Research Article
To Assess the Efficacy of Modified Atosiban Regimen in Prevention of Preterm Labor in Third Trimester
1081
Views & Citations81
Likes & Shares
The aim of the study was to assess the efficacy of a modified regimen of the drug Atosiban in preventing preterm labor. It is a prospective study done in a tertiary care center with a sample size of 60 pregnant women in their 24 to 37 weeks of gestation with suspected risk of preterm delivery. A complete history and examination were done and subjects were included according to predetermined criteria to avoid confounding factors. The sample consisted of patients of different age, parity, socioeconomic status, previous preterm delivery and gestational age among other factors. The various groups were followed up till delivery to assess the efficacy of the drug in preventing preterm labor. The study showed the regimen to be effective in preventing preterm labor in 83.3% of patients out of 60 patients the labor was prolonged 72 h 1 week in 24 of the patients in 48-72 h in 16 patients.
Keywords: Atosiban efficacy, Preterm delivery, Oxytocin receptor, Preterm labor
Abbreviations: OT: Oxytocin; OTR: Oxytocin Receptor; NICU: Neonatal Intensive Care Unit; OPD: Outpatient Department; IPD: Inpatient Department; ECG: Electrocardiograph; ANC: Antenatal Care; USG: Ultrasonography; RDS: Respiratory Distress Syndrome
INTRODUCTION
Delivery before the completion of 37 weeks of gestation is defined as Preterm labor. Almost 5-13% of all pregnancies are affected by preterm labor in developed countries. Preterm labor is responsible for approximately 50% of neonatal morbidity and 50-75% of neonatal mortality worldwide being the most important cause for neonatal morbidity and mortality [1].
Early birth is the major cause of perinatal morbidity and mortality accounting for 85% of all early infant deaths, not secondary to a congenital abnormality [2]. A significant increase in the survival rates, particularly for the extremely premature baby (born between 24- and 27-weeks’ gestation) have been seen due to the advancement in perinatology and neonatology in the past decades, however, the associated morbidity remains significant, one-fifth to one-quarter preterm born babies suffer at least one of the major disabilities like chronic lung disease, impaired mental development, cerebral palsy, deafness, or blindness [3,4]. The other risk factors include preterm rupture of membranes, antepartum hemorrhage, history of previous preterm delivery and abortion, vaginal and urinary tract infection, etc. [5]. The exact mechanism of the onset of term and preterm labor is a complex process. Once a patient starts undergoing preterm labor, it is very difficult to control.
Changes in the levels of intracellular calcium led to myometrial contractility. Calmodulin and Myosin Light Chain Kinase is activated due to the increased intracellular calcium levels, which in turn triggers actin filaments and generates the contraction force [6-8]. Oxytocin (OT) is a hormone produced by the hypothalamus and secreted by the pituitary gland is responsible for myometrial contractions and plays a crucial role in childbirth - both term and preterm labor. OT binds to its receptor leading to G-protein coupling pathway which in turn increases the intracellular calcium levels that initiate the generation of contractions. Henceforth, oxytocin receptor (OTR) is common point of target for the development of tocolytics, the drugs which are known to prevent preterm labor. Tocolysis mainly aims at prolonging pregnancy for at least 48-72 h to provide adequate time for minimal effect of corticosteroids thus helping in preventing RDS in newborns, promoting consultation with pediatricians and facilitating the transfer of the neonate to NICU.
Atosiban, 1(3-mercaptopropionic acid)-2-(O-ethylD-thyroxine)-4-threonine-8-L-orthinin e-oxytocin, is a synthesized cyclic non-peptide that acts as a competitive antagonist for OTR. It works by inhibiting the dose-dependent OT-mediated rise in intracellular calcium levels which also involves the closing of voltage-gated channels that prevent the entry of calcium into the cell [9].
Hence the present study was done at our tertiary care center to assess the efficacy of modified Atosiban regimen in the prevention of preterm labor in the 3rd trimester.
MATERIAL AND METHODS
Study Design: A hospital-based prospective study was conducted with 60 patients.
Study Duration: For 18 months.
Study Area: The study was done at our tertiary care center in the department of Obstetrics & Gynecology, at Dr. D.Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune on attending OPD/IPD.
Study Population: All Pregnant female subjects in their 24th week to 37th week of pregnancy with the suspected risk of preterm labor. attending OPD/IPD of Tertiary care hospital that fulfilled the inclusion criteria.
