Case Report
Delayed Onset of Bilateral Anterior Uveitis Secondary to Erlotinib
1187
Views & Citations187
Likes & Shares
Anterior uveitis is a rare complication associated with erlotinib. We report a unique case of delayed onset bilateral acute anterior uveitis at 21 months after commencement of erlotinib and review previous case reports in the literature on erlotinib associated anterior uveitis. Our patient was treated with frequent topical corticosteroid and a cycloplegic agent with good response whilst continued on erlotinib. Physicians should be aware of this potential complication and an urgent ophthalmology review is warranted when patients on erlotinib present with blurry vision, ocular injection and pain. Topical corticosteroid therapy often produces good clinical outcome.
Keywords: Erlotinib, Anterior uveitis, Epidermal growth factor receptor (EGFR), Tyrosine kinase inhibitor, Non-small cell lung cancer
INTRODUCTION
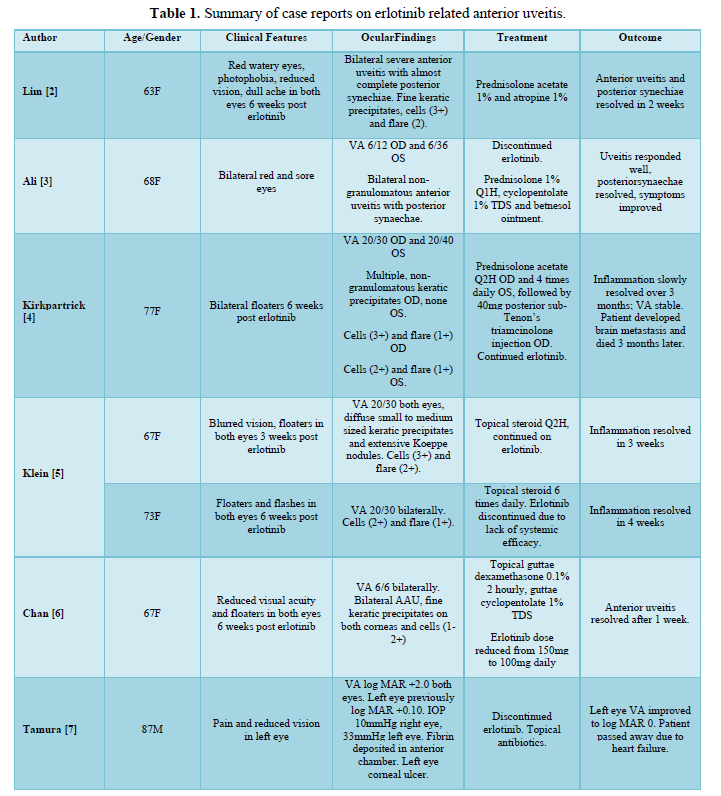
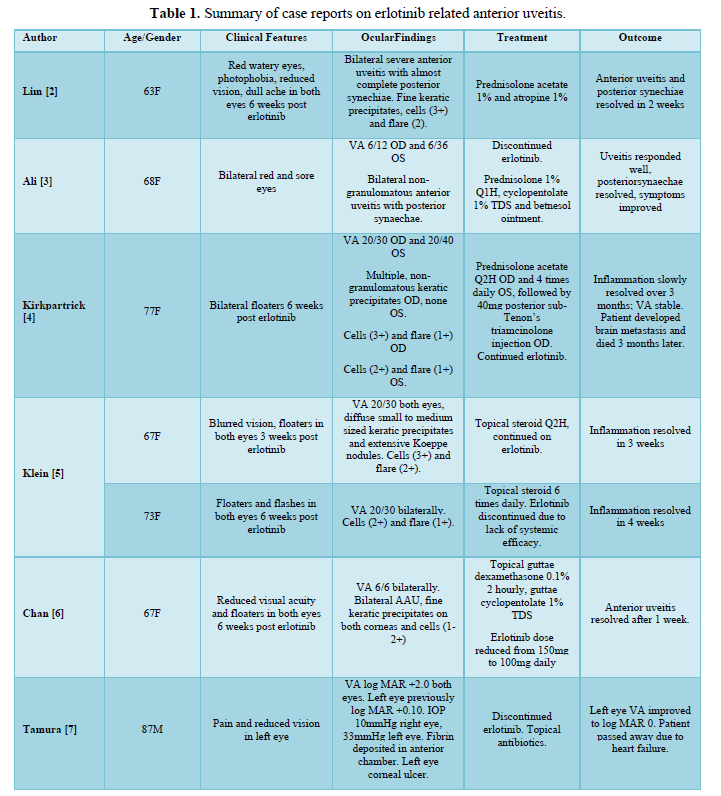
Erlotinib is an oral small molecule inhibitor of epidermal growth factor receptor (EGFR) tyrosine kinase. It is an approved therapy for advanced non-small cell lung cancer (NSCLCa) patients [1]. Common ocular adverse reactions with the use of erlotinib include conjunctivitis and keratoconjunctivitis sicca. Less common ocular adverse reactions include corneal perforation, corneal ulceration and episcleritis. Anterior uveitis is a rare complication associated with erlotinib that has been reported in only a few cases [2-7] (Table 1).
CASE HISTORY
We present a case of a 69-year-old Middle Eastern man with stage IV EGFR mutated lung adenocarcinoma with liver, nodal and paraspinal metastasis. He underwent left upper lobectomy followed by three cycles of adjuvant cisplatin and vincristine chemotherapy. His disease progressed requiring debulking of T10-12 paraspinal metastasis and radiotherapy 60Gy to the area. He was commenced on erlotinib standard dose 150 mg daily, which he tolerated well, with only a mild acneiform rash on his face managed with oral doxycycline. There was a complete response to erlotinib with no other detectable disease apart from a stable paravertebral mass on CT.
