature of the relationship with the individual who chooses euthanasia. While some may find comfort or acceptance in the decision, others may experience significant emotional distress and struggle to come to terms with the loss. Providing support and counselling to family members affected by euthanasia is essential in addressing their psychological needs and facilitating healing and adjustment.
Evolving Medical Ethics:
The number of instances of euthanasia or assisted dying approved in various countries can vary significantly depending on factors such as legal regulations, cultural attitudes, and healthcare practices. Here's an overview of how medical ethics has evolved and accepted euthanasia in some countries where it is legal:
Netherlands: The Netherlands was one of the first countries to legalize euthanasia in 2002. Since then, the practice has become increasingly accepted within Dutch medical ethics and society. The Dutch experience with euthanasia has led to the development of strict guidelines and protocols to ensure that the practice is carried out ethically and according to patient rights. Statistics from the Netherlands show that the number of reported euthanasia cases has steadily increased over the years, with thousands of cases reported annually.
Belgium: Belgium legalized euthanasia in 2002 and expanded its legislation in 2014 to include minors under certain conditions. Euthanasia is generally accepted within Belgian medical ethics, with healthcare providers adhering to established protocols and guidelines when considering and performing euthanasia. Statistics from Belgium indicate that the number of reported euthanasia cases has also risen over time, although the overall incidence remains lower than in the Netherlands.
Canada: Canada legalized medical assistance in dying (MAID) in 2016, allowing eligible patients to receive assistance in ending their lives under specific conditions. The acceptance of MAID within Canadian medical ethics has evolved rapidly since legalization, with healthcare providers and institutions developing policies and procedures to ensure compliance with legal requirements and ethical standards. Statistics from Canada show that the number of MAID cases has increased steadily since legalization, with thousands of cases reported each year.
Switzerland: Switzerland allows assisted suicide under certain conditions but does not explicitly legalize euthanasia. The acceptance of assisted suicide within Swiss medical ethics is generally high, with organizations like Dignitas and Exit International assisting individuals who wish to end their lives. Statistics on assisted suicide cases in Switzerland are less readily available compared to euthanasia cases in other countries, but it is estimated that hundreds of cases occur annually.
The evolution and acceptance of euthanasia within medical ethics have been influenced by various factors, including changing societal attitudes towards death and dying, advancements in palliative care and end-of-life decision-making, and legal developments in favor of patient autonomy and rights. While euthanasia remains a contentious issue in many parts of the world, its acceptance within medical ethics reflects a growing recognition of the importance of respecting patient autonomy, dignity, and quality of life at the end of life.
- Battin, M. P., & van der Heide, A. (2016). Assisted Dying: The End of the Beginning. JAMA, 316, 493-494.
- Boer, T. A., & Seyfert, M. (2002). Voluntary Euthanasia Under Control Further Empirical Evidence from The Netherlands. Journal of Medical Ethics, 28, 283-286.
- Battin, M. P., & van der Heide, A. (2017). What European healthcare can learn from Oregon's Death with Dignity Act. BMJ, 359, j5379.
- Bascom, P. B., & Tolle, S. W. (2002). Responding to requests for physician-assisted suicide. Annals of Internal Medicine, 136, 408-414.
- Battin, M. P. (2008). Physician-assisted suicide and euthanasia can you even say them? Perspectives in Biology and Medicine, 51, 466-473.
- Bilsen, J., Cohen, J., Chambaere, K., & Pousset, G. (2014). Medical end-of-life practices under the euthanasia law in Belgium. New England Journal of Medicine, 370, 1873-1875.
- Beauchamp, T. L., & Davidson, S. (1979). The definition of euthanasia. Journal of Medicine and Philosophy, 4, 294-312.
- Battin, M. P., Rhodes, R., & Silvers, A. (2015). Physician Assisted Suicide Expanding the Debate Routledge.
- Cholbi, M. (2015). Euthanasia A Reference Handbook. ABC-CLIO.
- Chambaere, K., Bilsen, J., Cohen, J., et al. (2010). Physician-assisted deaths under the euthanasia law in Belgium: A population-based survey. Canadian Medical Association Journal, 182,895-901.
- Chambaere, K., Vander Stichele, R., Mortier, F. (2010). Recent Trends in Euthanasia and Other End-of-Life Practices in Belgium. New England Journal of Medicine, 362, 1813-1820.
- Cohen, J., van Wesemael, Y., Smets, T. (2011). Nationwide survey of decisions concerning life‐sustaining treatment in the end‐of‐life phase in ICUs in Belgium. Intensive Care Medicine, 37, 1623-1630.
- Coors, M. E. (2007). Euthanasia and palliative care. The Journal of Medicine and Philosophy, 32, 79-92.
- Chochinov, H. M., Hack, T., McClement, S. (2002). Euthanasia and Assisted Suicide: A Physician's and Nurse's Perspective. Journal of Palliative Care, 18, 105-110.