Sample Size: 60 patients
Inclusion Criteria:
- Willing and able to provide written informed consent.
- Pregnant female weeks 24 to 37 weeks
- Screening ECG without clinically significant abnormalities.
- All ANC patients with history, clinical, & USG findings suggestive of preterm labor.
- Multigravida with the previous history of preterm delivery
Exclusion Criteria:
- Twin pregnancy
- Premature rupture of membranes
- Antepartum hemorrhage
- Fetal growth restriction
- Gross congenital anomalies
- Rh incompatibility
- With known medical disorders (Chronic Hypertension, Diabetes mellitus, heart disease) which may need preterm delivery.
- History of cervical encirclage.
After validation from the Institutional Ethics Committee, and informed consent was taken after an explanation of the purpose of the study from each participant.
After the patients were enrolled for the study, a thorough history and physical examination were done as per proforma. Informed consent was taken from Pregnant female subjects in their 24th week to 37th week of pregnancy with increased risk of preterm labor were chosen after a detailed history and clinical examination. Atosiban was administered after the evaluation of the patient, according to the drug characteristic medical protocol. The initial dose of Atosiban included a single intravenous bolus dose (6.75 mg in 0.9 mL isotonic sodium chloride solution), which was immediately followed by an intravenous infusion of 300 μg/min of Atosiban in 5% glucose for 3 h and then 100 μg/min for up to 48 h.
The treatment duration was 13 weeks maximum depending on the gestational age at enrolment. Safety and efficacy follow-up visit: Depending upon the period of gestation i.e., at 24th week, 28th week, 32nd week, 34th week, 36th week as per expected delivery.
Efficacy and Safety Parameters were assessed and recorded at baseline and each visit till pregnancy. Adverse events were assessed at all visits.
Qualitative data was presented with the help of a frequency and percentage table. Association among the study groups is assessed with the help of Fisher’s test, Student ‘t’ test and Chi square test. ‘p’ value less than 0.05 is taken significant.
The Chi square statistic was used for testing relationships on categorical variables. Student t-test was used to compare the means of a normally distributed interval dependent variable for two independent groups. The Fisher’s exact test was used when we wanted to conduct a Chi-square test, but one or more of the cells had an expected frequency of five or less.
RESULTS (TABLES 1-6)
DISCUSSION
A hospital-based prospective study was conducted with a total of 30 patients to assess the efficacy of a modified Atosiban regimen for the prevention of preterm labor in the 3rd trimester.
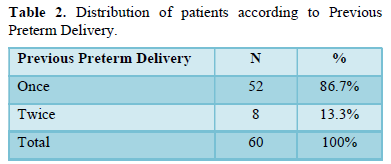
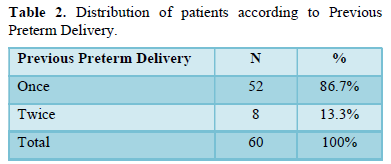
It was observed in the present study that 52 (86.7%) patients had one previous preterm delivery while 8 (13.3%) patients had two previous preterm deliveries respectively.
A previous preterm birth before 34 weeks of gestation is considered a major risk factor for the subsequent preterm birth with a relative risk of 13.56 [14].
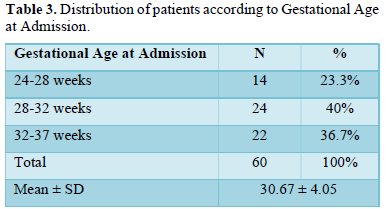
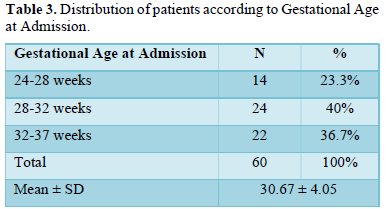
It was observed in our study that 14 (23.3%) patients presented among gestational age of 24-28 weeks while 24 (40%) and 22 (36.7%) patients presented among gestational age of 28-32 weeks and 32-37 weeks respectively. The mean gestational age of patients was 30.67 ± 4.05 weeks.
Yu [12] study found no significant difference between atosiban groups and conventional treatment groups in the low gestational ages. However, for the high gestational ages, Atosiban treatment group showed higher efficacy (84%; n ¼ 21/25 vs. 37.5%; n ¼ 3/8).