At 21 months post commencement of erlotinib therapy, he presented with a 5-day history of blurred vision, ocular injection and photosensitivity. There was no prior history of systemic inflammatory disease or uveitis. He had an unremarkable eye assessment 5 years prior. He has type 2 diabetes, dyslipidaemia, atrial fibrillation and asthma. His other regular medications include aspirin, metformin, rosuvastatin, sotalol and ventolin.
On ophthalmic examination his corrected visual acuity was 6/7.5 bilaterally and the intraocular pressure 12 mmHg in both eyes. There was bilateral anterior chamber inflammation (2+ cells) and flare (2+) (Standardization of Uveitis Nomenclature). The vitreous was quiet and there was no evidence of macular oedema or posterior segment involvement. The patient demonstrated palmo plantar erythron dysaesthesia from erlotinib. The patient did not have signs or symptoms of sarcoidosis or spondyloarthropathy.
Screening for infectious and inflammatory causes of bilateral anterior uveitis was unremarkable. In particular syphilis and Quanti FERON gold testing were negative. The HLA-B27 and ACE level were normal. The patient was diagnosed with bilateral anterior uveitis secondary to erlotinib. He was commenced on topical corticosteroid drops (prednisolone acetate) hourly and a cycloplegic agent (topical atropine). The anterior inflammation improved with topical steroid therapy alone and the patient’s vision remained stable. Erlotinib was continued throughout and hence not compromising his NSCLCa management.
DISCUSSION
Anterior uveitis is inflammation of the iris and/or anterior part of the ciliary body. Patients may present with pain, erythema and blurred vision. Uveitis is often idiopathic, however also frequently occurs in association with systemic conditions, such as infections and inflammatory diseases. Erlotinib associated anterior uveitis is rare with only 7 cases reported in the literature (Table 1). In most cases, patients presented with ocular symptoms within 6 weeks after commencing erlotinib. Our patient did not develop ocular symptoms until 21 months into erlotinib therapy. He also had papulopustular acneiform eruptions, which are typical cutaneous side effects of EGFR inhibitors such as erlotinib [8]. Initial treatment in the literature includes topical corticosteroid drops and a mydriatic agent. One case required posterior sub-Tenon’s triamcinolone injection [4]. In 3 cases erlotinib was discontinued [2,5,7]. In 1 case the dose of erlotinib was reduced [6]. All patients achieved resolution of uveitis with treatment.
Whilst a rare complication, there are increasing number of cases of erlotinib associated anterior uveitis with its growing use in cancer treatment. It is important for treating physicians and ophthalmologists to be aware of this complication and to educate their patients as to potential ocular side effects. An ophthalmology review is certainly required for all patients on erlotinib who have blurred vision, ocular pain and photophobia. Baseline ocular screening may also be considered in patients commencing erlotinib therapy, particularly those with co-existing systemic disease such as diabetes or inflammatory arthropathies.
CONCLUSION
We report a case of erlotinib associated delayed onset acute anterior uveitis. This is different to other reported cases where onset is usually within a few weeks of starting erlotinib. Similar to other cases, our patient responded well to topical corticosteroid treatment whilst being able to continue with erlotinib. We wish to highlight acute anterior uveitis as a potential complication with erlotinib use. Based on our review, clinical outcome is often favorable with treatment and in some cases with continuation of erlotinib therapy.
- Piperdi B, Soler RP (2012) Role of erlotinib in the treatment of non-small cell lung cancer: Clinical outcomes in wild-type epidermal growth factor receptor patients. Drugs72 Suppl 1(0 1):11-19.
- Lim LT, Blum RA, Cheng CP (2010) Bilateral anterior uveitis secondary to erlotinib. Eur J Clin Pharmacol 66: 1277-1278.
- Ali K, Kumar I, Saeed MU, Saeed MU (2011) Erlotinib-related bilateral anterior uveitis. BMJ Case Rep 2011: bcr0320113988.
- Kirkpatrick CA, Almeida DRP, Hornick AL, Chin EK, Boldt HC (2015) Erlotinib-associated bilateral anterior uveitis: Resolution with posterior sub-Tenon's triamcinolone without erlotinib cessation. Can J Ophthalmol 50(5): e66-e67.
- Klein KA, Azzoli CG, Rifkin LM (2017) Bilateral acute simultaneous onset anterior uveitis presumed secondary to erlotinib: A report of two cases. Am J Ophthalmol Case Rep 6: 21-23.
- Chan S, Ahern E, Chaudhry S, Hughes B (2019) Bilateral acute anterior uveitis: a rare ocular side effect of erlotinib. BMJ Case Rep 12(12): e232868.
- Tamura M, Takai Y, Nakamura S, Ohira A (2020) A case report of pseudo-exfoliation syndrome with prolonged corneal epithelial regeneration because of erlotinib-induced unilateral corneal ulcer and anterior uveitis. Acta Ophthalmol 98(8): e1055-e105.
- Preda VA, Mann S, Lee S (2008) Cutaneous complications of erlotinib in the treatment of non-small cell lung cancer: A report of three cases. Hong Kong J Dermatol Venereol 16: 133-141.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Journal of Renal Transplantation Science (ISSN:2640-0847)
- International Journal of Surgery and Invasive Procedures (ISSN:2640-0820)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- Journal of Spine Diseases
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- International Journal of AIDS (ISSN: 2644-3023)