- Dyer, C. (2019). Assisted dying Australian state Victoria passes legislation. BMJ, 367, l6815.
- Dees, M. K., Vernooij-Dassen, M. J., Dekkers, W. J. (2011). Perspectives on euthanasia and assisted suicide among Dutch general practitioners and nurses in home care a qualitative study. Health & Social Care in the Community, 19, 58-68.
- Dordrecht, R. F., Rietjens, J. A., van der Heide, A. (2017). The impact of physician-assisted suicide and euthanasia on family members: A nation-wide study in The Netherlands. Health Policy, 121, 1205-1211.
- de Lange, M., & Kuyper, H. (2009). Practical implications of ethical theories for end-of-life decisions and palliative care. Nursing Ethics, 16, 303-318.
- Emanuel, E. J., Daniels, E. R., & Fairclough, D. L. (1996). Euthanasia and Physician-Assisted Suicide: Attitudes and Experiences of Oncology Patients Oncologists and the Public. JAMA, 276, 1739-1744.
- Emanuel, L. L., & Emanuel, E. J. (1998). The promise of a good death. The Lancet, 351, 9114.
- Emanuel, E. J., & Onwuteaka-Philipsen, B. D. (2017). The Netherlands' Experience with Euthanasia: Implications for Policy in the United States. JAMA Internal Medicine, 177, 1393-1394.
- Frerichs, I. W., Rietjens, J. A., Van Delden, J. J. (2016). Terminal sedation and euthanasia a comparison of clinical practices. European Journal of Palliative Care, 23, 239-243.
- Ganzini, L., Johnston, W. S., & McFarland, B. H. (2000). Attitudes of Patients with Amyotrophic Lateral Sclerosis and Their Caregivers Toward Assisted Suicide. New England Journal of Medicine, 342, 1049-1052.
- Georges, J. J., & Onwuteaka-Philipsen, B. D. (2015). When Doctors and Family Members Disagree. Hastings Center Report, 45, 10-11.
- Green, J. (1995). Euthanasia and Religion. Journal of Palliative Care, 11, 10-13.
- Gorsuch, N. M. (2000). The Right to Assisted Suicide and Euthanasia. Harvard Journal of Law & Public Policy, 23, 599-610.
- Gevers, S., van der Heide, A., de Vogel-Voogt, E. (2016). Is a written advance euthanasia directive sufficient to guarantee a patient's autonomy? An analysis of The Dutch Euthanasia Act. Medicine, Health Care and Philosophy, 19, 439-447.
- Ganzini, L., Goy, E. R., Dobscha, S. K., et al. (2008). Mental Health Outcomes of Family Members of Oregonians Who Request Physician Aid in Dying. Journal of Pain and Symptom Management, 36, 441-449.
- Griffiths, J., Weyers, H., & Adams, M. (2008). Euthanasia and Law in Europe. Hart Publishing.
- Hendin, H. (2002). Seduced by Death: Doctors Patients and the Dutch Cure. WW Norton & Company.
- Hendin, H. (2008). The case against physician-assisted suicide and euthanasia. Issues in Law & Medicine, 24, 187-215.
- Hesselmann, G., & Kostev, K. (2018). End-of-life decisions in the treatment of patients with amyotrophic lateral sclerosis a review of current knowledge. Therapeutic Advances in Neurological Disorders, 11, 1756286418770061.
- Hagen, N. A., Biondo, P., Stiles, C. (2016). Euthanasia, assisted suicide, and requests for hastened death. Journal of Palliative Medicine, 19, 723-727.
- Harned, J. (2006). Legalizing euthanasia and assisted suicide: the illusion of safeguards and controls. Issues in Law & Medicine, 22, 247-265.
- Hendin, H., & Klerman, G. L. (2018). Physician-Assisted Suicide in Oregon: A Medical Perspective. Suicide & Life-Threatening Behavior, 48, 104-109.
- Keown, J. (2002). Euthanasia Ethics and Public Policy an Argument against Legalization. Cambridge University Press.
- Hendin, H., & Foley, K. (2008). Physician Assisted Suicide Expanding the Debate. Taylor & Francis.
- Kissane, D. W., & Kelly, B. J. (2000). Demoralization death and dying. Psycho-Oncology, 9, 101-106.
- Kesselheim, A. S., & Studdert, D. M. (2019). Should Physicians Help Patients Die JAMA, 322, 1563-1564.
- Logters, T. T., Klinkhammer-Schalke, M., Koller, M. (2016). Euthanasia: the role of the ICU and palliative care. Journal of Palliative Medicine, 19, 384-389.
- Lewens, T. (2013). Euthanasia Can't live with it can’t live without it. Studies in History and Philosophy of Science Part C: Studies in History and Philosophy of Biological and Biomedical Sciences, 44, 69-74.