Yu [12] observed that for the high gestational ages, Atosiban treatment group showed higher efficacy (84%; n ¼ 21/25 vs. 37.5%; n ¼ 3/8).
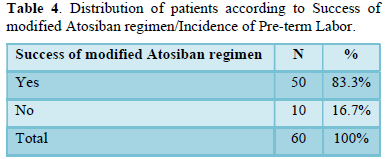
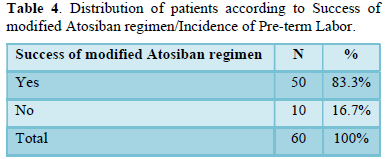
In our study, the success of modified Atosiban regimen in the prevention of preterm labor was 83.3%. The incidence of pre-term labor was 16.7%. Cabrol [10], Grzesiak [13] and Guillermo [15] noted similar observations in their studies.
Grzesiak [13] study observed patients that gave birth at 36.6 weeks of pregnancy on average which might suggest preterm birth, most of the pregnant women (35/53, 66%) had labored after 37 completed weeks of pregnancy confirming the tocolytic effectiveness of Atosiban.
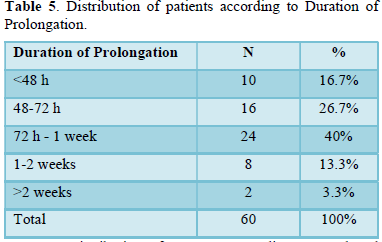
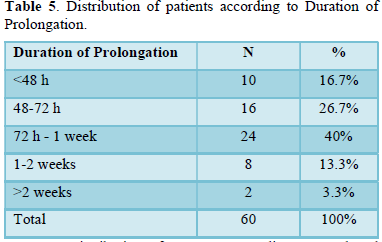
It was observed in this study that the duration of prolongation in 10 (16.7%) patients were2 weeks respectively. This is concordant to the studies of Yu [12], Ashraf [11], Grzesiak [13] and Tsatsaris [16].
Yu [12] study comparing the efficacy of atosiban with conventional treatment of the threatened preterm labor observed proportion of women not requiring an alternative tocolytic treatment within 48 h and remaining undelivered was significantly higher in Atosiban treatment group (89.3%; n ¼ 25/28) compared with conventional treatment (24.2%; n ¼ 8/ 33).
Ashraf [11] randomized controlled trial comparing the efficacy and safety of atosiban with nifedipine for PTL treatment found no significant difference between atosiban and nifedipine for pregnancy prolongation of 48 h or more regarding efficacy or effectiveness. Pregnancy prolongation for 7 days or more also did not differ between groups for efficacy or effectiveness.
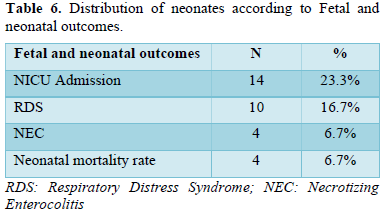
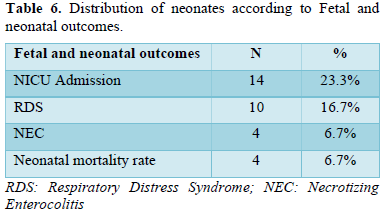
In our study, 14 (23.3%) neonates were admitted to NICU while 10 (16.7%) and 4 (6.7%) neonates had respiratory distress syndrome (RDS) and necrotizing enterocolitis respectively. There were 4 (6.7%) neonatal deaths in our study. Similar observations were noted in the studies of Yu [12], Tsatsaris [16] and Grzesiak [13].
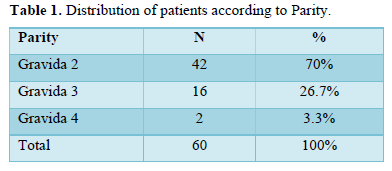
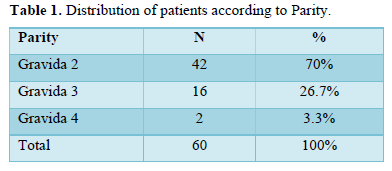
- 42 (70%) patients were gravida 2 while 16 (26.7%) were gravida 2 and (3.3%) were gravida 4 respectively.
- 52 (86.7%) patients had one previous preterm delivery while 8 (13.3%) patients had two previous preterm deliveries.