- Meier, D. E. (2016). Will assisted suicide laws lead to rampant elder abuse? Not: A psychiatrist’s perspective. Journal of Palliative Medicine, 19, 787-789.
- McLeod, C. (2008). Euthanasia A Problem for Modern Law. Modern Law Review, 71, 936-962.
- Ogden, J. A., & Saran, A. (2009). Euthanasia A Reference Handbook. ABC-CLIO.
- Onwuteaka-Philipsen, B. D., Brinkman-Stoppelenburg, A., Penning, C., et al. (2012). Trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from a repeated cross-sectional survey. The Lancet, 380, 908-915.
- Ogden, J. A. (2001). Euthanasia A Reference Handbook. ABC-CLIO.
- Penney, L. (2015). Assisted Suicide and Euthanasia: A Natural Law Ethics Approach. Journal of Palliative Care, 31, 214-220.
- Quill, T. E., Lo, B., & Brock, D. W. (1997). Palliative options of last resort: a comparison of voluntarily stopping eating and drinking terminal sedation physician-assisted suicide, and voluntary active euthanasia. JAMA, 278, 2099-2104.
- Quill, T. E., & Greenlaw, J. (2008). A Case for Non-Aggressive Death. Hastings Center Report, 38, 16-19.
- Rietjens, J. A., van der Heide, A., Onwuteaka-Philipsen, B. D., et al. (2009). A comparison of attitudes towards end-of-life decisions: a survey among the Dutch general public and physicians. Social Science & Medicine, 68, 1915-1922.
- Rodrigue, C., Brouckaert, B., & Leys, M. (2019). Characteristics and practical aspects of physician-assisted death requests in a Belgian tertiary care hospital a review of 235 consecutive cases. BMJ Supportive & Palliative Care, 9, 25.
- Rurup, M. L., Onwuteaka-Philipsen, B. D., van der Heide, A. (2005). Physicians' Experiences with Dying Patients in Dutch Hospitals. Social Science & Medicine, 60, 273-282.
- Raphael, B., & Rodin, G. (1991). Partnerships in Care Medicine and Ministry. Journal of Palliative Care, 7, 23-27.
- Smets, T., Bilsen, J., Cohen, J. (2011). Reporting of Euthanasia in Medical Practice in Flanders, Belgium. JAMA, 305, 100-101.
- Smith, K. A., Harvath, T. A., & Goy, E. R. (2006). Grief and Physician-Assisted Death: Ethical Considerations. Journal of Palliative Medicine, 9, 1361-1371.
- Schadenberg, A. (2013). The impact of euthanasia and assisted suicide on people with disabilities and older people. Issues in Law & Medicine, 28, 11-31.
- Schur, E. M. (2002). Dutch Euthanasia: A Review. Journal of the American Medical Directors Association, 3, 34-40.
- Singer, P. (2016). Not for the Nihilist: Bioethics and the Secular. Journal of the American College of Surgeons, 223, 119-126.
- Somerville, M. A. (2011). Death Talk the Case Against Euthanasia and Physician Assisted Suicide. McGill-Queen's Press.
- Singer, P. (1994). Rethinking Life and Death the Collapse of Our Traditional Ethics. St. Martin's Griffin.
- Sulmasy, D. P. (2011). Legalizing Euthanasia or Assisted Suicide the Illusion of Safeguards and Controls. Current Oncology Reports, 13, 83-88.
- Thomasma, D. C. (2000). Euthanasia and Physician-Assisted Suicide: Killing or Caring. Journal of Palliative Care, 16, 2-3.
- Ten Have, H., & Welie, J. V. M. (2005). Death and Medical Power: An Ethical Analysis of Dutch Euthanasia Practice. Open University Press.
- van der Heide, A., Deliens, L., Faisst, K. (2003). End-of-life decision-making in six European countries: A descriptive study. The Lancet, 362, 345-350.
- van Delden, J. J., & van der Heide, A. (2010). Legal physician-assisted suicide in Oregon and the Netherlands: evidence concerning the impact on patients in vulnerable groups. Journal of Medical Ethics, 36, 457-464.
- van der Heide, A., Onwuteaka-Philipsen, B. D., Rurup, M. L., et al. (2007). End-of-Life Practices in the Netherlands under the Euthanasia Act. New England Journal of Medicine, 356, 1957-1965.
- van der Heide, A., Deliens, L., Faisst, K. (2007). End-of-life decision-making in Belgium, Denmark, Sweden and Switzerland: Does place of death make a difference. Journal of Epidemiology and Community Health, 61, 1062-1068.
- Werth, J. L., & Smith, K. A. (2002). The Practice of Euthanasia and Physician-Assisted Suicide in the United States: Adherence to Proposed Safeguards and Effects on Physicians. The Journal of Law, Medicine & Ethics, 30, 122-130.