- 14 (23.3%) patients presented with the gestational age of 24-28 weeks while 24 (40%) with gestational age 28-32 weeks and 22 (36.7%) patients presented with gestational age of 32-37 weeks. The mean gestational age of patients was 30.67 ± 4.05 weeks.
- The success of the modified Atosiban regimen in the prevention of preterm labor was 83.3% and incidence of pre-term labor was 16.7%.
- The duration of prolongation in 10 (16.7%) patients was 2 weeks respectively.
- 14 (23.3%) neonates were admitted to NICU while 10 (16.7%) and 4 (6.7%) neonates had respiratory distress syndrome (RDS) and necrotizing enterocolitis respectively. There were 4 (6.7%) neonatal deaths in our study.
CONCLUSION
Predicting precisely and then preventing preterm labor and birth still remains a pivotal challenge faced by modern obstetrics. Identifying women with greater chances of preterm birth will allow the tailoring of medical interventions as well as targeted therapeutic treatments that aim at improving maternal and fetal outcomes.
Oxytocin antagonist atosiban was found to be better tolerated by both mother and fetus, with a comparable neonatal and infant safety profile, and atosiban was effective in delaying threatened preterm birth.
- Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C (2010) Global report on preterm birth and stillbirth (1 of 7): Definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth 10: S1.
- Norwitz ER, Robinson JN (2001) A systematic approach to the management of preterm labor. Semin Perinatol 25: 223-235.
- Chandiramani M, Tribe RM, Shennan AH (2007) Preterm labor and prematurity. Obstet Gynaecol Reprod Med 17: 232-237.
- Johnson S, Fawke J, Hennessy E, Rowell V, Thomas S, et al. (2009) Neurodevelopmental disability through 11 years of age in children born before 26 weeks of gestation. Pediatrics 124: e249-e257.
- Singh U, Singh N, Seth S (2007) A prospective analysis of etiology and outcome of preterm labor. J Obstet Gynecol India 57: 48-52.
- Sanborn BM, Ku CY, Shlykov S, Babich L (2005) Molecular signaling through G-protein-coupled receptors and the control of intracellular calcium in myometrium. J Soc Gynecol Investig 12: 479-487.
- Bernal AL (2003) Mechanisms of labor-biochemical aspects. BJOG 110: 39-45.
- MacIntyre DA, Tyson EK, Read M, Smith R, Yeo G, et al. (2007) Contraction in human myometrium is associated with changes in small heat shock proteins. Endocrinology 149: 245-252.
- Lamont RF (2003) The development and introduction of anti‐oxytocic tocolytics. BJOG 110: 108-112.
- Cabrol D, Gillett J, Madelenat P (2001) Treatment of preterm labor with the oxytocin antagonist Atosiban: A double-bind, randomized, controlled comparison with salbutamol. Eur J Obstet Gynecol Reprod Biol 98: 177-185.
- Ashraf AA, Kamal Sayed AK, El Sherif L, Loutfi GO, Ahmed AMM, et al. (2019) Systematic review and meta-analysis of randomized controlled trials of atosiban versus nifedipine for inhibition of preterm labor. Int J Gynaecol Obstet 145: 139-148.
- Yu Y, Yang Z, Wu L, Zhu Y, Guo F (2020) Effectiveness and safety of atosiban versus conventional treatment in the management of preterm labor. Taiwan J Obstet Gynecol 59: 682-685.
- Grzesiak M, Oszukowski ZG, Kocyłowski R, Suliburska J, Oszukowski P, et al. (2018) Oxidative Stress in Women Treated with Atosiban for Impending Preterm Birth. Oxid Med Cell Longev 2018: 3919106.
- Esplin MS, O’Brien E, Fraser A, Kerber RA, Clark E, et al. (2008) Estimating recurrence of spontaneous preterm delivery. Obstet Gynecol 112: 516-523.
- Guillermo V, Sanchez-Ramos7 L, Romero R, Silver HM, Koltun WD, et al. (2000) Maintenance treatment of preterm labor with the oxytocin antagonist atosiban. The Atosiban PTL-098 Study Group. Am J Obstet Gynecol 182: 1184-1190.
- Tsatsaris V, Carbonne B, Cabrol D (2004) Atosiban for Preterm Labor. Drugs 64: 375-382.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Pathology and Toxicology Research
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- Journal of Carcinogenesis and Mutagenesis Research (ISSN: 2643-0541)

